Depression and anxiety are commonly experienced by cardiac patients and are associated with reduced quality of life and mortality, but the evidence for the effectiveness of medical and psychological treatments for depression has been mixed.
 We explored the psychological needs of cardiac patients and developed a stepped-care model of psychological care, which was both accessible and acceptable to cardiac patients. The clinical psychologist was integral to the cardiac rehabilitation team and provided joint working, support and a range of interventions.
We explored the psychological needs of cardiac patients and developed a stepped-care model of psychological care, which was both accessible and acceptable to cardiac patients. The clinical psychologist was integral to the cardiac rehabilitation team and provided joint working, support and a range of interventions.
Preliminary evidence suggests that offering a range of psychological treatments might be an effective way of meeting cardiac patients’ psychological needs. Specific psychological interventions included: psycho-education sessions addressing behavioural risk factors and adjustment, brief individual therapy for patients with mild-to-moderate, as well as for those with severe, mental illness, group workshops and individual therapy, using cognitive-behaviour therapy for anxiety, depression and adjustment to adverse life events. Overall, the percentage of patients reporting depression and anxiety reduced by 13% and 19%, respectively, following this cardiac rehabilitation, which is a 30 day rehab programme compared with a national average of 4%. Further work might compare this model of service with others using controlled designs with follow-up measures.
Introduction
The prevalence of anxiety and depression among patients with cardiac conditions is three times higher than in the general population, with 25–30% of patients reporting persistent problems with anxiety and/or depression.1,2 The prevalence of depression alone after an acute cardiac event ranges from 15% to 45%.3 There is evidence that depression is a significant, independent influence on cardiac mortality.4 This impact is at least equivalent to that of left ventricular dysfunction and history of previous myocardial infarction (MI).5 Over and above their impact on quality of life, anxiety and depression are associated with poorer self-management and health outcomes, as well as increased incidence of cardiac events and health service utilisation.6,7
Cardiac rehabilitation is a multi-disciplinary activity that aims to facilitate physical, psychological and emotional recovery, and to enable patients to achieve and maintain better health.8 Attendance at cardiac rehabilitation is also lower among patients with depression9 and drop out rates are higher.10
Psychosocial interventions have been developed in cardiac rehabilitation programmes and are advocated by the National Service Framework (NSF) for Coronary Heart Disease (CHD)11 and the National Institute for Health and Clinical Excellence (NICE).12 Despite this, only a minority of patients who are depressed after an MI receive treatment for their depression.6 A strong evidence base exists for the efficacy of psychological interventions in addressing anxiety and depression in the general population.13 Several studies have examined the effectiveness of psychosocial interventions in patients with cardiac disease with mixed outcomes.14,15 A Cochrane review in 2004 concluded that, while psychological interventions showed no evidence of effect on total or cardiac mortality, they did show some small reductions in anxiety and depression in patients with CHD.16
The Enhancing Recovery in Coronary Heart Disease Patients (ENRICHD) study17 of patients undergoing cognitive-behavioural therapy post-MI demonstrated that there were improvements in patients’ levels of depression and social support six months after initiation of therapy, although benefits were not sustained at 30 months. The Myocardial Infarction and Depression – Intervention Trial (MIND-IT)18 evaluated the effectiveness of antidepressant treatment compared with usual care in an effectiveness study. At 18 months post-event no differences were observed between intervention and control groups in mean scores on the Beck Depression Inventory. It was concluded that antidepressant treatment did not alter long-term depression, post-MI status or improve cardiac prognosis.18
The results from the Sertraline Antidepressant Heart Attack Randomised Trial (SADHART) study19 of almost 400 patients demonstrated that sertraline is safe and effective for the treatment of depression in patients following MI or with unstable angina. However, although sertraline lowered treatment-emergent cardiovascular events, the effect was not statistically significant.
A meta-analysis for psychological treatment of cardiac patients20 concluded that psychological treatment offered in addition to usual care reduced mortality, for men, at least in the first two years. A further finding was that offering psychological treatment very soon after a cardiac event shows little benefit compared with usual care, whereas those starting treatment two months post-event showed an impressive mortality reduction of 72% in the first two years. Interestingly, a recent UK National Audit of Cardiac Rehabilitation21 found small overall reductions in anxiety and depression (averaging 4%) following cardiac rehabilitation; however, only 33% had a psychologist contributing to the rehabilitation sessions and only 3% of programmes included psychological interventions.
The cardiac rehabilitation team at Guy’s and St Thomas’ Foundation Trust designed a project to:
- define cardiac patients’ psychological needs
- develop a service that was accessible and acceptable to patients with interventions to meet their specific needs and improve patient outcomes (mood and patient satisfaction).
The model
Funding was granted by the Guy’s and St Thomas’ Charity for the project, which involved close working between Guy’s and St Thomas’ (GSTT) and South London and Maudsley (SLAM) NHS Foundation Trusts. A clinical psychologist was employed to provide a service within cardiothoracic services at GSTT for three years. Although initially the focus was solely on the needs of patients with coronary artery disease, this parameter was broadened during the course of the project to include other cardiac conditions – notably patients with heart failure and patients with implantable cardiac defibrillators (ICDs).
Defining cardiac patients’ psychological needs
GSTT cardiac patients presented with a range of psychological needs in terms of severity, complexity and duration. These difficulties were broadly associated with adjustment to having cardiac problems, including:
- concerns about the significance and impact of symptoms
- adherence to or side effects from treatments
- shock, disbelief and denial about having a cardiac problem
- coping and engaging in everyday activities
- modifying behavioural risk factors for coronary heart disease
- changes in their relationships and interactions with other people
- catastrophic interpretations about the impact of cardiac disease on their lives and prospects for the future
- the re-emergence or intensification of pre-morbid psychological difficulties.
Anxiety and depression
Audit data using the Hospital Anxiety and Depression Scale (HADS)22 showed that approximately 30–45% of patients had at least borderline levels of anxiety or depression at assessment for cardiac rehabilitation. Many of these patients were reluctant to accept a diagnosis of anxiety or depression and expressed reservations to the clinical psychologist, for example, by rejecting the term ‘depression’ for describing their problems, or by expressing negative views about attending a mental health service for treatment. Finding patient-acceptable ways to characterise these problems and treat them was, thus, an important service development issue.
Psychological adjustment to cardiac events
Psychological models of adjustment describe the ways that people adapt and learn to cope with chronic conditions over time. They provide a useful framework for describing the psychological needs reported by many patients who experience mild-to-moderate difficulties, as well as those who have an anxiety disorder or depression. While often associated with the nature of the cardiac problem, for some patients adjustment involves coming to terms with difficult consequences of treatment, such as pain and distress caused by ICD activation.
Behavioural risk factors for coronary heart disease
- Many of the treatment goals in cardiac rehabilitation are associated with behavioural risk factors for CHD, as described by the NSF for CHD. These include:
- resuming appropriate levels of exercise
- smoking cessation
- weight management (body mass index [BMI] <30 kg/m2).
The clinical psychologist contributed to interventions to meet these needs during the cardiac rehabilitation programme. In addition, individual patients sought psychological intervention for addressing these risk factors, as well as alcohol use and stress management.
Other psychological needs
People with severe mental health problems also suffer from cardiac disease. These included enduring problems, such as psychotic illness, as well as other problems such as post-traumatic stress disorder (PTSD) and severe depression. Their use of hospital services can be adversely affected by their mental health problems. During the course of this project, 24% of patients attending for psychological assessment were patients with these needs. In addition, the multi-disciplinary team (MDT) sought advice on managing some of these patients within the cardiac rehabilitation group programme. The clinical psychologist worked closely with both Trusts (Acute and Mental Health) to ensure effective liaison and intervention.
Patients with high-intensity physical healthcare needs, such as those with heart failure, were another group presenting with special needs. The clinical psychologist contributed a new psycho-education session for heart failure patients and initiated liaison work with the GSTT heart failure team to address this need.
Service development and implementation
A key objective of the project was to develop a service that was readily accessible and acceptable to GSTT patients where their physical and psychological needs were assessed holistically. The service was designed with multiple access points to the psychological service, which were created corresponding to particular stages of the patient’s journey from cardiac event to recovery at one year (figure 1).
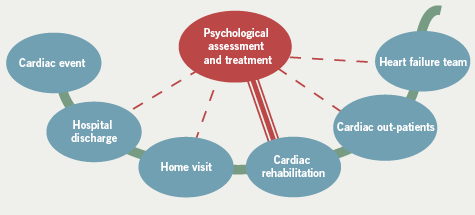
Methods
All patients entering the cardiac rehabilitation programme met the clinical psychologist at their assessment and were offered psycho-education sessions. Patients were screened for psychological difficulties at four points during the year following their cardiac event. Referrals to clinical psychology were made at all of these time points (figure 1). Because the clinical psychologist met regularly with the MDT, the team was also able to identify patients who were reluctant to seek help. Patients were also referred by cardiologists in cardiac out-patients as well as by cardiologists and nurses within the heart failure team.
Patients were initially seen for assessment in cardiac out-patient clinics rather than a psychology clinic or mental health setting, in order to encourage attendance and reduce possible stigma. The clinical psychologist also met patients with other members of the cardiac rehabilitation and heart failure teams, a helpful measure for those patients reluctant to attend a psychology clinic. In addition, three patient leaflets were developed to provide information about psychological services at different points during the patient’s journey.
Meeting patient need with appropriate interventions
Current Department of Health guidance suggests that patients with common mental health problems should be offered services that are acceptable for patients and practical for services. This project endeavoured to deliver such a stepped-care service, with interventions that matched patient need to treatment intensity.
Interventions offered:
- Psycho-education sessions provided to all patients within the cardiac rehabilitation educational component, addressing behavioural risk factors and adjustment issues. These were co-facilitated with other members of the MDT, allowing for inter-professional learning.
- Brief individual therapy – consisting of one to six sessions. This included cardiac-focused/engagement-focused interventions for patients with more severe mental health problems.
- Individual therapy using cognitive-behaviour therapy for anxiety, depression and adjustment to adverse life events. Patients were seen for 4–26 sessions, depending on their needs and preferences.
- Brief individual therapy for patients with severe mental illness (SMI) – consisting of one to six sessions focused on cardiac issues, risk and reducing levels of distress. Patients not in contact with mental health services were referred to appropriate providers.
- Group workshops consisting of eight sessions for small groups (three to eight patients) were also offered. The workshops were taken up primarily by patients engaged in individual therapy for anxiety or depression. Group interventions developed with support from psychotherapists within the mental health trust (SLAM).
Results
Patients accessing psychological services
The project attracted a significant increase in the number of patients, with approximately 50% accepting psychology referrals, compared with 20% accepting referral to liaison psychiatry services in previous years. The number of patients referred reflects the percentage of patients reporting persistent problems with anxiety and depression in the cardiac population.
Attendance
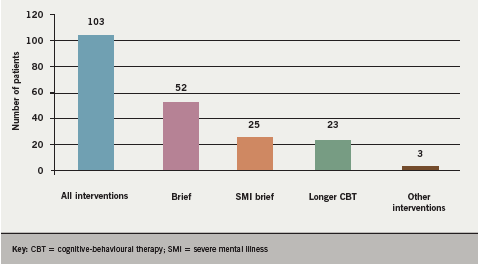
Patients were assessed by the clinical psychologist and supported in choosing the intervention most acceptable to them. In total, 103 (82%) of the 125 patients referred accepted interventions from the psychologist. The gender (62% male and 38% female) and ethnicity (70% White, 10% Black, 8% Asian, 7% other and 6% not recorded) of the patients was similar to that of patients attending cardiac rehabilitation. More than half of patients attending chose to have brief therapy, with substantial numbers engaging in all the options described above (figure 2).
Outcomes
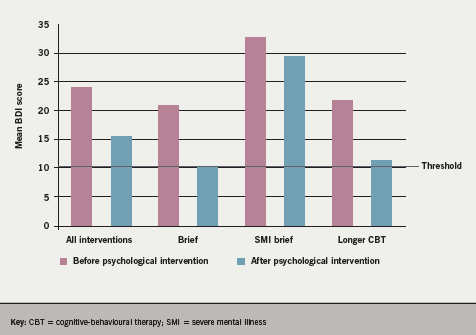
Overall, audit data for 460 patients attending cardiac rehabilitation during the two years (2005–2007) using the model, showed a reduction of 19% for anxiety and 13.5% for depression (HADS22): 41.5% had borderline/clinical anxiety before the programme and 22% afterwards, while 28.75% had borderline/clinical depression before and 15.25% after the programme. These data can be compared with the national average reductions of 4%.21 The Beck Depression Inventory (BDI)23 was given before and after specific psychological interventions and data were available for 43 patients. The results showed significant reductions in levels of depression after treatment (pre-treatment mean 24.42, standard deviation [sd] =11.70; post-treatment mean 14.98, sd=10.90; t=7.64, df 42, p<0.00001) and three months later (follow-up mean 15.79, sd=11.01; t=7.74, df=38, p<0.0001). There were fewer changes for those with severe mental health problems (figure 3).
Satisfaction with the interventions was assessed using the Client Satisfaction Questionnaire (CSQ).24 Data collected after interventions showed overall satisfaction rates of 86% for all intervention types, ranging from 83% to 93%.
Discussion
Given the relatively high prevalence and impact of anxiety and depression among cardiac patients, it is imperative to find effective interventions. The integration of psychological care within acute settings enabled increased accessibility and patient acceptability. In the UK, addressing these needs has attracted increasing attention from policy-makers. For example, the Improving Access to Psychological Therapies (IAPT) programme has laid particular emphasis on addressing the needs of patients with long-term conditions, such as cardiac conditions. This stepped-care model placed the psychologist in the heart of the cardiac rehabilitation team, thus providing an integrated service. The cardiac rehabilitation team strives to deliver a menu-driven programme to patients and the psychologist’s sessions were an integral part together with nurses, doctors, physiotherapist, dietitian and pharmacist. This lessened the inconvenience and possible stigma of attending other departments, and normalised the inclusion of psychological issues for all the patients. Patients experienced the psychology sessions as part of their cardiac rehabilitation programme. The psychologist also provided the team with support in addressing psychological issues, and further enabled them to work holistically in meeting the patients’ needs.
 The audit data for outcomes during 2005–2007 showed high levels of anxiety and depression – higher than the national average,21 which may be explained by the higher needs within an inner city location. Nevertheless, the programme also resulted in greater reductions in anxiety (19%) and depression (13%) than the national average (4%). The significant reduction in depression (BDI) among those treated by the psychologist is encouraging and the stepped-care model is consistent with care pathways for depression and long-term conditions. The service could be offered within acute trust settings or within community clinics. The flexible timing of the psychological interventions and the emphasis on patient choice of the level of intervention were felt to be important elements of the service. However, further collaborative work between acute Trusts, Mental Health Trusts and Primary Care Trusts needs to be undertaken to examine the longer-term outcomes of this service model.
The audit data for outcomes during 2005–2007 showed high levels of anxiety and depression – higher than the national average,21 which may be explained by the higher needs within an inner city location. Nevertheless, the programme also resulted in greater reductions in anxiety (19%) and depression (13%) than the national average (4%). The significant reduction in depression (BDI) among those treated by the psychologist is encouraging and the stepped-care model is consistent with care pathways for depression and long-term conditions. The service could be offered within acute trust settings or within community clinics. The flexible timing of the psychological interventions and the emphasis on patient choice of the level of intervention were felt to be important elements of the service. However, further collaborative work between acute Trusts, Mental Health Trusts and Primary Care Trusts needs to be undertaken to examine the longer-term outcomes of this service model.
Acknowledgements
This service development was funded by the Guy’s & St Thomas’s Charity. We also acknowledge the NIHR Biomedical Research Centre for Mental Health, South London & Maudsley NHS Foundation Trust and Institute of Psychiatry, King’s College London.
Conflict of interest
None declared.
Key messages
- Depression and anxiety are commonly experienced by cardiac patients and are associated with reduced quality of life and mortality
- The evidence for the effectiveness of medical and psychological treatments for depression has been mixed
- We developed a stepped-care model of psychological care, which was both accessible and acceptable to cardiac patients
- Preliminary evidence suggests that offering a range of psychological treatments might be an effective way of meeting psychological needs
References
1. Lane D, Carroll C, Ring C et al. The prevalence and persistence of depression and anxiety following myocardial infarction. Br J Health Psychol 2002;7:11–21.
2. Blumenthal JA, Lett HS, Babyak A et al. Depression as a risk factor for mortality after coronary artery bypass surgery. Lancet 2003;362:604–09.
3. Scottish Intercollegiate Guidelines Network. 57 Cardiac rehabilitation: a national clinical guideline. Edinburgh: SIGN Executive, January 2002.
4. Ladwig KH, Kieser M, Konig J et al. Affective disorders and survival after acute myocardial infarction. Eur Heart J 1991;12:959–64.
5. Frasure-Smith N, Lesperance F, Talajic M. Depression following myocardial infarction – impact on 6 month survival. JAMA 1993;270:1819–25.
6. Carney M, Freedland KE, Miller GE, Jaffe AS. Depression as a risk factor for cardiac mortality and morbidity: a review of potential mechanisms. J Psychosom Res 2002;53:897–902.
7. Frasure-Smith N, Lesperance F. Depression and other psychological risks following myocardial infarction. Arch Gen Psychiat 2003;60:627–36.
8. NHS Centre for Reviews and Dissemination. Cardiac rehabilitation. University of York: Effective Health Care, 1998:4(4).
9. Beswick AD, Rees K, Griebsch I et al. Provision, uptake and cost of cardiac rehabilitation programmes. Improving services to under-represented groups. London: HMSO, 2004.
10. Blumenthal JA, Williams RS, Wallace AG et al. Physiological and psychological variables predict compliance to prescribed exercise therapy in patients recovering from myocardial infarction. Psychosom Med 1982;44:19–27.
11. Department of Health. National service framework for coronary heart disease. London: DoH, 2001.
12. National Institute for Health and Clinical Excellence. MI secondary prevention. Secondary prevention in primary and secondary care for patients following a myocardial infarction. London: NICE, 2007.
13. National Institute for Health and Clinical Excellence. Management of depression in primary and secondary care [also NICE Guidelines for Anxiety]. London: NICE, 2007.
14. Horlick L, Cameron R, Firor W et al. The effects of group education and group discussion in the post myocardial infarction patient. J Psychosom Res 1984;28:485–92.
15. Stern MJ, Gorman PA, Kaslow L. The group counselling vs. exercise therapy study: a controlled intervention with subjects following myocardial infarction. Arch Intern Med 1983;143:1719–25.
16. Rees K, Bennett P, West R et al. Psychological interventions for coronary heart disease. Cochrane Database Syst Rev 2004;(2):CD002902.
17. Writing Committee for the ENRICHD Investigators. Effects of treating depression and low perceived social support on clinical events after myocardial infarction. The Enhancing Recovery in Coronary Heart Disease Patients (ENRICHD) randomized trial. JAMA 2003;289:3106–16.
18. Van Melle J, De Jonge P, Honig A et al. Effects of antidepressant treatment following myocardial infarction. Br J Psychiatry 2007;190:460–6.
19. Glassman AH, O’Connor CM, Califf RM et al.; for the Sertraline Antidepressant Heart Attack Randomized Trial (SADHART) Group. Sertraline treatment of major depression in patients with acute MI or unstable angina. JAMA 2002;288:701–09.
20. Linden W, Phillips M, Leclerc J. Psychological treatment of cardiac patients: a meta-analysis. Eur Heart J 2007;28:2972–84.
21. British Heart Foundation. The national audit of cardiac rehabilitation. British Heart Foundation Annual Report, 2009. Available from: http://www.bhf.org.uk/publications
22. Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand 1983;67:361–70.
23. Beck AT, Ward CH, Mendelson M et al. An inventory for measuring depression. Arch Gen Psychiat 1961;4:561–71.
24. Larsen DL, Attkisson CC, Hargreaves WA, Nguyen TD. Assessment of client/patient satisfaction: development of a general scale. Eval Program Plan 1979;2:197–207.
