The majority of patients with hypertension are treated in primary care and well controlled. Typically, a practice will achieve about 80% control as judged against the Quality Outcome Framework (QOF). The QOF only requires a practice to reach a target of 70%. A practice will need to control the blood pressure of about 18% of their patients and therefore about 3.5% of the practice population will not be controlled. Too many to refer to secondary care and therefore the practice needs a strategy to try and improve control in-house and to identify those in greatest need of referral.1
1. Check that the measurement is correct
Ensure that they really are poorly controlled by resting the patient for 10 minutes, with the cuff in place to discourage them from standing, before taking at least two measurements, one to two minutes apart. Feel the radial pulse because in arrhythmias such as atrial fibrillation automatic sphygmomanometers are inaccurate and therefore traditional devices such as mercury sphygmomanometers must be used. People aged over 80 years and some diabetics may have postural hypotension. This is where the systolic blood pressure drops 20 mmHg on standing or they may have postural symptoms.2 Having made that diagnosis you should treat them using the standing blood pressure as the target and use that measurement for your QOF report.
Consider loaning the patient an automatic sphygmomanometer to carry out a series of home measurements. A list of recommended machines is available at www.bhsoc.org. Take an average of their readings and add 10/5 mmHg to account for the difference between home measurement and clinic measurement. Some practices may have ambulatory sphygmomanometers available but in general terms the scale of workload makes them impractical.
2. Check compliance, establish concordance
Warning the patient about side effects will often help to avoid them stopping new prescriptions, especially if you point out that many side effects are temporary. As a routine you should ask patients when they last took their medication. You should be familiar with your computer system’s prescription monitoring system and check that they have collected sufficient amounts to have a continuous supply.
Seek agreement with the patient about their prescription and make sure they are doing this for themselves and not you! Many patients feel guilty about poor compliance and this is why they hide this from their practitioner.
3. Encourage weight loss and salt reduction
A weight loss of about 10 kg will result in a systolic blood pressure drop of up to 10 mmHg, depending on the level of a patient’s obesity. Inform the patient of this fact and explain to them that most people can lose that amount of weight relatively easily. If they put it on again you can always encourage them to do it on an annual basis.
A reduction in salt intake will result in a significant reduction in blood pressure and will maximise the blood pressure-lowering effect of many classes of drugs such as angiotensin-converting enzyme (ACE) inhibitors, angiotensin receptor blockers, renin inhibitors, beta blockers and verapamil.3 Inform the patient that most of the salt is hidden in food and encourage them to visit www.salt.gov.uk for more information. Inform the patient that you can monitor how well they do by regularly measuring 24-hour urinary sodium excretion.
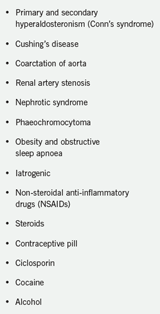
4. Stop drugs that raise blood pressure
Non-steroidal anti-inflammatory drugs and the combined oral contraceptive pill are drugs that commonly cause a rise in blood pressure. Ciclosporin has a hypertensive effect and you might bring this to the attention of the specialist prescribing it and ask if an alternative could be used. Drugs of abuse should also be considered such as cocaine and alcohol. In such cases, addiction treatment is the only solution to the problem.
5. Maximise medication using ACD
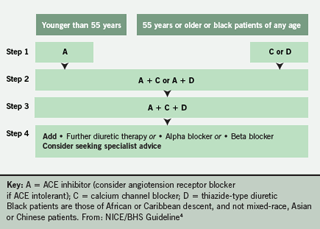
The National Institute of Health and Clinical Excellence (NICE)/British Hypertension Society (BHS) ACD table should be rechecked to make sure the patient has tried the logical combination.4 In particular they should be on an ACE inhibitor or angiotensin receptor blocker, plus a calcium channel blocker and a thiazide or thiazide-like diuretic. Having established that they are on three drugs consider step 4 of the algorithm and add a further diuretic, such as spironolactone, an alpha blocker or a beta blocker.
6. Spironolactone
It is estimated that 21% of resistant hypertensive patients have hyperaldosteronism.5 Patients with resistance and a low serum potassium are particularly likely to have this problem. The diagnosis can sometimes be confirmed by measuring the renin to aldosterone ratio but this is not available to doctors in many areas and can provide false negatives. A low dose of spironolactone, half a 25 mg tablet, may well be very effective. Spironolactone is not licensed for hypertension but is licensed for hyperaldosteronism. The Anglo-Scandinavian Cardiac Outcomes Trial (ASCOT) included a spironolactone arm.6 Amiloride and eplenerone may have a similar effect. Urea and electrolytes should be monitored regularly and you should warn patients to stop these drugs temporarily if they are suffering diarrhoea or are dehydrated.
Watch for hypotension and often you may have to reduce the doses of the ACD drugs because the spironolactone is so effective. Conn’s syndrome is hyperaldosteronism secondary to either an adrenal gland adenoma or to bilateral adrenal hyperplasia, usually found by computed tomography (CT) scanning.
7. Establish that better control is required
Make sure that the patient is willing to take further medication and wants more investigation. You should have a clear, written policy in your practice as regards maximal treatment of blood pressure based on the BHS guidelines. An example of a policy has previously been published in this journal.7 The patient’s opinion should be taken into account and recorded before using the exception code.
8. Ensure that other preventive measures are in place
Risk factors cluster so if you cannot fully control somebody’s hypertension you should cover the other risk factors. If the patient has cardiovascular disease, diabetes or chronic kidney disease they should have all other relevant preventive measures in place. A prevention screen should have been carried out, as for all other patients, and if their cardiovascular risk is equal to or greater than 20% they should be considered for statin therapy. The new NICE guidelines also tell us to use statin therapy in people over 74 years who smoke or have hypertension.8,9
9. Are there any investigations that might be useful for the specialist?
The specialist needs to have as many facts to hand as possible when they see the patient. If they have to arrange tests it just delays implementing treatment. You should have a good idea of the sort of tests your local specialist might like to have done. As previously mentioned, a prevention screen, including lipids and blood glucose are important. Have you carried out routine tests such as microalbuminuria, 24-hour urine for sodium, urea and electrolytes, estimated glomerular filtration rate (eGFR), serum urate, thyroid-stimulating hormone and gamma gluteryl transferase?
All hypertensive patients need a routine electrocardiogram (ECG) and a copy should ideally be sent with the referral. An echocardiogram would be useful when left ventricular hypertrophy is seen on the ECG. Consider ultrasound of the kidney when patients have evidence of kidney impairment or to rule out polycystic kidney disease. Renal artery stenosis (RAS) should be suspected in young resistant hypertensives and in patients who have peripheral vascular disease or deteriorating renal function when using ACE inhibitors. RAS will sometimes result in a unilateral small kidney on ultrasound. Consider other causes of secondary hypertension and relevant tests such as a urinary vanillylmandelic acid (VMA) in young anxious patients. (See table of possible causes of secondary hypertension.)
10. Are you referring to the correct consultant?
You may have a local hypertension clinic and it is obvious where you should refer, but not all general practitioners have such a local clinic. Where there is no specialist clinic it is common to refer to the local cardiologist. But does your local cardiologist have any specialist training or an interest in hypertension? Many do not and may actually have less overall experience of managing hypertension than you do. Patients with renal impairment may benefit from seeing a renal physician and many of them do have a specific interest in hypertension. There may be a local vascular or stroke physician with an interest and some elderly care physicians have such an interest. Many general practitioners with a special interest (GPSIs) have completed training in hypertension. Choose and book may be your best source of information but you could also see if the specialist is a member of the BHS, holds a European Hypertension Specialist certificate or is associated with a European Hypertension Centre of Excellence (see www.bhsoc.org).
References
- Singer DRJ, Edmunds M, Cappuccio FP. Feasibility study of a virtual approach to cardiovascular risk management. J Hypertens 2008;26(suppl 1):S299.
- Williams B, Poulter NR, Brown MJ et al.; British Hypertension Society. Guidelines for management of hypertension: report of the fourth working party of the British Hypertension Society, 2004-BHS IV. J Hum Hypertens 2004;18:139–85.
- Cappuccio FP. Salt and cardiovascular disease. BMJ 2007;334:859–60.
- National Institute for Health and Clinical Excellence. CG34 Hypertension – NICE guideline. London: NICE, June 2006.
- Douma S, Petidis K, Doumas M. Prevalence of primary hyperaldosteronism in resistant hypertension: a retrospective observational study. Lancet 2008;371:1921–6.
- Dahlof B, Sever P, Poulter N. Anglo Scandinavian Cardiac Outcomes Trial – Blood Pressure Lowering Arm (ASCOT-BPLA). Lancet 2005;366:895–906.
- McCormack T, Davis M. The definition of maximally tolerated blood pressure treatment. Br J Cardiol 2005;12:156–60.
- National Institute of Health and Clinical Excellence. CG67 Lipid modification – NICE guideline. London: NICE, May 2008.
- Cappuccio FP. Controversies in NICE guidance on lipid modification for the prevention of cardiovascular disease. BMJ 2008;336:1248–9.
