Difficult conversations with the seriously ill
“We will have to talk about dying during COVID-19 but the challenge for us is how to do this with confidence and empathy and have these conversations with openness, compassion and dignity.”

These are the words of Dr Lara Mitchell (pictured right), a Consultant in Medicine for the Elderly (Queen Elizabeth University Hospital, Glasgow; NHS Greater Glasgow & Clyde). She is also Chair of the British Geriatrics Society Cardiovascular Special Interest Group and a BJC editorial board member. To give healthcare professionals a visual approach to support with difficult conversations around dying with compassion and honesty, Dr Mitchell has produced resource materials with Open Change, an educational design company.
A structured way that healthcare professionals can deliver these conversations is through a red map framework, compiled by Edinburgh colleagues. This is outlined in her video (see end of section for details).
She describes the components as:
- Ready – First I would say are you ready, have you put the joblist down, are you in a space where you are ready to do this? If talking to the relatives, check where they are, ask if someone is with them and verify if they are OK to proceed? If it’s the patient, ask “Can we talk about your care?”
- Expect – It’s always a good idea to check understanding. You need to know where they are at because if they are on a different page, you may have more explaining to do. For example ask “what do you know”/“want to ask”?
- Diagnosis – Let them know what we know/ what we don’t know. Be open and honest.
- Matters – really find out what matters to them? It may be to see a certain family member / their dog. Or something else altogether. Ask. Listen.
- Action – Use clear language to let them know what can help / what will not help.
- Plan – Make a plan so everyone knows what to do and document this clearly in the notes.
“For many of us we may feel out of our comfort zone…..at medical school we are taught all the lifesaving treatments and how we can make people better, cure them from whatever ailment they have. Yet, still, I think we struggle with the concept that caring for the dying and providing a good death for someone is equally as important,” says Dr Mitchell.
The pandemic is a crisis that’s moved the conversation on and there is a sense of urgency when patients are presenting to hospital. “Many of us are going to be doing this over the next few months and it is really important that you are able to debrief with a colleague and check in with yourself about how you are. My colleague and I do this regularly and it helps to share the experience,” Dr Mitchell concludes.
Dr Mitchell’s full presentation ‘Difficult conversations – we need to talk about dying’ is available in two versions on the NHS Education for Scotland site TURAS Learn:
- For healthcare workers, visit https://learn.nes.nhs.scot/741/quality-improvement-zone for information. The seven-minute presentation covers framework, concepts and phrases to support honest and compassionate conversations and is available at: https://vimeo.com/404554818
- Medical and nursing staff can find information at the COVID End of Life and Palliative Care section of TURAS Learn at: https://learn.nes.nhs.scot/28406/coronavirus-covid-19/palliative-and-end-of-life-care, which includes a 13-minute presentation as above but with a principles of treatment section.
Almost half COVID-19 deaths are in those 80 years and over
A comparison analysis of COVID-19 deaths from seven major countries (7MM*) shows disproportionate rates among older age groups according to GlobalData, a US data and analytics company.
A comparison of COVID-19 mortality data by age groups from the 7MM i.e. US, France, Germany, Italy, Spain, China, South Korea and Singapore, found that the proportions of deaths vary by four different age groups: under 60 years, 60–69 years, 70–79 years, and 80 years and older (figure 1).
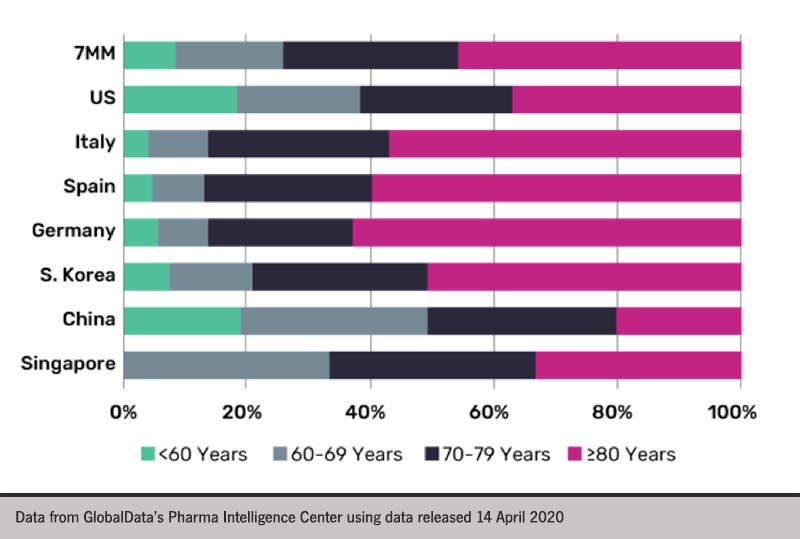
Dr Nanthida Nanthavong, an epidemiologist at GlobalData, commented: “In the 7MM, the average proportion of deaths by age group highlights that men and women over the age of 60 years account for the majority of COVID-19 deaths and nearly half of all COVID-19 deaths are among men and women ages 80 years and older.
For all markets except China, the highest proportion of deaths are among the 80 years and older age group. In China, the proportion of deaths among men and women over 80 years accounts for only 20% of all COVID-19 deaths.
Dr Nanthavong continued: “The discrepancy between the proportions in China compared with other markets may be attributed to the limited availability of epidemiological data on COVID-19 in China, including data on age and sex of the deceased”.
Due to these limitations in China, “the actual numbers of COVID-19 confirmed cases and deaths are most likely underreported. These concerns are also applicable to other markets, especially in an early phase of the outbreak where reliable data are limited” he concluded.
COVID-19 Bulletin 1:
COVID-19 and diabetes
COVID-19 and heart failure
COVID-19 and primary care
COVID-19 in cancer patients
COVID-19 and cardiovascular disease
COVID-19 and respiratory medicine
Round up of COVID-19 e-learning, apps and websites
