Heart failure with preserved ejection fraction (HFpEF) is a common concern in the medical field due to its prevalence in an ageing western population. HFpEF is associated with significant morbidity and mortality not dissimilar to heart failure (HF) with reduced ejection fraction. N-terminal pro-B-type natriuretic peptide (NT-proBNP) levels and echocardiography are the guideline diagnostic indicators of HF and their use is being examined in this study, with the aim to consider NT-proBNP thresholds performance as a rule-out test.
The current National Institute for Health and Care Excellence (NICE) and European guidelines recommend a single NT-proBNP threshold of >400 ng/L and >125 ng/L, respectively, to trigger echocardiographic assessment of HF in the outpatient setting. NT-proBNP levels are known to increase with age and worsening renal function. Unsurprisingly, a single threshold significantly increases demand for echocardiography. NT-proBNP measurements and echocardiograms performed within six months of each other were included for 469 patients with suspected HF.
A significant relationship between NT-proBNP levels and diastolic dysfunction was established. NT-proBNP levels and age are significant predictors of diastolic dysfunction in uni-variant (odds ratio 1.251, 95% confidence interval [CI], p<0.001) and multi-variant analysis (odds ratio 1.174, 95%CI, p=0.002). High negative-predictive values (NPVs) were obtained in severe diastolic impairment with the NPV being 95% at the European NT-proBNP cut-off of 125 ng/L, 95% at the NICE cut-off of 400 ng/L, 93% at 1,000 ng/L and 92% at 2,000 ng/L.
There is a significant association between NT-proBNP and diastolic dysfunction. NT-proBNP and age can predict diastolic dysfunction, and age can predict NT-proBNP levels, thus, these variables should be considered when considering referral for an echocardiogram. Most importantly, at higher NT-proBNP cut-offs the NPVs remain above 90% suggesting that different thresholds for subpopulations could yield a more effective strategy and mitigate the increased demand for echocardiography.
Introduction

In recent years heart failure with preserved ejection fraction (HFpEF) has become a research priority, since despite having a preserved ejection fraction (EF), it is still associated with mortality and survival rates similar to heart failure with a reduced ejection fraction (HFrEF).1 Historically, the interest in HFpEF stems from the collaboration of two areas of research. Studies found that diastolic left ventricular (LV) dysfunction contributed to myocardial hypertrophy.2,3 Shortly after, HFpEF was found to be an adjunct in heart failure (HF) trials, examining the usefulness of angiotensin-converting enzyme (ACE) inhibitors in remodelling of the LV post-infarct.4,5 Fast forward another few years and cases of HFpEF are on the increase, with indications that this could be the most common type of HF in the next decade.6 Currently, HFpEF makes up more than 50% of cases in those over the age of 65 years.7 As it is becoming more prevalent it is important to not only diagnose HF, but to classify the form using reliable investigations. The requirement of objective evidence of HF is echoed in both European Society of Cardiology (ESC) and National Institute for Health and Care Excellence (NICE) guidelines.8,9 The assessment of N-terminal pro-B-type natriuretic peptide (NT-proBNP) levels and an echocardiogram are the recommended tools to aid HF diagnosis, therefore, it is important to explore this specifically for HFpEF.10 As well as NT-proBNP levels, other factors such as gender and age can impact on diastolic function. Age, renal function, atrial arrhythmias, body mass index and diastolic dysfunction can influence NT-proBNP levels. In fact, having age-related NT-proBNP thresholds has shown encouraging results in the diagnosis of acute HF. In the recent ICON-RELOADED (International Collaborative of NT-proBNP-Re-evaluation of Acute Diagnostic Cut-Offs in the Emergency Department) study the following age-specific NT-proBNP cut-offs were used: 450 pg/ml for those under 50 years old, 900 pg/ml for those aged 50 to 75, and 1,800 pg/ml for those over 75 years of age. The negative-predictive values (NPVs) for each cut-off group were 99.7%, 96.9% and 85.1%, respectively, highlighting that adopting age-related cut-offs should be explored further.11,12
In July 2020, the British Heart Foundation (BHF) reported that 48,000 people had been diagnosed with HF in Scotland.13 While these statistics do not differentiate between HFrEF and HFpEF, HF is a cause for concern, particularly since the pathophysiological mechanism of HFpEF is still ambiguous. Moreover, the treatments for HFrEF and HFpEF are different, thus, further emphasising the importance of a specific diagnosis. In HFrEF, medication such as sacubitril/valsartan has proven to be beneficial, however, the results from the recent PARAGON-HF (Prospective Comparison of ARNI with ARB Global Outcomes in HF with Preserved Ejection Fraction) trial show this drug has no effect in those with an EF over 45%.14,15 Current treatment for HFpEF will exclusively alleviate symptoms, but has no effect on mortality and morbidity. It is only very recently that sodium-glucose cotransporter 2 (SGLT2) inhibitors, such as empagliflozin, have proven beneficial in reducing cardiac death and hospitalisations for HFpEF. In the 2021 EMPEROR-Preserved (Empagliflozin Outcome Trial in Patients With Chronic Heart Failure With Preserved Ejection Fraction) study, cardiovascular death or hospitalisation occurred in 13.8% of HFpEF patients taking empagliflozin versus 17.1% in the placebo group with a p value of <0.001 to support the significance of this. While this is promising, more research is essential.16 The NICE guidelines state a NT-proBNP cut-off of 400 ng/L, as at lower levels, HF is unlikely. They suggest that anyone with a NT-proBNP between 400 and 2,000 ng/L must have an echo within six weeks. For those with a level exceeding 2,000 ng/L, the echo should be within two weeks, as very high levels of NT-proBNP are associated with poor outcomes.9 When assessing the sensitivity and specificity of NT-proBNP to diagnose diastolic dysfunction, high values have been obtained. However, the peptide threshold was lower than in the NICE guidelines. Celik et al. (2012) found a 90% sensitivity and 73% specificity at a NT-proBNP cut-off of 269.1 ng/L.17 An earlier study demonstrated a sensitivity of 91% and specificity of 86% at a 55 ng/L cut-off.18 The use of NT-proBNP as a rule-in and rule-out test for diastolic dysfunction has also been explored, with high positive-predictive values (PPVs) and NPVs being found, respectively (PPV 84%, NPV 94%).19 Nevertheless, there are currently no studies that have explored higher NT-proBNP thresholds and how these would impact on sensitivity, specificity, PPVs and NPVs.20
Taking everything into account, the association between NT-proBNP and diastolic function needs to be explored to aid the diagnosis of HFpEF. Second, NT-proBNP, gender and age as predictors of diastolic dysfunction will be considered, as these are common confounding variables in a HFpEF diagnosis. Predictors of NT-proBNP levels will also be assessed. Finally, NT-proBNP as a rule-out test for HFpEF will be assessed. This is especially important since the demand on echocardiography services is currently greater than at any time before, due to the impact of the COVID-19 pandemic on the provision of cardiac services.
Materials and method
The study population comprised patients in the Dumfries and Galloway region with suspected HF, using data archived from 2014 to 2016, as these were readily available. Data obtained included patient gender, age, NT-proBNP measurements, and echocardiographic parameters (LV systolic function and degree of diastolic dysfunction). NT-proBNP levels were provided by the biochemistry laboratory at Dumfries and Galloway Royal Infirmary (DGRI), with the remaining information obtained from the institutional case note system. The initial sample size was 1,000. However, when NT-proBNP levels and echocardiograms were not performed within six months of each other, these patients were excluded. Further exclusion criteria included those with a reduced EF as measured by Simpsons (49% or less), atrial fibrillation and valve disease. Consequently, the final sample size is 469 patients (females n=262, males n=207) with an age range of 26 to 94 years.
Diastolic function was not always classified in accordance with the recommended guidelines. Consequently, diastolic function was re-assessed using the British Society of Echocardiography (BSE) guidelines for all the echocardiograms included in this study. During the original scans an E/A pattern was obtained. However, an E/A ratio was not always calculated, therefore, for consistency, this ratio and deceleration time (DT) were calculated for every echocardiogram included in this study. The software has also provided velocities for the mitral annulus (e′), both medially and laterally, to yield an E/e′ ratio. The size of the left atrium (LA) was also measured in M-mode at the level of the aortic valve.
Statistical Package for the Social Sciences (SPSS) version 26 was used for statistical analysis. A Chi-squared test was carried out to determine if there was an association between NT-proBNP levels and diastolic function (all grades). Generalised linear analysis was used to predict the effects of NT-proBNP, gender and age on diastolic dysfunction and the effects of gender and age on NT-proBNP levels. Finally, multiple two-by-two tables were created in SPSS for each NT-proBNP cut-off comparing normal versus grade 1 diastolic dysfunction and normal versus grade 2 and 3 diastolic dysfunction. An extra cut-off of 125 ng/L was added at this point in keeping with European guidance, as they have demonstrated lower NT-proBNP levels in primary care.8 These tables were then used to input data into VassarStats to obtain sensitivity and specificity results.
Results
Baseline characteristics
A total of 469 patients were included in this study. Half of the patients (52.2%) had a degree of diastolic impairment. Males accounted for 44.1% (n=207) of the total study population and 55.9% (n=262) were female. No males in this study had grade 3 diastolic dysfunction. The mean age was 71.6 years and 50–75 years was the biggest age cohort. The average age for grade 2 and grade 3 diastolic dysfunction was 76 years old. No grade 3 diastolic dysfunction was observed in those under 50 years. NT-proBNP levels were above the local and NICE 400 ng/L cut-off in 39.6% of cases. All grade 3 patients had a NT-proBNP of >2,000 ng/L. Normal diastolic function was observed in 48% of cases. Grade 1 diastolic impairment was observed in 46.1% of cases, 5.1% for grade 2 and only four patients had grade 3 diastolic impairment, meaning grades 2 and 3 were amalgamated and reclassified as severe impairment for statistical analysis. Full characteristics are shown in table 1.
Table 1. Baseline characteristics
| Normal diastolic function | Grade 1 diastolic function | Grade 2 diastolic function | Grade 3 diastolic function | All patients | |
|---|---|---|---|---|---|
| N (%) | 225 (48) | 216 (46.1) | 24 (5.1) | 4 (0.9) | 469 (100) |
| Gender, n (%) | |||||
| Male | 110 (53.1) | 88 (42.5) | 9 (4.4) | 0 (0) | 207 (44.1) |
| Female | 115 (43.9) | 128 (48.9) | 15 (5.7) | 4 (1.5) | 262 (55.9) |
| Age, years | |||||
| Mean ± SD | 42 ± 7.9 | 45 ± 6.3 | 76 ± 7.5 | 76 ± 12.6 | 71.57 ± 10.7 |
| <50, n (%) | 10 (66.7) | 5 (33.3) | 0 (0) | 0 (0) | 15 (3.2) |
| 50–75, n (%) | 151 (55.5) | 108 (39.7) | 12 (4.4) | 1 (0.4) | 272 (58.0) |
| >75, n (%) | 64 (35.2) | 103 (56.6) | 12 (6.6) | 3 (1.7) | 182 (38.8) |
| NT-proBNP, ng/L | |||||
| Median (IQR) |
239 (123–499) |
323 (164–769) |
501 (311–2,350) |
4,320 (2,291–5,855) |
302 (154–649) |
| NT-proBNP 0–400, n (%) | 152 (53.7) | 123 (43.5) | 8 (2.8) | 0 (0) | 283 (60.3) |
| 400–1000, n (%) | 45 (42.5) | 53 (50) | 8 (7.5) | 0 (0) | 106 (22.6) |
| 1,000–2,000, n (%) | 20 (48.8) | 20 (48.8) | 1 (2.4) | 0 (0) | 41 (8.7) |
| > 2,000, n (%) | 8 (20.5) | 20 (51.3) | 7 (18) | 4 (10.3) | 39 (8.3) |
| Key: IQR = interquartile range; NT-proBNP = N-terminal pro-B-type natriuretic peptide; SD = standard deviation | |||||
NT-proBNP results
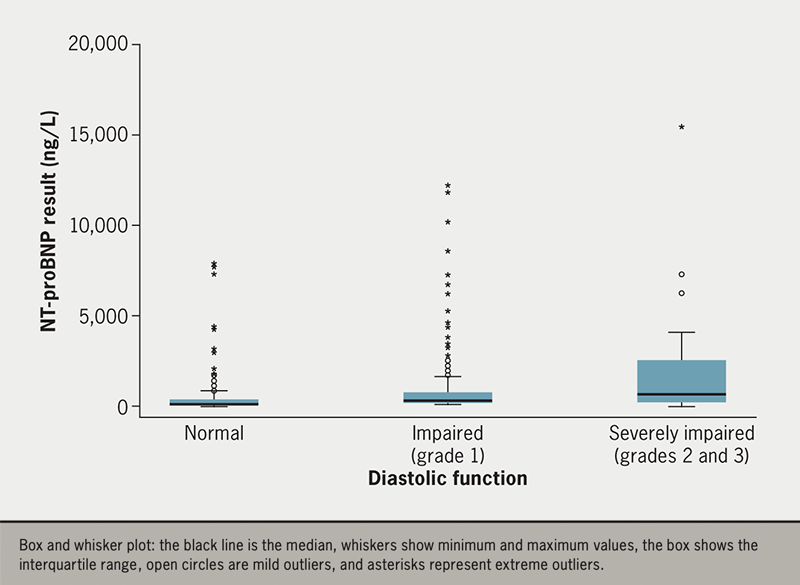
As diastolic function worsens, the median and interquartile range (IQR) increase. For those with normal diastolic function, the median NT-proBNP was 239 ng/L and the IQR was 123–499 ng/L. In grade 1 impairment the median NT-proBNP level was 323 ng/L (IQR 164–769 ng/L) and for severe impairment (grades 2 and 3) the median was 564 ng/L (IQR 352–2,237 ng/L) (figure 1).
Predictors of diastolic function and NT-proBNP levels
There is a significant association between NT-proBNP and all grades of diastolic function with a p value of <0.001. In the single and multi-variate predictor models NT-proBNP and age were significant predictors of diastolic function. In the multi-variate analysis, age is the strongest significant predictor of diastolic dysfunction (odds ratio [OR] 1.174, 95% confidence interval [CI] 1.061 to 1.300, p=0.002). Increasing NT-proBNP levels and age are likely to be associated with increasing diastolic impairment. Gender is not a significant predictor of diastolic dysfunction (table 2).
Table 2. Predictors of diastolic function and N-terminal pro-B-type natriuretic peptide (NT-proBNP) levels
| Single predictor model | Multi-variate predictor model | |||
|---|---|---|---|---|
| Variable | Odds ratio (95%CI) | p value | Odds ratio (95%CI) | p value |
| Predictors of diastolic function | ||||
| NT-proBNP | 1.162 (1.099 to 1.229) | <0.001 | 1.128 (1.061 to 1.200) | <0.001 |
| Sex | 0.890 (0.798 to 0.993) | 0.36 | 0.915 (0.823 to 1.016) | 0.097 |
| Age | 1.251 (1.133 to 1.381) | <0.001 | 1.174 (1.061 to 1.300) | 0.002 |
| Predictors of NT-proBNP levels | ||||
| Sex | 0.841 (0.586 to 1.209) | 0.351 | 1.031 (0.702 to 1.515) | 0.876 |
| Age | 2.549 (1.796 to 3.161) | <0.001 | 1.639 (1.131 to 2.374) | 0.009 |
| Key: CI = confidence interval | ||||
Table 2 also shows that age is the strongest predictor of increased NT-proBNP levels in both the single and multi-variate models, and this is supported by significant p values of <0.0001 and 0.009, respectively (OR 2.549, 95%CI 1.796 to 3.1610; OR 1.639, 95%CI 1.131 to 2.374). In the single-predictor model, increased age is 2.5 times more likely at higher NT-proBNP levels and over one and a half times more likely in the multi-variate analysis. Gender is not a significant predictor of NT-proBNP levels.
NT-proBNP as a rule-out test for diastolic impairment
Table 3 shows the sensitivity, specificity, PPVs and NPVs for ESC and NICE guideline cut-offs. The probability that a negative result will not indicate grade 1 impairment is 61% at a NT-proBNP cut-off of 125 ng/L, 55% at 400 ng/L, 53% at 1,000 ng/L and 52% at 2,000 ng/L. For severe impairment, the NPVs are 95%, 95%, 93% and 92%, respectively.
Table 3. Sensitivity, specificity, positive-predictive value (PPV) and negative-predictive value (NPV) for European Society of Cardiology (ESC) and National Institute for Health and Care Excellence (NICE) guidelines
| All patients N=469 |
Impaired (grade 1) | Severe (grades 2 and 3) |
|---|---|---|
| Number of patients | 216 | 28 |
| All ages, cut-point 125 ng/L (ESC) | ||
| Sensitivity, % (95%CI) | 83.4 (77.6 to 88.0) | 89.2 (70.6 to 97.2) |
| Specificity, % (95%CI) | 25.0 (19.6 to 31.3) | 25.0 (19.6 to 31.3) |
| PPV | 0.52 | 0.13 |
| NPV | 0.61 | 0.95 |
| All ages, cut-point 400 ng/L (NICE) | ||
| Sensitivity, % (95%CI) | 43.3 (36.7 to 50.2) | 71.4 (51.1 to 86.0) |
| Specificity, % (95%CI) | 67.9 (61.3 to 73.8) | 67.9 (61.3 to 73.8) |
| PPV | 0.57 | 0.22 |
| NPV | 0.55 | 0.95 |
| All ages, cut-point 1,000 ng/L | ||
| Sensitivity, % (95%CI) | 18.9 (14.0 to 24.9) | 42.9 (25.0 to 62.6) |
| Specificity, % (95%CI) | 88.0 (82.8 to 91.8) | 88.0 (82.8 to 91.8) |
| PPV | 0.60 | 0.31 |
| NPV | 0.53 | 0.93 |
| All ages, cut-point 2,000 ng/L | ||
| Sensitivity, % (95%CI) | 9.22 (5.86 to 14.1) | 39.3 (22.1 to 59.3) |
| Specificity, % (95%CI) | 96.4 (92.8 to 98.3) | 96.4 (92.8 to 98.3) |
| PPV | 0.71 | 0.58 |
| NPV | 0.52 | 0.92 |
| Key: ACE = angiotensin-converting enzyme; ARB = angiotensin-receptor blocker | ||
NT-proBNP as a rule-in test for diastolic impairment
The PPVs demonstrate that as the NT-proBNP cut-point increases, the probability that a positive test will indicate grade 1 impairment increases. At a cut-point of 125 ng/L there is a 52% probability that a positive result will indicate grade 1 diastolic impairment, 57% at 400 ng/L, 60% at 1,000 ng/L and 71% at 2,000 ng/L. The same can be said for severe impairment, as there is a 13% probability at a cut-point of 125 ng/L, 22% at 400 ng/L, 31% at 1,000 ng/L and 58% at 2,000 ng/L (table 3).
Discussion
The use of NT-proBNP threshold levels to diagnose diastolic dysfunction is widely debated and a point of research interest given the increasing prevalence of HFpEF.21 This study demonstrates that there is a significant relationship between NT-proBNP and diastolic function. Furthermore, as diastolic impairment worsens, the median NT-proBNP levels increase, which is in keeping with current literature.22 However, in general, the NT-proBNP levels in HFpEF are thought to be lower than HFrEF.23–25 The median NT-proBNP level in this study for those with grade 1 diastolic impairment is 325 ng/L, which is below the NICE guidelines’ threshold for echocardiography, as HF is deemed unlikely. However, grade 1 impairment is common in older age and over the age of 60 years. In the absence of any other indicators of diastolic impairment, this would be considered normal.26 In this case, 56.6% of those with grade 1 impairment were over 75 years old and 39.7% were aged between 50 and 75 years. In younger patients, the early diastolic phase (E) of ventricular filling is more dominant than the late phase (A) as the pressures in the apex of the LV are lower than the base. However, as we age, collagen continues to amass in the myocardium, meaning relaxation of the LV becomes slow and the isovolumetric relaxation phase is lengthened. Since this predominately affects the early diastolic phase (E), there is a compensatory increase of filling in the late phase (A), resulting in a reversed E/A pattern (grade 1 impairment).27 Despite this, the mean age for grade 1 impairment in this study was 45 years old, suggesting that diastolic impairment could be influenced by other factors, such as renal impairment.
In those with the most severe diastolic impairment (grade 3), the median NT-proBNP level is 4,320 ng/L (IQR 3,278–5,361 ng/L), and for grade 2 the median is 501 ng/L (IQR 325–1,916 ng/L). These results support the fact that high NT-proBNP levels are associated with worsening diastolic function. Moreover, the results of this study show that NT-proBNP is the biggest predictor of diastolic dysfunction in single variant analysis (table 2). In HFpEF, the LV wall thickness increases while the LV diameter reduces. Laplace’s law of LV wall stress states as wall tension increases so does the LV diameter, but LV thickness decreases. Consequently, since NT-proBNP is released in response to wall stress, this peptide is thought to have little effect on diastolic function. This also explains why NT-proBNP levels are generally lower in HFpEF versus HFrEF.28,29
In the multi-variant analysis, age was the strongest predictor of diastolic function (table 2). In a healthy population the E/e′ ratio and e′ velocity was found to be significantly greater in females versus males, and the deceleration time (DT) of males was longer than females, indicating that there are sex differences.30
It has already been remarked that NT-proBNP levels increase with age, even in healthy individuals, and that changes in cardiac vasculature can prompt the release of this peptide to compensate.31 This study supports the premise that age is the most significant predictor of NT-proBNP levels in both uni- and multi-variant analysis (table 3). In fact, recent research suggests NT-proBNP could be the best predictor of biological age, and it is associated with all-cause mortality, even in those without HF.32 Once again, gender was not found to be a significant predictor of NT-proBNP levels, in both uni- and multi-variant analysis.
Pan et al. (2017) have shown that there are various factors that can influence NT-proBNP, and, as a result of this, the sensitivity of this peptide to diagnose HF is thought to be high and specificity low.33 However, in this current study, as the NT-proBNP cut-offs for all age groups increased, sensitivity decreased for impaired and severely impaired cohorts, respectively (table 3). In this study, while higher sensitivities would be desirable, it would mean additional unnecessary echocardiograms in a service already under significant demand. Across health boards echo cardiology services are under extreme pressure, made worse by the COVID-19 pandemic. When Scotland went into lockdown, clinic numbers had to be reduced, and locally this meant that by the end of May 2020 the number of outpatient clinic reviews had reduced by up to 74%. Now that services have resumed there is a massive backlog of patients, and it is anticipated that post-COVID, the potential cardiovascular impact of COVID infections will increase the pressure further.34
The specificity has, however, increased in this study as cut-points increased for ESC and NICE guidelines, with high specificity being found at the highest cut-offs. Specificity indicates the probability that the screening test will correctly detect those without diastolic impairment, while avoiding false positives.35 At the 1,000 ng/L and 2,000 ng/L cut-offs, the specificity was 88% and 96.4%, respectively, for both impaired and severely impaired cohorts. These high specificities indicate that higher cut-off points could be created safely, while managing the pressure on echocardiography services.
The most important results of this study are the NPVs, if local and national protocols are to be altered. To increase the current NT-proBNP cut-off of 400 ng/L for an echocardiogram we must be confident that a large percentage of the population will not be missed. The NPVs for diastolic dysfunction are low, however, grade 1 dysfunction can be a normal finding in the elderly. Furthermore, grade 1 dysfunction does not require medical intervention and is thought to manifest from an isolated dysfunction of early diastolic filling. It does not influence LV compliance, unlike more severe dysfunction.36 Consequently, it is the NPVs for severe impairment that are of interest. When the ESC and NICE cut-offs were adopted, the NPVs for severe diastolic impairment were 95% at 125 ng/L, 95% at 400 ng/L, 93% at 1,000 ng/L and 92% at 2,000 ng/L.
When the cut-off was 125 ng/L as per the ESC, 225 patients (48%) had normal diastolic function, and an echocardiogram did not need to be performed. At this cut-off, there was a 95% probability that severe diastolic impairment was not present with a sensitivity of 89.2%. When this NT-proBNP cut-off is increased to 400 ng/L, as per NICE guidelines, the NPV does not alter, meaning that even when you scan less people you can still obtain a 95% probability that the patients will not have severe impairment. At the higher cut-offs of 1,000 ng/L and 2,000 ng/L, the NPVs are still high when assessing severe impairment with increasing specificity, 88% and 96.4%, respectively. High NPVs were also found in a recent meta-analysis exploring the association of NT-proBNP and diastolic dysfunction in HFpEF patients, but not to the same degree as this current study.20 Importantly, this study has produced the highest NPVs when higher NT-proBNP thresholds are used, in comparison to current literature. However, this could be due to a smaller sample of those with severe diastolic dysfunction in this study.
Consequently, the greatest limitation of this study was the small cohort of patients with grade 2 and 3 diastolic impairment, making up only 5.97% of the total population. When interpreting echocardiographic parameters, additional factors should also be considered. For example, E wave velocity can be influenced by factors such as filling pressure, age, and presence of valve disease, with overall mitral inflow being less valuable if comorbidities, such as coronary artery disease (CAD), are present. CAD can also interfere with other tissue Doppler measurements, as can age-associated annular calcification. Caution should also be taken when interpreting the E/e′ pattern, as this only interprets early diastole, meaning global diastolic dysfunction is not assessed.37 Increased LA size does not necessarily represent diastolic dysfunction. It can be affected by atrial arrhythmias, severe mitral valve disease and chronic volume overload from chronic kidney disease.38,39 It is proposed that echocardiographic parameters measured in diastolic phase are not innate, and in fact emulate changes in intravascular volume. Consequently, filling pressures are more important.39 In this study, LA size was measured in M-mode, which may be considered outdated, volumetric assessment should be used in future studies. Renal failure was not taken into account, and this is a major factor affecting NT-proBNP levels and diastolic dysfunction.
Conclusion
This study showed that NT-proBNP levels significantly predict diastolic dysfunction (p<0.001). Age is a significant predictor of diastolic function with increasing age being associated with increasing diastolic dysfunction in uni- and multi-variate analyses. Age is also a significant predictor of NT-proBNP levels in both single and multi-variable predictor models. Consequently, this variable should be taken into consideration when developing guidelines for HFpEF diagnosis. Most importantly, this study showed that the current ESC and NICE NT-proBNP cut-offs could be increased without compromising clinical performance. Furthermore, as well as adopting a local HF policy with higher NT-proBNP cut-offs, age-adjusted thresholds could also be considered. By doing so, the number of echo referrals for query HF would be significantly reduced. Furthermore, as renal status is thought to influence NT-proBNP levels, age-adjusted thresholds could account for this. The PRIDE (N-terminal Pro-BNP Investigation of Dyspnea in the Emergency department) study found that when appropriate age cut-offs were used, the sensitivity and specificity of NT-proBNP for those with normal kidney function were 85% and 88%, respectively.40 However, as the most recent studies looking at age cut-offs have had low numbers of HF patients, this needs to be explored further.
Key messages
- Heart failure with preserved ejection fraction (HFpEF) cases are rising with N-terminal pro-B-type natriuretic peptide (NT-proBNP) and echocardiography being the key diagnostic indicators in clinical practice. The current single threshold for NT-proBNP is low, resulting in a vast number of inappropriate echocardiography referrals, overwhelming an already stretched service
- High negative-predictive values (NPVs) indicate that the current NT-proBNP threshold could be increased without compromising clinical performance
- By increasing the NT-proBNP threshold there would be a dramatic reduction in echocardiography referrals and help alleviate the strain
Conflicts of interest
None declared.
Funding
None.
Study approval
This study involved human data and was approved by the Research and Development department at Dumfries and Galloway Royal Infirmary.
Acknowledgements
We would like to thank Fiona Ross and Mieke Mckend who helped extract echo data.
References
1. Yoon S, Eom GH. Heart failure with preserved ejection fraction; present status and future directions. Exp Mol Med 2019;51:1–9. https://doi.org/10.1038/s12276-019-0323-2
2. Sanderson EJ, Gibson GD, Brown JD, Goodwin FJ. Left ventricular filling in hypertrophic cardiomyopathy. An angiographic study. Heart 1997;39:661–70. https://doi.org/10.1136/hrt.39.6.661
3. Hanrath P, Mathey DG, Siegert R, Blefeld W. Left ventricular relaxation and filling pattern in different forms of left ventricular hypertrophy: an echocardiographic study. Am J Cardiol 1980;45:15–23. https://doi.org/10.1016/0002-9149(80)90214-3
4. Aronow WS, Kronzoni I. Effect of enalapril on congestive heart failure treated with diuretics in elderly patients with prior myocardial infarction and normal left ventricular ejection fraction. Am J Cardiol 1993;71:602–04. https://doi.org/10.1016/0002-9149(93)90520-M
5. Carson P, Johnson G, Fletcher R, Cohn J. Mild systolic dysfunction in heart failure (left ventricular ejection fraction >35%): baseline characteristics, prognosis, and response to therapy in the Vasodilator in Heart Failure Trials (V-HeFT). J Am Coll Cardiol 1996;27:642–9. https://doi.org/10.1016/0735-1097(95)00503-X
6. Owan ET, Hodge OD, Herges MR, Jacobsen JS, Roger LV, Redfield MM. Trends in prevalence and outcome of heart failure with preserved ejection fraction. N Engl J Med 2006;355:251–9. https://doi.org/10.1056/NEJMoa052256
7. Upadhya B, Kitzman WD. Heart failure with preserved ejection fraction: new approaches to diagnosis and management. Clin Cardiol 2020;43:145–55. https://doi.org/10.1002/clc.23321
8. McDonagh TA, Metra M, Adamo M et al. 2021 ESC guidelines for the diagnosis and treatment of acute and chronic heart failure: developed by the Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC) with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur Heart J 2021;42:3599–726. https://doi.org/10.1093/eurheartj/ehab368
9. National Institute for Health and Care Excellence (NICE). Chronic heart failure in adults: diagnosis and management. London: NICE, 2018. Available from: https://www.nice.org.uk/guidance/ng106/chapter/Recommendations
10. Mohammad AA. NICE heart failure guidelines: the diagnostic algorithm in practice, what is the next step? Heart 2020;106:1579–85. https://doi.org/10.1136/heartjnl-2020-317450
11. Lee KK, Doudesis D, Anwar M et al. Development and validation of a decision support tool for the diagnosis of acute heart failure: systematic review, meta-analysis, and modelling study. BMJ 2022;377:e068424. https://doi.org/10.1136/bmj-2021-068424
12. Januzzi JL, Chen-Tournoux AA, Christenson RH et al. N-terminal pro-B-type natriuretic peptide in the emergency department: the ICON-RELOADED study. J Am Coll Cardiol 2018;71:1191–200. https://doi.org/10.1016/j.jacc.2018.01.021
13. British Heart Foundation. Heart statistics. Available at: https://www.bhf.org.uk/statistics [accessed 23 October 2020].
14. Solomon SD, McMurray JJ, Anand IS et al. Angiotensin-neprilysin inhibition in heart failure with preserved ejection fraction. N Engl J Med 2019;381:1609–20. https://doi.org/10.1056/NEJMoa1908655
15. Lelonek M. Heart failure with preserved ejection fraction after the PARAGON-HF trial results: current knowledge and future directions. Kardiol Pol 2020;78:1199–205. https://doi.org/10.33963/KP.15639
16. Anker SD, Butler J, Filippatos G et al. Empagliflozin in heart failure with a preserved ejection fraction. N Engl J Med 2021;385:1451–61. https://doi.org/10.1056/NEJMoa2107038
17. Celik A, Koc F, Kadi H et al. Relationship between red cell distribution width and echocardiographic parameters in patients with diastolic heart failure. Kaohsiung J Med Sci 2012;28:165–72. https://doi.org/10.1016/j.kjms.2011.06.024
18. Barragan A, Lacalzada J, Rosa A et al. Relationship between slightly elevated NT-proBNP and alterations in diastolic function detected by echocardiography in patients without structural heart disease. Int J Cardiol 2008;129:430–2. https://doi.org/10.1016/j.ijcard.2007.06.097
19. Tschope C, Kasner M, Westermann D, Gaub R, Poller CW, Schulthesis PH. The role of NT-proBNP in the diagnostics of isolated diastolic dysfunction: correlation with echocardiographic and invasive measurements. Eur Heart J 2005;26:2277–84. https://doi.org/10.1093/eurheartj/ehi406
20. Remmelzwaal S, Ballegooijen JA, Schoonmade JL et al. Natriuretic peptides for the detection of diastolic dysfunction and heart failure with preserved ejection fraction – a systematic review and meta-analysis. BMC Med 2020;18:290. https://doi.org/10.1186/s12916-020-01764-x
21. Toth PP, Gauthieric D. Heart failure with preserved ejection fraction: disease burden for patients, caregivers, and the health-care system. Postgrad Med 2021;133:140–5. https://doi.org/10.1080/00325481.2020.1842621
22. Turkoglu IE, Cicekdag KCE. Heart failure with preserved ejection fraction, atrial fibrillation, and increased NTproBNP levels. Herz 2021;46(suppl 2):191–7. https://doi.org/10.1007/s00059-020-04981-5
23. Kang HS, Park JJ, Choi JD et al. Prognostic value of NT-proBNP in heart failure with preserved versus reduced EF. Heart 2015;101:1881–8. https://doi.org/10.1136/heartjnl-2015-307782
24. Kashara S, Sakata Y, Nochioka K et al. Comparable prognostic impact of BNP levels among HFpEF, borderline HFpEF and HFrEF: a report from the CHART-2 study. Heart Vessels 2018;33:997–1007. https://doi.org/10.1007/s00380-018-1150-4
25. Rorth R, Jhund SP, Yilmaz BM et al. Comparison of BNP and NT-proBNP in patients with heart failure and reduced ejection fraction. Circ Heart Fail 2020;13:e006541. https://doi.org/10.1161/CIRCHEARTFAILURE.119.006541
26. British Echocardiographic Society (BSE). A guideline protocol for the echocardiographic assessment of diastolic dysfunction. London: BSE, 2013. Available from: https://www.bsecho.org/common/Uploaded%20files/Education/Protocols%20and%20guidelines/Diastolic%20dysfunction.pdf [accessed 13 November 2020].
27. Henein YM, Lindqvist P. Diastolic function assessment by echocardiography: a practical manual for clinical use and future applications. Echocardiography 2020;37:1908–18. https://doi.org/10.1111/echo.14698
28. Veldhuisen JD, Linssen MCG, Jaarsma T et al. B-type natriuretic peptide and prognosis in heart failure patients with preserved and reduced ejection fraction. J Am Coll Cardiol 2013;61:1498–506. https://doi.org/10.1016/j.jacc.2012.12.044
29. Morais H, Feijao A, Pereira SV. Reference values of left ventricular diastolic function accessed by conventional and Doppler echocardiography in healthy Angolans: effect of age and gender. Authorea January 26 2021 [preprint]. https://doi.org/10.22541/au.161169022.23653445/v1
30. Hamada M, Shigematsu Y, Takezaki M, Ikeda S, Ogimoto A. Plasma levels of atrial and brain natriuretic peptides in apparently healthy subjects: effects of sex, age, and haemoglobin concentration. Int J Cardiol 2017;228:599–604. https://doi.org/10.1016/j.ijcard.2016.11.197
31. National Institute of Health (NIH). Heart health and aging. Available at: https://www.nia.nih.gov/health/heart-health-and-aging [accessed 6 November 2020].
32. Muscari A, Bianchi G, Forti P, Magalotti D., Pandolfi P, Zoli M. N-terminal pro B-type natriuretic peptide (NT-proBNP): a possible surrogate of biological age in the elderly people. GeroScience 2021;43:845–57. https://doi.org/10.1007/s11357-020-00249-2
33. Pan Y, Li D, Shan L, Wei M. NT-proBNP test with improved accuracy for the diagnosis of chronic heart failure. Medicine (Baltimore) 2017;96:e9181. https://doi.org/10.1097/MD.0000000000009181
34. Fersia O, Bryant S, Nicholson R et al. The impact of the COVID-19 pandemic on cardiology services. Open Heart 2020;7:e001359. https://doi.org/10.1136/openhrt-2020-001359
35. Trevethan R. Sensitivity, specificity, and predictive values: foundations, pliabilities, and pitfalls in research and practice. Front Public Health 2017;7:408. https://doi.org/10.3389/fpubh.2017.00307
36. Grant AD, Negishi K, Nigeshi T et al. Grading diastolic function by echocardiography: hemodynamic validation of existing guidelines. Cardiovasc Ultrasound 2015;13:28. https://doi.org/10.1186/s12947-015-0023-6
37. Maurer SM, Speuvack D, Burkhoff D, Krowzon I. Diastolic dysfunction. J Am Coll Cardiol 2004;44:1543–9. https://doi.org/10.1016/j.jacc.2004.07.034
38. Hee L, Nguyen T, Whatmough M et al. Left atrial volume and adverse cardiovascular outcomes in unselected patients with and without CKD. Clin J Am Soc Nephrol 2014;9:1369–76. https://doi.org/10.2215/CJN.06700613
39. Nagueh FS, Smiseth AO, Appleton PC et al. Recommendations for the evaluation of left ventricular diastolic function by echocardiography: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J Am Soc Echocardiogr 2016;29:277–314. https://doi.org/10.1016/j.echo.2016.01.011
40. Anwaruddin S, Lloyd-Jones DM, Baggish A et al. Renal function, congestive heart failure, and amino-terminal pro-brain natriuretic peptide measurement: results from the ProBNP Investigation of Dyspnea in the Emergency Department (PRIDE) study. J Am Coll Cardiol 2006;47:91–7. https://doi.org/10.1016/j.jacc.2005.08.051
