In June 2004 the Department of Health made a commitment to reduce waiting times from GP referral to hospital treatment to less than 18 weeks by 2008. Patients with chest pain are often now seen within two weeks thanks to the success of rapid-access chest pain clinics. Around 10–25% of these patients are referred for diagnostic coronary angiography (CAG) and of these, about 30% require percutaneous coronary intervention (PCI) to treat coronary stenoses. Conventionally, UK practice has been that such patients occupy two waiting lists: one for the CAG, which is often performed by a non-interventional cardiologist, and one for the PCI. This pathway makes achieving the 18-week target challenging. We introduced a new care pathway whereby all elective chest pain patients referred for CAG to one of the interventional cardiologists were listed for a standby coronary angiogram (SBCA), during which if PCI was indicated then it was performed immediately. We present the results of an audit of 102 consecutive patients since this pathway was introduced that demonstrates one method of achieving the 18-week target for this group of patients. This can now be further refined by aiming to achieve a higher proportion of day-case PCI cases.
Introduction
The National Health Service (NHS) Improvement Plan stated that by 2008 no one would wait longer than 18 weeks from GP referral to hospital treatment.1 This is, therefore, currently a key area of focus for the Department of Health and a major challenge for hospital trusts that provide cardiac services. ‘Chest pain’ is the most common indication for out-patient referral to cardiology. The delay between referral and out-patient review has been successfully reduced in our institution and across the UK by the rapid-access chest pain clinics (RACPC), with 96% of referrals nationwide being seen within two weeks.2 In this centre, up to 20% of the patients assessed in RACPC are referred for diagnostic coronary angiography (CAG). Interestingly, a recent survey of 8,762 patients assessed in six RACPC across the UK reported an overall angiography rate of 7%,3 although of the patients who had a primary event (coronary-related death plus acute coronary syndrome) at median follow-up of 2.6 years in that study, 32% were from the group labelled as ‘non-cardiac’ at RACPC
At angiography, if significant coronary narrowings are identified in these patients one of the three management options is percutaneous coronary intervention (PCI). Currently in the UK, most elective patients with chest pain are listed for CAG, which is then performed as an isolated procedure. Patients in whom the treatment of choice is PCI are then listed for a separate admission via a second waiting list. The inherent delay in this pathway means that achieving the 18-week target will be challenging. Current practice persists for the following reasons. First, there is resistance to preparation of patients for the uncertainty of a PCI procedure that may or not happen at the time of CAG. This is despite the fact that most non-elective patients with acute coronary syndromes are already managed using the standby coronary angiogram (SBCA) system in the UK. Second, The National Tariff and Payment by Results encourages this practice because a hospital trust currently receives two separate tariffs (one for CAG, one for PCI) if the procedures are performed on different occasions, but only one tariff if cases were to proceed directly to PCI (i.e. no payment is made for the diagnostic angiogram).
The aim of this project was to assess the feasibility of all CAG patients who were referred to a single interventional cardiologist being managed by SBCA and to analyse the outcome of such patients in terms of their speed of access to PCI.
Methods
In 2005, one high-volume interventional cardiologist (NC), who performs 350 to 400 PCI per year,4 changed his practice so that the majority of his elective patients with chest pain were listed for a SBCA rather than just for CAG. Patients were informed, both by letter and in person, that should significant coronary narrowings suitable for PCI be demonstrated at the CAG then the plan would be to proceed directly to that procedure. This mirrors a well-established management plan already offered to most in-patients with acute coronary syndromes. Consent was undertaken accordingly and the patients were given 600 mg of clopidogrel at least six hours prior to their procedure. Lists were made up according to estimated conversion rates to PCI: thus, if CAG was treated as one unit of cath lab time, the SBCA cases were allocated 1.5 units in mixed lists. This change in practice was linked prospectively to the intention to audit formally after 100 consecutive patients, in agreement with our local implementation team. We therefore designed an audit to assess this practice to calculate current waiting times and identify factors that lead to delays. Our aim was to test the hypothesis that the novel SBCA system meant patients could achieve the 18-week waiting time target.
We performed a retrospective case note review of prospectively identified patients who had their procedure between November 7th 2005 and February 14th 2007 (15 months), cross-checked from the cardiac catheter laboratory lists. A proforma was designed to collect appropriate data and this was then transposed into a Microsoft Access database.
Results
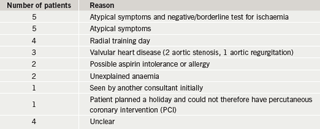
Over the study period, 253 patients were identified from the cardiac catheter laboratory log for elective (NC) lists. Of these, 113 were in-patient cases and were therefore excluded. All of the remaining 140 patients’ notes were obtained and analysed. After excluding patients listed for definite elective PCI, emergency cases and those patients under ongoing follow-up, 102 patients were identified for use in the study. In this patient cohort, 75 were listed for SBCA and 27 for CAG only, as described in table 1. One patient chose not to have the procedure by SBCA.
Demographics
Of the total cohort (102 patients), average age was 64 years. Sixty-seven (66%) of the patients were male. Fifty-nine (58%) were initially seen in the RACPC, 39 (38%) in the out-patient clinic (OPC) and two (2%) in pre-clerking. Sixty-two (61%) of the angiograms were performed via the femoral artery and 40 (39%) via the radial artery.
Of the 75 SBCA patients, the average age was 63 years old. Forty-seven (63%) of the patients were initially seen in the RACPC, 26 (35%) in the OPC and two (3%) in pre-clerking.
Outcome
Of the 102 patients, 50 (49%) required medical management or had normal coronary arteries; 18 (18%) were referred for coronary artery bypass grafting (CABG); 30 (29%) had PCI and four (4%) were referred for aortic valve replacement (two with additional CABG). In seven (7%) cases a pressure wire was used to aid decision-making: five went on to have medical management, one CABG and one PCI. In three (3%) cases intravascular ultrasound (IVUS) was used during the procedure (one had CABG, two had PCI).
Of the 75 SBCA patients, 36 (48%) had medical management, 23 (31%) had PCI and 16 (21%) were referred for CABG. The mean length of hospital stay was 0.92 days for the diagnostic SBCA group and 1.48 days for those SBCA patients who had PCI.
Waiting times
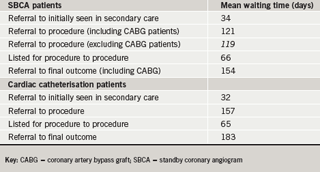
The mean waiting time from referral to initial secondary care review was nine days for patients seen in the RACPC and 67 days for those seen in OPC. The waiting times for patients at each stage of their care pathway are shown in table 2. Four of the 75 patients listed for SBCA cancelled or did not attend their appointment and were therefore excluded from further analysis of waiting times (they would not be counted in the 18-week waiting time – see the Updated 18-week Clock Rules: section 31).5 There was a substantial wait for patients referred for CABG (mean 251 days) and this, therefore, will represent a major challenge for the 18-week target that this project has not addressed. The mean time from referral to outcome for the SBCA cohort, including patients that went on to have CABG was 149 days. After excluding those patients referred for CABG, the mean time from referral until treatment for those patients listed for SBCA was 119 days, hence within the 126 days needed to achieve the 18-week waiting time.
Long waiters
Twenty-six patients waited 196 days or greater from original referral to SBCA or CAG, range 196 to 480 days. The majority of these patients were referred for another investigation prior to being listed for angiography. These included myoview nuclear medicine scans (11 patients, average wait 145 days), stress echocardiography (two patients, average wait 107 days) and stress magnetic resonance imaging (MRI) (two patients, average wait 103 days). Patients also waited an average of 67 days to be seen in the OPC, adding to the delay if they were reviewed following one of the above investigations.
Discussion
This project demonstrates the feasibility of listing elective patients being investigated for possible angina as SBCA rather than diagnostic angiography. Our data show that 23 of 75 (31%) managed in this way did undergo PCI, while 36 of 75 (48%) had medical treatment and 16 of 75 (21%) were referred for CABG. Importantly, this means that 69% of this group could be managed, as in any routine practice, as day-case angiograms, even though they had been prepared for PCI. Only the 31% proceeding to PCI may need to stay overnight, although at least some of these patients could be treated as day cases as well, especially if the procedure was performed via the radial artery.
There are several advantages of this change in care pathway. First, this process removes the separate wait that is incurred in listing patients for CAG and then PCI. This is more efficient and facilitates achieving the 18-week target for PCI patients, without disadvantaging those patients whose final management choice is either medical treatment or CABG surgery. Second, this process, if coupled to a robust day-case PCI programme, could optimise use of day-case facilities and reduce admission rates to other cardiology beds. Third, the process, if explained thoroughly, is popular with patients, who preferred to have all their possible treatment in ‘one go’. Fourth, this care pathway avoids the unpopular and unweildy bureaucracy that is evoked by Patient Choice. It is our experience and that of other front-line healthcare staff that patients very rarely choose not to continue to be looked after by a hospital and team with whom they have become familiar. The motivation to choose another unit is generally related to speed of access, the very issue that this new care pathway addresses. Fifth, if this care pathway were to be widely accepted, most chest pain patients would have their original angiographic assessment and management decision-making by an interventional cardiologist. This has not only been previously shown to increase PCI activity relative to CABG referral,6 but also allows instant assessment of equivocal coronary disease by pressure wire or IVUS, which were used in 10% of this cohort. Sixth, this care pathway would save money for the total local healthcare economy by reducing the total admission rate. Such a shift would advantage commissioning bodies and disadvantage the hospital trust (see below).
This new care pathway also has disadvantages and limitations. First, all such patients would require more preparation prior to their initial procedure. Thus, they need to be educated about the concept of the uncertainty of SBCA and all need to be given clopidogrel loading doses prior to their procedure, which could result in unexpected bleeding in a small number. Second, the cath lab listing needs to be done more carefully in order to allow enough time for around 30% of such patients to receive PCI as well as CAG. Such perceived problems have actually already been readily overcome in the case of most in-patients undergoing CAG as SBCA around the UK! Third, the hospital trust would be paid for only one procedure (PCI instead of CAG+PCI) on the patients proceeding to PCI. Preliminary discussions with representatives of primary care trusts (PCTs) at local implementation team meetings suggest that there would be interest in removing this financial disincentive if our trust (Southampton University Hospitals Trust) could demonstrate waiting time advantage, particularly because the process as a whole is likely to save commissioners money by cutting down the total number of admissions for this cohort. Fourth, the efficiency of this concept, at a time when many regional cardiac centres have seen a downturn in their elective PCI referrals, because of increasing numbers of district general hospital catheter labs, threatens the diagnostic CAG practice of some non-interventional cardiologists, especially those within regional units. Given (a) that the process is more efficient, (b) the advantage of being able to perform pressure wire or IVUS assessment of equivocal lesions instantly, and (c) the data relating to differences in interpretation of angiography, we feel that this potential change in practice is justified.
In conclusion, this study demonstrated the feasibility of SBCA assessment of a cohort of elective chest pain patients. This care pathway shift facilitates achieving the 18-week target for PCI, particularly when coupled with RACPC and day-case PCI. The pathway could be made more robust by removing the financial disincentive incurred by current reimbursement arrangements for SBCA PCI, which are illogical, but will represent a threat to the roll out across the UK. We recommend that, particularly in the light of the emerging capacity of elective PCI space in large regional centres, elective diagnostic CAG for patients with chest pain is directed at interventional cardiologists and performed as SBCA procedures.
Conflict of interest
None declared.
Key messages
- Performing all angiograms for out-patients with chest pain as standby procedures can facilitate achieving the 18-week pathway
- Standby angiograms allow for improvements in efficiency, although patient preparation is more complex
- Standby angiography allows for diagnostic certainty with 10% of cases having definitive pressure wire or intravascular ultrasound (IVUS) assessment to optimise management there and then
- These data are consistent with the argument that more diagnostic angiography should be done by interventional cardiologists on a standby basis, although reimbursement by tariff will need to reflect activity
References
- Department of Health. The NHS improvement plan. Available from: http://www.dh.gov.uk/publications
- Boyle RM. Value of rapid access chest pain clinics. Heart 2007;93:415–16.
- Sekhri N, Feder G, Hemingway H, Timmis A. How effective are rapid access chest pain clinics? Prognosis of incident angina and non-cardiac pain in 8762 consecutive patients. Heart2007;93:458–63.
- Dawkins KD, Gershlick T, de Belder M et al.; Joint Working Group on Percutaneous Coronary Intervention of the British Cardiovascular Intervention Society and the British Cardiac Society. Percutaneous coronary intervention: recommendations for good practice and training. Heart 2005;91(suppl 6):vi1–vi27.
- Updated 18 Week Clock Rules. Available from: http://www.18weeks.nhs.uk/cms/ArticleFiles/kk4lzf45hu10e0iaaa54bl4523082005112550/Files/061211UpdatedRulesfinal.doc
- Tryfonidis M, Prendergast B, Curzen N. Are waiting times for coronary artery bypass graft surgery longer than they should be? Implications of the NICE guidelines for coronary artery stents. Br J Cardiol: Acute & Interventional Cardiology 2002;9(1):13–17.
