The management of acute coronary syndromes (ACS) has changed greatly over recent years. Trial evidence encouraged clinicians to consider early invasive management in high-risk patients and this has created a large clinical burden. We instituted a comprehensive system of nurse-led diagnosis and management of ACS. In-patients are seen by a cardiac outreach nursing team and depending on their risk profile may be managed in a designated acute cardiac unit (ACU) by cardiologists. We also piloted an ‘ACS clinic’ where patients with higher risk are seen within two weeks of discharge. We conducted audits to assess the impact of these new services.
A total of 158 consecutive patients from ACU with unstable angina or non-ST elevation myocardial infarction (NSTEMI) were identified. The in-patient coronary angiography rate was 48%, percutaneous coronary intervention (PCI) rate 15% and coronary artery bypass graft (CABG) rate 4%. The six-month re-admission rate was 28.5%, of whom 44.4% were within one month of discharge. In-patient coronary angiography almost halved the rate of re-admission (20.0% vs. 36.6%; p=0.026). We also audited the first 12 months of the ACS clinic. The six-month re-admission rate was 14.2%, a significant reduction compared with the first audit (p=0.0002). In conclusion, the strategy of nurse-led identification and follow-up of ACS patients promotes effective use of resources and reduces re-admissions.
Introduction
As the management of patients with acute coronary syndromes (ACS) has changed over recent years, so cardiology services have had to adapt their configurations. We instituted a comprehensive system of nurse specialist-led diagnosis and management of ACS and audited the impact of these changes.
The evidence informing our management of ACS patients comes from national registries, such as the prospective registry of acute ischaemic syndrome in the UK (PRAIS-UK)1 and large clinical trials.2-3 The PRAIS-UK registry investigated the management and outcome of 1,046 patients with unstable angina (UA) and non-ST elevation myocardial infarction (NSTEMI) across 56 UK hospitals in 1998. The rates for in-hospital and six-month coronary angiography were 10% and 27%, percutaneous coronary intervention (PCI) 4% and 8%, and coronary artery bypass grafting (CABG) 2% and 7%. Several clinical trials have since demonstrated the benefit of early invasive management, with coronary angiography, followed by revascularisation, where appropriate. The fragmin and fast revascularisation during instability in coronary artery disease II trial (FRISC II)2 demonstrated a significant reduction in the composite end point of death and myocardial infarction (MI) at one year (p=0.005).2 The randomised intervention trial of unstable angina (RITA 3)3 randomised patients with moderate risk and demonstrated a significant reduction in the primary end point of death, MI or refractory angina at four months. There was no reduction in the secondary end point of death and MI until five years (p=0.044).3 Recently, the invasive versus conservative treatment in unstable coronary syndromes (ICTUS) study4 compared an early invasive strategy with a selectively invasive strategy and found no difference in the composite end point of death, MI and re-admission at one year. This was driven by a higher rate of MI in the early invasive group (15% vs. 10%) as a result of the European Society of Cardiology and American College of Cardiology (ESC-ACC) redefinition of MI.
Queens Medical Centre has a large number of admissions of patients with cardiac sounding chest pain, without ST elevation. To correctly identify the higher risk patients, we adopted the thrombolysis in myocardial infarction (TIMI) risk score5 and instituted a cardiac outreach service, consisting of specialist nurses working across the hospital to identify ACS patients.6 A specific ward area, known as the ‘acute cardiac unit’ (ACU) was provided to manage the ACS patients deemed to have a higher risk.
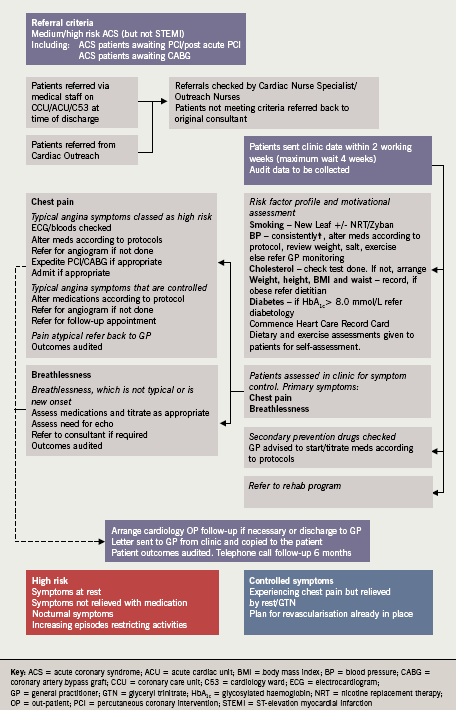
Finally, we piloted a nurse-led ‘ACS clinic’ for 18 months. The aim was for a cardiology sister to identify patients with high and moderate TIMI scores (>2) and to offer them an appointment within two weeks of discharge. In the clinic, the diagnosis, management plan and any symptoms were reviewed with the patient in a 30-minute appointment. Cardiac rehabilitation was offered to all patients. All patients were discussed with a consultant cardiologist. General practitioners and patients received a written summary (figure 1).
We audited the management of ACS patients admitted to the ACU. This was to monitor the outcome of having such a unit and document any improvement upon PRAIS-UK levels of performance. This was followed by an audit of the first year of the ACS clinic service and the six-month re-admission rates for patients seen in the ACS clinic. Chi-square test was used to test for significance in the re-admission rates.
Results
The ACU admissions logbook identified 158 consecutive patients with UA or NSTEMI who were admitted to ACU in the first six months of 2005. Their mean age was 64±13 years with an age range of 34–89 years; 37% were ≥70 years old; 72% were male. In this group of patients, 23% had ST segment depression, 42% T-wave inversion and 19% were normal. Troponin I was raised in 59% of patients. Past history included 23% of patients with diabetes, 56% hypertension, 28% previous MI, 29% current smokers. The rates of use of the standard drugs were aspirin 94%, clopidogrel 64%, enoxaparin 85%, beta blocker 70%, statin 92%, angiotensin-converting enzyme (ACE) inhibitor 65%, intravenous glyceryl trinitrate (GTN) 10%, and glycoprotein (GP) IIb/IIIa 3%.
The rate of in-patient coronary angiography was 48%, revascularisation with PCI was 15% and CABG was 4%. In-hospital mortality was 3%. At six months there was a further 5% coronary angiography, 12% PCI and 10% CABG. The total revascularisation rate was 41%, mortality was 5.1% and re-infarctions 7.6%. The six-month rate of re-admission with further angina was 28.5% (44% within the first month). We re-analysed the data for re-admission and re-infarction based on whether patients had coronary angiography during the index admission and found a reduction in re-admissions (20.0% vs. 36.6%; p=0.026), and re-infarctions (6.7% vs. 9.0%). Finally, we analysed the data based on age; for patients aged 70 years or older (n=59) the rate of in-hospital coronary angiography was 40.7% versus 52.5% for those younger than 70 years (n=99). Total revascularisation in the older group was 39% versus 43%.
The nurse-led ACS clinic reviewed 309 patients in the first year (TIMI score >2). Of these, 44 (14.2%) were re-admitted within six months, a significant reduction compared with the first audit (p=0.0002). A total of 143 (46%) patients from the nurse-led ACS clinic cohort were managed by cardiologists on the ACU and only 18 (12.6%) of them were re-admitted within six months. Furthermore, medications were titrated or altered in 264 (85%) patients. The uptake of rehabilitation was 92%, compared with previous uptake of 60% from departmental audit. As a result of ACS clinic review a further 25 patients were referred for coronary angiography, nine for PCI, two for CABG and four direct admissions were made. A total of 72 (23%) patients were discharged from cardiology follow-up.
Thirty consecutive patients were asked to complete a questionnaire to help us improve the clinic. All (100%) of the patients felt the length of time from discharge to the clinic was about right: 83% preferred to be seen within two weeks by a nurse than to wait four months to be seen by a doctor, and 73% found the letter summary to be informative.
Discussion
Our results illustrate the current state of management and outcomes of patients with UA and NSTEMI in a teaching hospital in the UK. The in-patient management illustrated high use of evidence-based drugs. There was a much higher rate of use of coronary angiography and revascularisation compared with PRAIS-UK. The evidence-based increase in the rate of coronary angiography and revascularisation was documented in more recent registries, such as the Euro Heart survey, which showed an increase in in-hospital coronary angiography from 52% to 63%, PCI from 25% to 37% and CABG from 5.4% to 7.4% between 2000 and 2004.7
The mortality rate of 5.1% at six months was lower than PRAIS-UK (7.4%) while the rate of re-infarctions of 7.6% did not improve since PRAIS-UK (7.3%), probably as a result of the European Society of Cardiology/American College of Cardiology redefinition of MI. Paradoxically, re-admissions have increased since PRAIS-UK (28.5% vs. 17%). This trend towards increased re-admissions was seen in recent data from the global registry of acute coronary events (GRACE) registry (32%), despite a high rate of invasive management (46% for moderate-risk and 51% for high-risk patients).8 Our subgroup analysis confirms that invasive management reduces re-admissions, as was demonstrated in the trials.2,3 Finally, our results show broadly similar rates of revascularisation in the elderly compared with younger patients, which is a change in practice since PRAIS-UK.
Our ACS clinic audit demonstrated that a nurse-led ACS clinic can provide evidence-based care and significantly reduce re-admissions. This is a result of the information, reassurance and support that are provided in the vital early stages, as well as the early surveillance for recurrence of symptoms. The high discharge rate frees up space in hard-pressed cardiology clinics. An appropriate use of urgent re-admission for unstable patients, and change in priority or plan for those whose clinical condition has changed, provides a flexible patient-centred service.
Acknowledgement
This work was presented in part at the British Cardiology Society annual conference, Glasgow, 2007.
Conflict of interest
None declared.
Key message
- A formal nurse-led programme of identification of acute coronary syndrome patients, management in a designated area, appropriate use of invasive investigations and follow-up in a nurse-led specialist clinic all promote effective use of resources, increase uptake of cardiac rehabilitation and reduce six-month re-admission rates
References
1. Collinson J, Flather MD, Fox KA et al. Clinical outcomes, risk stratification and practice patterns of unstable angina and myocardial infarction without ST elevation: Prospective Registry of Acute Ischaemic Syndromes in the UK (PRAIS-UK). Eur Heart J 2000;21:1450–7.
2. Lars Wallentin, Bo Lagerqvist, Steen Husted et al. Outcome at 1 year after an invasive compared with a non-invasive strategy in unstable coronary-artery disease: the FRISC II invasive randomised trial. Lancet 2000;356:9–16.
3. Fox KA, Poole-Wilson P, Clayton TC et al. 5-year outcome of an interventional strategy in non-ST-elevation acute coronary syndrome: the British Heart Foundation RITA 3 randomised trial. Lancet 2005;366:914–20.
4. de Winter RJ, Windhausen F, Cornel JH et al. Early invasive versus selectively invasive management for acute coronary syndromes. N Engl J Med 2005;353:1095–104.
5. Antman EM, Cohen M, Bernink PJ et al. The TIMI risk score for unstable angina/non-ST elevation MI: a method for prognostication and therapeutic decision-making. JAMA 2000;284:835–42.
6. Waterall J. Does optimal drug treatment of acute coronary syndromes depend on management area? Br J Cardiac Nurs 2006;1:247–52.
7. Mandelzweig L, Battler A, Boyko V et al. The second Euro Heart Survey on acute coronary syndromes: characteristics, treatment, and outcome of patients with ACS in Europe and the Mediterranean Basin in 2004. Eur Heart J 2006;27:2285–93.
8. Devlin G, Anderson FA, Heald S et al. Management and outcomes of lower risk patients presenting with acute coronary syndromes in a multinational observational registry. Heart 2005;91:1394–9.
