A young man with multifocal cavitating pneumonia presented with early abscess formation secondary to Staphylococcus aureus bacteraemia treated with intravenous (IV) flucloxacillin. Further workup with transthoracic echocardiography revealed a large vegetation on the tricuspid valve with at least moderate tricuspid regurgitation; however, there were no peripheral stigmata of infective endocarditis. There was no history of intravenous drug use, but he had a history of administering frequent intramuscular recreational steroid injections. He also had a recent history of a loose tooth. In addition, there were multiple skin excoriations from scratching related to anxiety. Transoesophageal echocardiography confirmed two vegetations on the tricuspid valve, the largest measuring 21 mm with evidence of severe tricuspid regurgitation. The findings were discussed in the cardiac surgery multidisciplinary meeting and the consensus was for initial sterilisation with IV antibiotics followed by surgery.
Introduction
The tricuspid valve (TV) is involved in 90% of patients with right-sided endocarditis and is most common in people with intravenous drug use (IVDU). Septic pulmonary emboli occur in >50% of patients with TV involvement and manifests with various respiratory symptoms.1
Case report
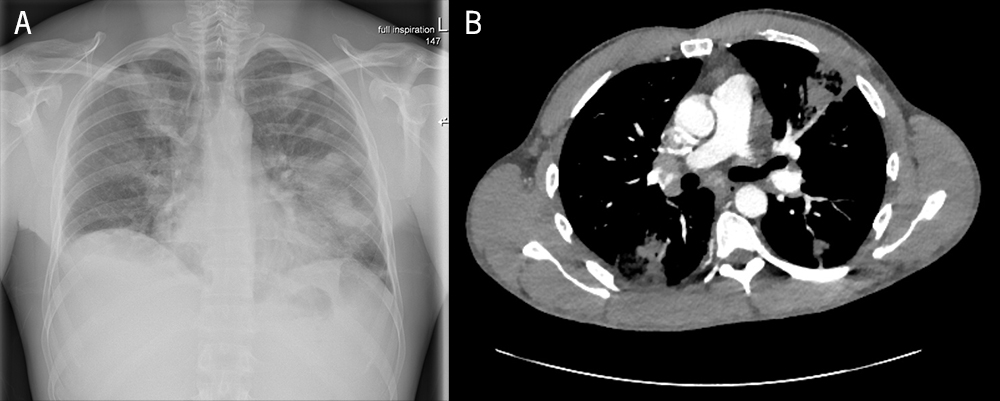
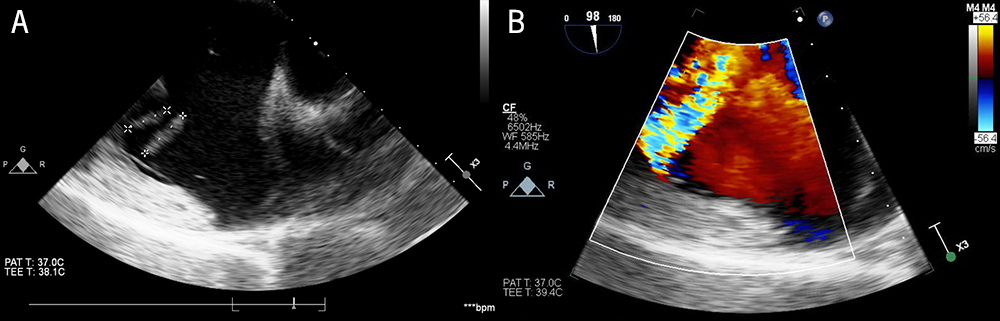
A 38-year-old man presented with a prodrome of flu-like illness along with night sweats, pleuritic chest pain and cough for two weeks unresponsive to the usual first- and second-line oral antibiotics (amoxicillin 1 g 8 hourly for five days, and doxycycline 100 mg 12 hourly for five days, respectively). There was no history of illicit IVDU or any condition suggesting that he was immunocompromised; however, there was a history of administering frequent intramuscular recreational steroid injections. He also had a history of a loose tooth over the past two months. He had no peripheral stigmata of infective endocarditis. Skin examination revealed multiple excoriations on both forearms from scratching related to anxiety. Blood workup revealed raised inflammatory markers, including a C-reactive protein of 120 mg/L (normal: 0–5 mg/L). Chest X-ray (figure 1A) and computed tomography (figure 1B) findings were consistent with multifocal cavitating pneumonia with early abscess formation. Further assessment, including screening for HIV, tuberculosis and atypical infections, was negative. Blood cultures revealed a methicillin-sensitive Staphylococcus aureus bacteraemia for which he was started on intravenous (IV) flucloxacillin 2 g IV four times a day. His loose tooth may have been an additional source of his bacteraemia. Further workup with transthoracic echocardiography for S. aureus bacteraemia demonstrated a large, partially mobile echodensity on the TV with at least moderate tricuspid regurgitation (TR). Transoesophageal echocardiography confirmed two vegetations on the TV (figure 2A), the largest measuring 21 mm, along with evidence of severe TR (figure 2B). The findings were discussed in the cardiac surgery multidisciplinary meeting and the consensus was for initial sterilisation with IV flucloxacillin followed by excision of the vegetation with or without TV repair.2
Discussion
This case reinforces the importance of detailed work-up, including an echocardiography, in patients with multifocal cavitary pneumonia and also the need for echocardiography in S. aureus bacteraemia without an apparent source.3 All patients with TV endocarditis need treatment with IV antibiotics along with a multidisciplinary discussion for surgical assessment, especially in those with persistent bacteraemia after at least one week of appropriate antibiotic therapy, large TV vegetations (>20 mm), recurrent septic pulmonary emboli, involvement of left-sided structures and right-sided heart failure secondary to severe TR unresponsive to diuretics.4
Key messages
- In right-sided endocarditis, the tricuspid valve is involved in 90% of patients and is most common in people with intravenous drug use
- Septic pulmonary emboli occur in >50% of patients with tricuspid valve involvement and manifests with various respiratory symptoms and signs, such as multifocal cavitatory pneumonia seen in this case
- In patients with an unidentified source of bacteraemia, a detailed workup including echocardiography is essential to identify the underlying pathogen and appropriate intravenous treatment commenced while considering surgical interventions
Conflicts of interest
None declared.
Funding
None.
Statement of consent
Written consent was granted by the patient for publication of this case report.
References
1. Yuan SM. Right-sided infective endocarditis: recent epidemiologic changes. Int J Clin Exp Med 2014;7:199–218. [Epub online ahead of print]
2. Hussain ST, Witten J, Shrestha NK, Blackstone EH, Pettersson GB. Tricuspid valve endocarditis. Ann Cardiothorac Surg 2017;6:255–61. https://doi.org/10.21037/acs.2017.03.09
3. Abraham L, Bamberger DM. Staphylococcus aureus bacteremia: contemporary management. Mo Med 2020;117:341–5.
4. Delgado V, Ajmone Marsan N, de Waha S et al. 2023 ESC Guidelines for the management of endocarditis. Eur Heart J 2023;44:3948–4042. https://doi.org/10.1093/eurheartj/ehad193
