Cardiac pathology contributes to a significant proportion of emergency department (ED) attendances. Many could be managed as urgent outpatients and avoid hospital admission. We evaluated a novel rapid-access general cardiology clinic to achieve this, implemented during the COVID-19 pandemic.
We performed a retrospective review of baseline characteristics, investigations, final diagnoses, and 90-day safety (readmission, major adverse cardiovascular events [MACE], mortality) from electronic records and conducted a patient experience survey.
There were 216 ED referrals made between 1 June and 30 October 2020. The median time to review was two days (interquartile range 1–5). At 90 days, there were three (1.4%) re-presentations requiring admission, two (0.9%) MACE, and no deaths. There were 205 (95%) successfully managed without hospital admission. Among surveyed patients, 96% felt they had concerns adequately addressed in a timely manner.
In conclusion, our rapid-access cardiology clinic is a safe model for outpatient management of a range of cardiovascular presentations to the ED.
Introduction
Emergency department (ED) activity in the UK has steadily increased, with a 12% increase in attendances and 31% increase in downstream admissions between 2011/2012 and 2019/2020.1 Despite this, overall inpatient bed capacity has reduced.2 This was recognised in the National Health Service (NHS) Long-Term Plan (2019), which outlined an aim to reduce pressure on emergency hospital services.3 Ambulatory emergency care services were proposed as one of multiple measures to achieve this aim.
Presentations with suspected cardiac pathology contribute to a significant proportion of unplanned attendances to secondary care.4–6 Of these, some may require admission for further investigation, but others may be safely investigated in the outpatient setting. Rapid-access chest pain clinics are commonplace across the UK,7 but a similar approach for other cardiac presentations is less well-established.
Throughout the COVID-19 pandemic, there has been increased pressure to reduce inpatient admissions where possible, due to high levels of COVID-19 and non-COVID-19 admissions, and further reductions in inpatient capacity. In the initial phase of COVID-19, most outpatient activity was cancelled. In this context, it was recognised that some patients presenting with suspected cardiac pathology could be safely managed in an urgent outpatient setting. A consultant-led rapid-access cardiology clinic was established in our centre to address this. Here we evaluate the safety and efficacy of this service.
Method
This was a retrospective review of the safety and efficacy of a new clinical service. We have reported this in accordance with the Standards for Quality Improvement Reporting Excellence (SQUIRE 2.0) statement.8
The service
This consultant-led service was set up in a district general hospital serving a local population of 500,000 patients. When initially set up in April 2020, it was a seven-day service (Monday to Friday 0800–2000, Saturday to Sunday 0900–1200) allowing for same-day referrals from the ED. As the pandemic progressed, increasing inpatient workload and low weekend uptake meant the service was modified to a consultant-led morning clinic (Monday to Friday 0900–1300) with 30-minute scheduled patient consultation slots for rapid-access referrals.
Patients with suspected cardiac pathology were referred from the local ED via local electronic patient record system. Patients were booked into the next available clinic slot by administrative staff, although consultant triage was available if required. Referral criteria were kept broad to maximise the number of patients that could benefit from our clinic. The only criteria were:
- Ability to ambulate
- A negative severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) test
- Any cardiological presentation that did not require urgent inpatient treatment.
Of note, a separate established ambulatory heart failure service already existed so heart failure patients were not included in our cohort.
Clinics were carried out in the outpatient area of the cardiology department. There were facilities to allow basic observations, blood tests, 12-lead electrocardiograms (ECGs), and bedside echocardiograms to be performed for all presenting patients. There was some provision of same-day formal echocardiography and exercise treadmill tests, and patients could be dispensed with ambulatory blood pressure and rhythm monitoring devices. Patients could be referred for further investigations (echocardiograms, computed tomography [CT], magnetic resonance imaging [MRI]) from clinic, though this was not necessarily a same-day service. Admission from clinic was possible as the cardiology outpatient area was located adjacent to a 16-bed cardiac care unit and 28-bed cardiology ward.
Data collection
Two authors (BB, PTT) retrospectively reviewed contemporaneous documentation in the electronic patient record. We collected data on baseline demographics (age, gender, cardiovascular risk factors), referral details (date of referral, date seen in clinic, reason for referral), investigations performed in clinic, outcomes from clinic (further investigations, follow-up, admission from clinic, final diagnosis), and safety outcomes (90-day readmission for any reason, 90-day readmission with original referring complaint, 90-day major adverse cardiovascular events [MACE, defined as myocardial infarction, stroke, aborted sudden cardiac arrest, cardiac death], 90-day all-cause mortality, 90-day cardiovascular mortality).
We also conducted a patient survey to evaluate patient experience of this service. The survey was given to consecutive patients presenting over one week to complete. This consisted of three questions, and space for free-text comments:
- Overall, how would you rate your experience in clinic? (Likert scale, 1–5)
- Do you feel your concerns were addressed in clinic? (Yes or no)
- Do you feel you have been seen in a timely manner? (Yes or no)
Outcomes and statistical analysis
The outcomes of interest included time from referral to clinic appointment, investigations performed in and after clinic, final diagnoses, and safety outcomes (90-day readmission for any reason, 90-day readmission with original referring complaint, 90-day all-cause mortality, 90-day cardiovascular mortality).
Continuous variables are summarised using mean ± standard deviation (SD) or median (interquartile range [IQR]), while discrete variables are summarised using percentage incidence of each characteristic or outcome.
Ethical considerations
As this study constituted clinical audit,9 ethical approval was not required. The set-up of the service was discussed locally with multidisciplinary input and establishment of the service was part of a formal agreement within the Royal Berkshire NHS Foundation Trust.
Results
Referral characteristics
Table 1. Baseline characteristics, and overall outcomes for the referred population
| Characteristic | Total (N=216) |
|---|---|
| Mean age ± SD, years | 60.6 ± 17.1 |
| Male, n (%) | 128 (59) |
| Median referral to clinic time (IQR), days | 2 (1–5) |
| Referral indication, n (%) | |
| Chest pain | 158 (73) |
| Syncope | 23 (11) |
| Palpitations | 19 (9) |
| Documented arrhythmia | 16 (7) |
| Miscellaneous | 1 (0.5) |
| Safety outcomes, n (%) | |
| Direct admission from clinic | 8 (4) |
| 90-day mortality | 0 (0) |
| 90-day major adverse cardiovascular events | 2 (0.9) |
| 90-day all-cause unscheduled re-presentation | 40 (19) |
| 90-day unscheduled re-presentation with same presenting complaint | 18 (8) |
| Patient experience outcomes | Surveyed (N=52) |
| Mean overall experience, n/5 | 4.8 |
| Concerns addressed in clinic, n (%) | 50 (96) |
| Seen in a timely manner, n (%) | 52 (100) |
| Key: IQR = interquartile range; SD = standard deviation | |
There were 216 patients referred by the ED to the service between 1 June and 30 October 2020. Baseline characteristics are summarised in table 1. The mean age of the referred population was 60.6 years, and 128 (59%) were male. The most common reason for referral was chest pain (158/216, 73%), followed by syncope (23/216, 11%), palpitations (19/216, 9%), and management of documented arrhythmias (16/216, 7%). The median time from referral to clinic appointment was two days (IQR 1–5 days). Of referred patients, 184 (85%) were seen in clinic within one week (figure 1).
Safety outcomes
Safety outcomes are summarised in table 1. Eight patients (4%) required direct admission from clinic. Of these, six were admissions for inpatient investigation of suspected unstable angina, one for investigation of suspected pulmonary embolus, and one for cardioversion of a supraventricular tachycardia. There were 40 patients (19%) who re-presented to the ED within 90 days, with only 18 of these re-presenting with the same complaint necessitating the original referral to clinic. Overall, 11 patients (5%) required admission within 90 days for the same complaint that led to referral (including the eight that were directly admitted from clinic). There were two occurrences of MACE (0.4%) within 90 days. The first was a patient who was referred with palpitations and diagnosed with new atrial fibrillation (AF). He was discharged awaiting outpatient echocardiogram but subsequently re-presented with an out-of-hospital cardiac arrest. The second was referred with chest pain and diagnosed with stable angina. He was awaiting an urgent outpatient angiogram, but re-presented with an ST-elevation myocardial infarction (STEMI), which was successfully managed with primary percutaneous coronary intervention (PCI). Both patients survived to discharge. There were no deaths within 90 days of being seen in clinic.
Chest pain
There were 158 patients referred for further assessment of chest pain. The average age was 60.8 years, and 64% (101/158) were male. Of referred patients, 39 (24.7%) had a history of known coronary artery disease, and patients had an average of 1.7 recognised risk factors for coronary artery disease (smoking, hypertension, hypercholesterolaemia, diabetes mellitus, family history of premature coronary artery disease).

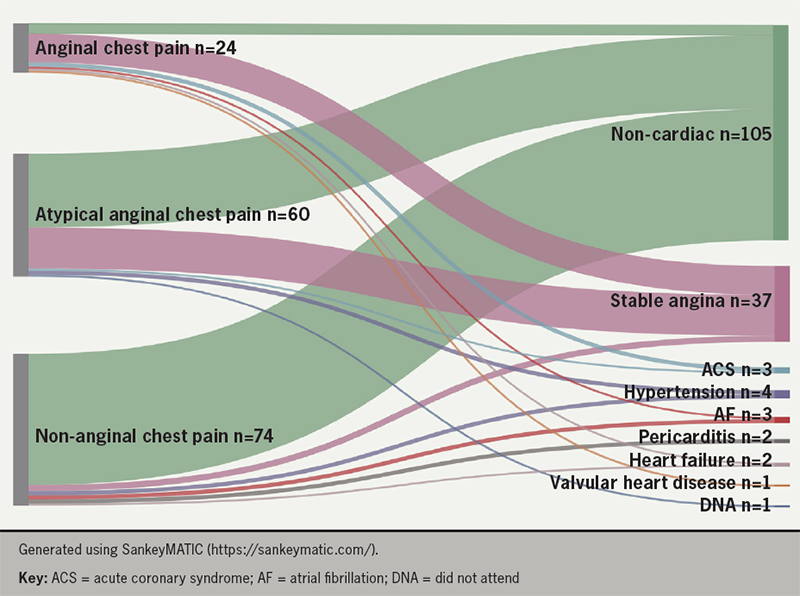
Seven patients were admitted from clinic. Ultimately, 3/158 patients (2%) were diagnosed with unstable angina, 37/158 patients (23%) were diagnosed with stable angina, and 105/158 patients (66.5%) were diagnosed with non-cardiac chest pain. In addition, 12/158 patients (8%) received an alternative cardiac diagnosis (table 2 and figure 2). There were 17 patients (8%) who required a further cardiology clinic appointment, and 54 patients (34%) who did not require further investigation. At 90 days, 28 patients (18%) had re-attended the hospital for any reason; 15 of these (10%) re-presented with chest pain and two required admission.
Table 2. Baseline characteristics, investigations, and outcomes for patients referred for further evaluation of chest pain
| Characteristic | Typical (N=24) |
Atypical (N=60) |
Non-anginal (N=74) |
|---|---|---|---|
| Known coronary artery disease, n (%) | 10 (42) | 14 (23) | 15 (20) |
| Mean number of cardiovascular risk factors ± SD | 2.3 ± 1.3 | 1.8 ± 1.0 | 1.5 ± 1.1 |
| Investigations, n (%) | |||
| CTCA | 5 (21) | 26 (43) | 11 (15) |
| Stress testing | 6 (25) | 4 (7) | 4 (5) |
| Invasive coronary angiography | 8 (33) | 5 (8)* | 2 (3) |
| Echocardiography | 10 (42) | 23 (38) | 28 (38) |
| Cardiac magnetic resonance imaging | 1 (4) | 0 (0) | 1 (1) |
| Ambulatory blood pressure monitor | 0 (0) | 1 (3) | 2 (3) |
| Holter monitor | 0 (0) | 0 (0) | 2 (3) |
| No additional investigations | 7 (29) | 16 (27) | 31 (42) |
| Safety outcomes, n (%) | |||
| Direct admission from clinic | 4 (17) | 2 (3) | 1 (1) |
| 90-day mortality | 0 (0) | 0 (0) | 0 (0) |
| 90-day major adverse cardiovascular events | 1 (4) | 0 (0) | 0 (0) |
| 90-day all-cause unscheduled re-presentation | 5 (21) | 11 (18) | 12 (16) |
| 90-day unscheduled re-presentation with same presenting complaint | 2 (8) | 12 (20) | 6 (8) |
| Diagnoses, n (%) | |||
| Unstable angina | 2 (8) | 1 (3) | 0 (0) |
| Stable angina | 14 (58) | 20 (33) | 3 (4) |
| Other cardiac diagnosis Atrial fibrillation Hypertension Heart failure Pericarditis Valvular disease |
2 (8) 1 (4) 0 (0) 1 (4) 0 (0) 1 (4) |
2 (3) 0 (0) 2 (3) 0 (0) 0 (0) 0 (0) |
7 (10) 2 (3) 2 (3) 1 (1) 2 (3) 0 (0) |
| Non-cardiac pain | 5 (21) | 36 (60) | 64 (87) |
| Did not attend | 0 (0) | 1 (3) | 0 (0) |
| *One patient presenting with atypical symptoms was offered, but declined, invasive coronary angiography Key: CTCA = computed tomographic coronary angiography; SD = standard deviation |
|||
In order to assess the appropriateness of ED referrals for chest pain, we further classified referrals according to guidance set out by the National Institute for Health and Care Excellence (NICE CG95).10 This advocates characterising chest pain based on the presence of:
- Constricting discomfort in the front of the chest with or without radiation to the neck, jaw, or arms.
- Pain precipitated by physical exertion.
- Pain relieved by rest or nitroglycerin.
There were 24 patients (15%) classified as having typical angina (fulfilling all three criteria), 60 patients (38%) atypical angina (two of three criteria), and 74 patients (47%) non-anginal chest pain (one or none of the criteria). Characteristics and outcomes for the chest pain cohort, stratified by character of chest pain, are summarised in table 2 and figure 2.
The rate of angiography (either CT coronary angiography [CTCA] or invasive angiography) was similar in those presenting with typical or atypical symptoms: 50% and 48%, respectively (one patient in each group had initial CTCA then invasive angiography). In those presenting with anginal symptoms the rate of initial invasive angiography was, as expected, higher (29% vs. 5%) than those without anginal symptoms. In those presenting with non-anginal chest pain, only 18% underwent CTCA or invasive angiography. The rate of diagnosis of angina ranged from 4% (non-anginal presentations) to 64% (anginal presentations): the overall prevalence of angina was 25% (40/158).
Syncope
There were 23 patients referred for assessment of suspected syncope. Most patients underwent some form of assessment for structural heart disease (echocardiography or cardiac MRI: 57%, 13/23), and some form of rhythm monitoring (Holter or implantable loop recorder: 74%, 17/23). These, and further investigations, are summarised in table 3. Ultimately, six patients were diagnosed with cardiac syncope, and one with supraventricular tachycardia; the rest were diagnosed with a combination of vasovagal syncope, non-cardiac syncope, and postural hypotension (table 4). Only one patient required a further follow-up appointment.
Table 3. Investigations and outcomes for patients referred for further evaluation of palpitations, syncope, and documented arrhythmias
| Syncope (N=23) |
Palpitations (N=19) |
Documented arrhythmia (N=16) |
|
|---|---|---|---|
| Investigations, n (%) | |||
| Holter monitoring | 15 (65) | 7 (37) | 2 (13) |
| Implantable loop recorder | 6 (26) | 0 (0) | 0 (0) |
| Echocardiography | 13 (57) | 9 (47) | 8 (42) |
| Bubble contrast echocardiography | 0 (0) | 1 (5) | 0 (0) |
| Stress/exercise test | 2 (8) | 0 (0) | 1 (6) |
| CMR | 3 (13) | 0 (0) | 0 (0) |
| CTCA | 1 (4) | 0 (0) | 1 (6) |
| No additional investigations | 4 (17) | 3 (16) | 6 (38) |
| Safety outcomes, n (%) | |||
| Direct admission from clinic | 0 (0) | 1 (5) | 0 (0) |
| 90-day mortality | 0 (0) | 0 (0) | 0 (0) |
| 90-day major adverse cardiovascular events | 0 (0) | 0 (0) | 1 (6) |
| 90-day all-cause unscheduled re-presentation | 6 (26) | 3 (16) | 3 (19) |
| 90-day unscheduled re-presentation with same presenting complaint | 1 (4) | 0 (0) | 2 (13) |
| Key: CMR = cardiac magnetic resonance imaging; CTCA = computed tomographic coronary angiography | |||
Table 4. Diagnoses for patients referred for further evaluation of palpitations, syncope, and documented arrhythmias (with stratification based on management undertaken)
| Diagnoses | n (%) |
|---|---|
| Syncope (N=23) | |
| Cardiac syncope | 6 (26) |
| Supraventricular tachycardia | 1 (4) |
| Non-cardiac syncope Benign paroxysmal positional vertigo Neurological event Uncertain cause (normal investigations) |
5 (22) 1 (4) 1 (4) 3 (13) |
| Vasovagal syncope | 9 (39) |
| Postural hypotension | 2 (9) |
| Palpitations (N=19) | |
| Atrial fibrillation | 3 (16) |
| Supraventricular tachycardia | 2 (11) |
| Premature ventricular complexes (medical management) | 6 (32) |
| Benign palpitations | 5 (26) |
| Documented arrhythmia (N=16) | |
| Atrial fibrillation Referred to electrophysiology clinic Outpatient DC cardioversion |
8 (50) 1 (6) 1 (6) |
| Atrial flutter Referred to electrophysiology clinic Outpatient DC cardioversion |
3 (19) 2 (13) 1 (6) |
| Supraventricular tachycardia Referred to electrophysiology clinic (for electrophysiology study ± ablation) |
5 (31) 2 (13) |
| Key: DC = direct current | |
At 90 days, six patients had re-presented to hospital for any reason, although only one patient re-presented for the same reason as the index referral; they were discharged safely from the ED. There were no deaths at 90 days (table 3).
Palpitations
There were 19 patients referred with palpitations. Just under half (8/19, 42%) underwent some form of rhythm monitoring. Ten patients underwent an assessment for structural heart disease with echocardiography. Investigations are summarised in table 3. One patient was admitted from clinic with a narrow complex tachycardia and was cardioverted with adenosine before being discharged later that day.
Ultimately, the majority received a cardiac diagnosis (14/19, 74%) and five were diagnosed with benign palpitations (table 4). At 90 days, there were three re-presentations with non-cardiac complaints. There were no re-presentations or admissions for cardiac reasons (table 3).
Documented arrhythmia
There were 16 patients referred for further assessment of a documented arrhythmia. Of these, 11 were for atrial fibrillation or flutter and five were for supraventricular arrhythmias (defined as narrow complex tachycardias that were not AF or flutter) (table 4).
At 90 days, three patients re-presented to hospital for any reason (table 3). Two of these patients re-presented with issues relating to their original referral and one required hospital admission.
Miscellaneous
One patient was referred for assessment of a painful implantable loop recorder site, with no intervention indicated.
Patient experience survey
A total of 52 patients completed the patient experience survey. Overall feedback was positive. The mean rating of patients’ overall experience was 4.8/5. Most, 50/52 (96%), patients reported that they felt their concerns had been addressed in clinic, and 52/52 (100%) felt that they had been seen in a timely manner.
Discussion
This retrospective study demonstrates that a rapid-access general cardiology service can prevent unnecessary acute cardiology admissions, while maintaining both patient safety and satisfaction.
Rapid-access cardiology services
Rapid-access chest pain clinics have become commonplace in the UK since National Service Framework recommendations in 2000,11 but rapid-access general cardiology clinics are less common.
Here, we report our experience of a novel rapid-access general cardiology service designed to help support our ED colleagues during the COVID-19 pandemic. There were 216 ED referrals reviewed at a median of two days. Of referred patients, 205 (95%) were successfully managed without needing hospital admission at any point during our 90-day follow-up period, and only 11 patients required admission to hospital within 90 days (eight directly from clinic, and three at a later date). We were not able to directly compare rates of cardiology admissions to similar periods in previous years due to numerous confounding factors, not least changes in healthcare delivery and patient behaviour during the COVID-19 pandemic. However, our finding that 95% of referred patients were successfully managed as outpatients suggests a significant admission avoidance impact of this service.
Furthermore, we report good safety outcomes, with no deaths, and two (0.9%) MACE at 90 days. There were 40 patients who re-presented to ED, but only 18 (8%) were related to their index referral. Overall, these figures are similar to what has been reported in established rapid-access chest pain clinics.12
Finally, our service was well-received by patients. The average overall rating of the service was 4.8/5. In the current climate of high ED attendances and long waiting times,13 a service where 100% of referred patients felt they had been seen in a timely manner, and 96% felt their concerns were adequately addressed, provides much-needed relief to both emergency services and patients.
We have found only two descriptions of similar services in the literature. One UK centre reported outcomes for a combined rapid-access chest pain, arrhythmia, and heart failure service serving a population of 165,000 patients.14,15 They provided an open-access, walk-in service for referrals from the ED and general practitioners. Exact figures on waiting times, re-presentations, and readmissions were not supplied, though the authors report most patients were seen on the same day as referral. At one year, cardiac mortality was 1%, and overall mortality 3%.14 A Dutch centre established a ‘one-stop’ rapid-access cardiology clinic.16 Again, average waiting times and admission statistics were not supplied, though the authors reported that all patients were seen within five working days. At 10 years, cardiac mortality was 4% with an overall mortality rate of 12%.
In both services, the rates of diagnosis of non-cardiovascular causes of symptoms ranged from 60 to 70%.14–16 This is slightly higher than observed in our cohort (51%). This may be explained by the observation that most non-chest pain referrals resulted in a new cardiac diagnosis. In contrast, 67% of chest pain referrals resulted in a diagnosis of non-cardiac chest pain, which is in keeping with the diagnostic rates of non-cardiac causes of chest pain among rapid-access chest pain services in the literature.17 Furthermore, 46.8% of referrals did not meet NICE criteria for rapid-access chest pain referral, which highlights an area for further improvement of the referral process.
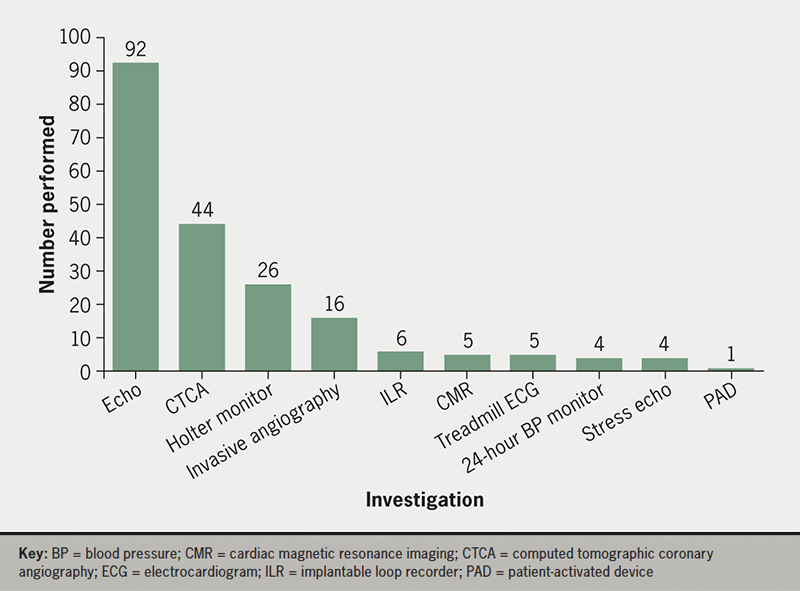
The success of our service relied both on the availability of same-day investigations (echocardiography, stress testing) to aid diagnosis and risk stratification for safe discharge, as well as access to urgent outpatient investigations for timely work-up. The volume of investigations performed is illustrated in figure 3: wider applicability of this service will depend on local availability of such resources.
Limitations
This was a retrospective cohort analysis of the population referred to the rapid-access cardiology service. While we have shown that most patients can be safely and effectively managed in an outpatient manner, we were not able to prove a reduction in cardiac admission rates as a result. Due to the circumstances of the COVID-19 pandemic, which led to a change in clinical practice and service structure, we could not perform a direct comparison to admission rates of previous years. Any such comparison would likely have been confounded by an overall decrease in inpatient admissions during the COVID-19 pandemic.
Although the overall profile of referrals was similar between our cohort and others described, one notable difference is in the lack of patients referred with suspected heart failure to our service. While reasons for this are not clear, it may relate to pre-existing pathways to diagnose and manage heart failure patients. Local general practitioners and the ED are able to request open-access echocardiograms for patients with suspected heart failure, which obviates the need for rapid-access cardiology referrals for initial diagnosis and management. There is also an established community heart function service in our region for patients with known heart failure. These established outpatient pathways may explain the lack of heart failure-related referrals to the service.
Finally, although we present outcomes for the short and medium term, assessment of longer-term outcomes is necessary.
Future applications
This clinic model can provide continual benefits in reducing inpatient admission even beyond the exceptional pandemic conditions that necessitated its conception. During the COVID pandemic, when there was a significant reduction in routine outpatient activity, it ensured that patients with suspected cardiac pathology are reviewed by specialists in a timely manner. Going forward, in the context of the significant backlog caused by multiple waves of the pandemic, and ever-increasing NHS waiting lists and ED attendances,18 services like ours will expedite specialist-led work-up and treatment of patients with acute conditions not requiring emergent inpatient treatment. Indeed, given the success and safety demonstrated by our pilot, our ambulatory rapid-access cardiology clinic has been continued indefinitely, and is currently being expanded to include rapid-access general practitioner referrals. Finally, this service model may provide a framework for other departments to deliver rapid-access cardiology pathways, such as mandated in UK guidance by the Getting it Right First Time report.19
Conclusion
This rapid-access general cardiology clinic was effective and well-utilised, offering rapid review of patients discharged from the ED with suspected cardiac pathology, while maintaining patient safety. Broader uptake of such rapid-access cardiology services may be valuable in improving patient experience through access to prompt diagnosis, and serve as a safe and effective admission avoidance service.
Key messages
- Patients with suspected cardiac pathology constitute a large proportion of emergency department (ED) attendances; many of these could be safely investigated in the urgent outpatient setting, over and above current routinely available services for this (rapid-access chest pain clinics)
- We report outcomes for a rapid-access general cardiology clinic established during the COVID-19 pandemic, for patients discharged from the ED with suspected cardiac pathology. This was effective and well-utilised, while maintaining patient safety, with high patient satisfaction
- Beyond the exceptional circumstances that necessitated its conception, this clinic model could be a useful framework for others looking to provide early specialist-led outpatient work-up and treatment of presentations that would otherwise be associated with the costs of inpatient admission: locally, the clinic has continued running since the pandemic
Conflicts of interest
None declared.
Funding
None.
Study approval
As this study constituted clinical audit,9 ethical approval was not required. The set-up of the service was discussed locally with multidisciplinary input and establishment of the service was part of a formal agreement within the Royal Berkshire NHS Foundation Trust.
References
1. The King’s Fund. Key facts and figures about the NHS. London: The King’s Fund, 2022. Available from: https://www.kingsfund.org.uk/audio-video/key-facts-figures-nhs [accessed 10 May 2022].
2. Ewbank L, Thompson J, McKenna H, Anandaciva S, Ward D. NHS hospital bed numbers: past, present, future. London: The King’s Fund, 2021. Available from: https://www.kingsfund.org.uk/publications/nhs-hospital-bed-numbers [accessed 27 April 2022].
3. National Health Service. The NHS Long Term Plan. London: NHS, 2019. Available from: https://www.longtermplan.nhs.uk
4. Goodacre S, Cross E, Arnold J et al. The health care burden of acute chest pain. Heart 2005;91:229–30. https://doi.org/10.1136/hrt.2003.027599
5. Mockel M, Searle J, Muller R et al. Chief complaints in medical emergencies: do they relate to underlying disease and outcome? The Charité Emergency Medicine Study (CHARITEM). Eur J Emerg Med 2013;20:103–08. https://doi.org/10.1097/MEJ.0b013e328351e609
6. Bjørnsen LP, Naess-Pleym LE, Dale J, Grenne B, Wiseth R. Description of chest pain patients in a Norwegian emergency department. Scand Cardiovasc J 2019;53:28–34. https://doi.org/10.1080/14017431.2019.1583362
7. Boyle RM. Value of rapid-access chest pain clinics. Heart 2007;93:415–16. https://doi.org/10.1136/hrt.2006.100248
8. Ogrinc G, Davies L, Goodman D et al. SQUIRE 2.0 (Standards for QUality Improvement Reporting Excellence): revised publication guidelines from a detailed consensus process. BMJ Qual Saf 2016;25:986–92. https://doi.org/10.1136/bmjqs-2015-004411
9. Health Research Authority. Defining Research Table. London: Health Research Authority, 2022. Available from: https://www.hra-decisiontools.org.uk/research/docs/DefiningResearchTable_Oct2022.pdf Last accessed March 2024
10. National Institute for Health and Care Excellence. Chest pain of recent onset: assessment and diagnosis of recent-onset chest pain or discomfort of suspected cardiac origin. CG95. London: NICE, 2016. Available from: https://www.nice.org.uk/guidance/cg95
11. Department of Health. National service framework for coronary heart disease. London: Department of Health, 2000. Available from: https://www.gov.uk/government/publications/quality-standards-for-coronary-heart-disease-care
12. Kite TA, Gaunt H, Banning AS et al. Clinical outcomes of patients discharged from the rapid access chest pain clinic with non-anginal chest pain: a retrospective cohort study. Int J Cardiol 2020;302:1–4. https://doi.org/10.1016/j.ijcard.2019.12.008
13. NHS England. A&E attendances and emergency admissions March 2022 statistical commentary. Leeds: NHS England, 2022. Available from: https://www.england.nhs.uk/statistics/wp-content/uploads/sites/2/2022/04/Statistical-commentary-March-2022-jf8.pdf [accessed 10 May 2022].
14. Tenkorang JN, Fox KF, Collier TJ, Wood DA. A rapid access cardiology service for chest pain, heart failure and arrhythmias accurately diagnoses cardiac disease and identifies patients at high risk: a prospective cohort study. Heart 2006;92:1084–90. https://doi.org/10.1136/hrt.2005.079376
15. Debney MT, Fox KF. Rapid access cardiology – a nine year review. Q J Med 2012;105:231–4. https://doi.org/10.1093/qjmed/hcr182
16. Lederink T, Balkestein EJM. First time referral reasons, diagnoses and 10-year follow-up of patients seen at a Dutch fast lane outpatient cardiology clinic. Neth Heart J 2019;27:354–61. https://doi.org/10.1007/s12471-019-1266-x
17. Klimis H, Thiagalingam A, Altman M et al. Rapid-access cardiology services: can these reduce the burden of acute chest pain on Australian and New Zealand health services? Int Med J 2017;47:986–91. https://doi.org/10.1111/imj.13334
18. House of Commons Library. NHS key statistics: England, July 2023. London: House of Commons, 2023. Available from: https://commonslibrary.parliament.uk/research-briefings/cbp-7281/ [accessed 30 July 2023].
19. Clark S, Ray S. Cardiology – GIRFT programme national specialty report. London: Getting it Right First Time (GIRFT), 2021. Available from: https://gettingitrightfirsttime.co.uk/medical_specialties/cardiology/
