The fourth annual survey from the British Junior Cardiologists Association (BJCA) reports at a time of restructuring of higher specialist training in the UK. Cardiology faces challenges in training and assessing doctors with a wide array of sub-specialist interests.1 Selection into cardiology, and subsequently into a sub-specialty is being considered. This year’s survey provides timely insight into issues generated by Modernising Medical Careers including sub-specialty training selection, the European Working Time Directive, assessment and academic career pathways. Previous surveys have been noted for providing an authoritative insight into trainees views by national bodies including the British Cardiovascular Society and Royal College of Physicians.(2) Over a third of BJCA members responded to this year’s survey, and the highlights are presented here.
Demographics
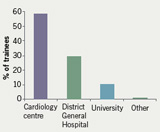
In line with previous years, the proportion of female trainees was 19%. The average age of trainees was 33 years with an even spread of training years represented. The new specialty registrar (StR) grade accounted for only 7% of respondents, a proportion that will increase year on year. Almost two thirds (66%) are married, and over two thirds of those have children. Of note, 92% of respondents’ partners work full-time in the National Health Service (NHS), a figure that has significant implications for NHS child-care provision. Nevertheless, only 7% intend to train flexibly. A higher proportion than in previous years (60%) work in tertiary cardiac centres, with most of the remainder working in District General Hospitals (figure 1).
British Cardiovascular Society
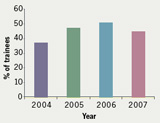
Half of trainees are members of the British Cardiovascular Society (BCS). The majority of trainees felt it would be preferable to link BCS membership to subscriptions for the Joint Royal College Postgraduate Training Board subscriptions in a manner similar to that for medical Royal College subscriptions. Over half (52%) of trainees felt the BCS adequately represented their views. Although 45% of trainees attended the BCS Annual Scientific Conference Trainees’ day at the BCS, this is less than in previous years (figure 2).
On-call patterns and pay-banding
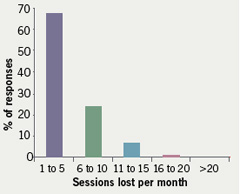
Over a third (36%) undertake 24-hour on-call, 32% full-shift, 23% partial shift and 7% hybrid rotas. The average frequency of on-call was one in eight, and unlike previous years there was no major disparity in rota design across the regions. Despite 24-hour on-call rotas, no trainees received band 3 payments for non-compliant rotas, 25% were in band 2A and 46% band 2B. The proportion of resident on-call rotas has risen to 65% with 62% of trainees on-call for cardiology only (mostly in tertiary centres). The majority of the remainder are on-call for general internal medicine (GIM) only. When on-call, a quarter of respondents have no formal arrangements in place to cover daytime fixed sessions. The effect of the European Working Time Directive (EWTD) continues to affect the availability for training sessions (figure 3).
Intended career paths
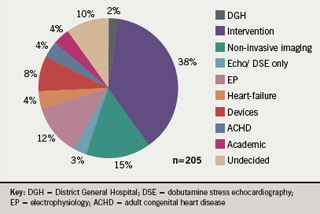
The major change compared with previous years is the rise in popularity of non-invasive imaging with 18.5% of trainees aspiring to some form of imaging-based career. The proportion of trainees wishing to pursue intervention is essentially unchanged at 38% (cf. 39% in 2005).2 Results were broadly similar irrespective of gender and are summarised in figure 4.
Accreditation and GIM
Three-quarters of trainees are currently pursuing dual accreditation with GIM, with a further 7% intending to revert to single accreditation this year. Two-thirds of those dual accrediting would drop GIM if this made no difference to their prospects of securing a suitable consultant post, and a similar proportion of all respondents felt dual accreditation incompatible with achieving adequate sub-specialty training. When asked if they would support increased independence for the BCS from the Royal College of Physicians (RCP), 63% replied that they would support its devolution from the RCP.
Academia
The popularity of academia continues to decline with only 4% intending to pursue an academic career path. Most said it was an unattractive option compared with clinical cardiology while a few cited the pressure to publish. Two-thirds enter higher specialist training having completed a higher degree (MD or PhD), 20% have completed such a degree during time out-of-programme from training, while the majority of the remainder intend so to do. However, only 22% felt that such a degree should be a mandatory requirement of training. Three-quarters (72%) were worried about the effect of Modernising Medical Careers (MMC) on opportunities to do research during training. Notably 60% said they were not usually able to take their research half-day, with two-thirds of these reporting no research time included on their rota, with the remainder committed to clinical duties.
Formal training
The concept of modular training with rotation through sub-specialty areas was extremely popular, supported by 90% of respondents, but only available in a quarter of all regions. Few trainees (22%) have the opportunity to travel to tertiary centres for specialist training unavailable at their hospital, and many comments related to the perceived ‘mismatch’ of post with career aspiration, especially during the first four years of training. Only 9% are advised of rotations more than one year in advance.
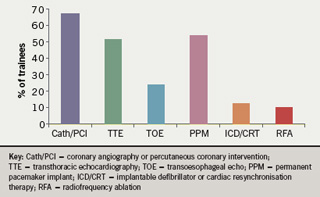
Over half (52%) of trainees were satisfied with current regional arrangements with 60% receiving regular structured training. The majority (88%) would support a compulsory foundation course in general cardiology in years one to three (ST3 to ST5). On average, six cardiology training days are reported as being arranged per region per year (range two to 14). Three-quarters (72%) felt able to attend most of these, and 40% regularly attend local GIM teaching. Half (54%) prefer regional deanery level teaching, with 41% opting for ‘mega-deanery’ level organisation of training courses. Only 52% felt well informed regarding upcoming courses. On average a trainee has a £500 study budget per annum (there was concern that many budgets have been cut by trusts and 6% of respondents report their study budget being cut to zero in the last year). The proportion of trainees participating in regular fixed training sessions is summarised in figure 5.
Less than half felt there was sufficient departmental capacity to train cardiologists in echocardiography, and there were perceived to be inadequate opportunities to train in cardiac magnetic resonance imaging (MRI) and computed tomography (CT) in many regions. Difficulties with access to electrophysiology and grown-up congenital heart disease (GUCH) training were also reported.
Sub-specialty training
Ninety-three per cent of trainees support competitive entry in sub-specialty training with a view to improving quality of training, although it was strongly felt that this should be organised either at local deanery (69%) or ‘mega-deanery’ (20%) level. Two-thirds (68%) would be prepared to move deanery to pursue a specific sub-specialty interest, although only 22% would be prepared to relocate to anywhere in the UK. Most (84%) anticipated a period of out-of-programme fellowship experience would be required to complete their training, and half aimed to do this overseas.
Assessment
There was broad agreement with the aims and ideals of assessment in general, with respondents feeling these were best served by a combination of summative and formative assessments employing a wide range of techniques. Directly Observed Procedural Skill (DOPS) assessments were felt to be especially valuable in cardiology. Two-thirds (64%) felt the Knowledge Based Assessment (KBA) alone should not be used to select for sub-specialty training, and the vast majority felt that it should fall in years three or four (ST5 or ST6). The Record of In-training Assessment (RITA) in its current form was felt to successfully address training issues by only 37% of trainees: previous published reports of trainees’ perceptions of this process have been mixed.3,4
Consultant posts
There was pessimism about the prospects of securing suitable consultant posts with 62% feeling the job market to be less favourable than two years ago. Ability to pursue a sub-specialty interest was the overriding consideration for most (69%) trainees: just over half of trainees would consider a post with one in nine commitment to GIM on-call if it satisfied this criterion.
Other comments
Many issues highlighted in previous studies remain: namely, the difficulties of achieving equitable access to training opportunities across the country, poor provision of training in some sub-specialties and the need for better avenues of communication both to and from trainees and the BCS. Aspects of the new training curriculum appear to have been greeted enthusiastically; in particular the benefits of regular assessment. The need for selection into sub-specialty training is supported by trainees. Trainees are concerned that NHS financial pressures have impacted on study budgets. In relation to MMC, there is disquiet from some in Locum Appointment for Training and similar posts regarding interim arrangements for appointment to the new training system, and uncertainty regarding whether higher training in cardiology will be ‘un-coupled’ from general medical run-through training. As a first step the BJCA’s priority will be to strengthen the trainees’ collective voice at this time of change and opportunity in UK cardiology.
Conflict of interest
None declared.
Acknowledgements
The BJCA wishes to thank the British Cardiovascular Society for their continuing support and in particular Azeem Ahmad and Dilowar Hussain from the British Cardiovascular Society for their assistance with the on-line questionnaire. The full set of results from the 2007 BJCA survey can be found on the BCS website (www.bcs.com).
Damian J Kelly, Secretary, BJCA; Christopher P Gale, President, BJCA; on behalf of the committee.
References
- Gale CP, Gale RP, Batin PD, Wilson J. The European Working Time Directive: potential impact on cardiology specialist registrar training. Br J Cardiol 2007;14:161–3.
- Myerson S. 2005 BJCA survey of cardiology trainees. Br J Cardiol 2006;13:102–04.
- Bache J, Brown J, Graham D. In-training assessment for specialist registrars: views of trainees and trainers in the Mersey Deanery. J R Soc Med2002;95:612–13.
- Pearce I, Royle J, O’Flynn K, Payne S. The record of in-training assessments (RITAs) in urology: an evaluation of trainee perceptions. Ann R Coll Surg Engl 2003;85:351–4.
