Angiography of internal mammary artery (IMA) grafts continues to be a common indication for upfront femoral access. This is particularly the case for bilateral pedicled IMAs, or when the left radial artery has been grafted. While the right radial artery is ideally suited in these situations for cannulation of the right IMA, accessing the left IMA (LIMA) by this route is often perceived as challenging and for ‘radial evangelists’ only. We describe a case series showing a simple technique for selective cannulation of the LIMA from the right radial artery using a single catheter that provides sufficient backup for percutaneous coronary intervention (PCI).
Introduction
While many in the interventional cardiology community consider the debate of routine radial versus femoral access for coronary angiography to be all but over,1-5 there, nonetheless, continues to be a wide variation in the uptake of transradial access worldwide.6,7 Even putting the preferences of transradial enthusiasts aside, it also seems that patients who have had experience of both access routes prefer use of the radial artery.8
Nonetheless, femoral access undoubtedly continues to remain relevant in situations such as large bore and complex intervention, the need for mechanical support devices, and structural intervention. One such traditional bastion of the femoral approach is internal mammary artery (IMA) graft angiography. Although the ipsilateral radial artery provides a direct route to an IMA graft, the advantage of this route is lost when bilateral IMA grafts need to be visualised, or when the required radial artery has been used for grafting. Given the superior outcomes of arterial over vein graft revascularisation,9,10 we can only assume that the number of these patients presenting for angiography will increase in the future.
We present a case series illustrating a simple technique for selective angiography of an IMA graft from the contralateral radial artery. This technique demonstrates that cardiologists do not necessarily need to resort to routine femoral access when the ipsilateral radial artery is not available.
Case 1
A 64-year-old man presented to the cardiology clinic six years following coronary artery bypass grafting (CABG, left internal mammary artery to left anterior descending [LIMA-LAD]; left radial artery to obtuse marginal [LRA-OM]; saphenous vein graft to right coronary artery [SVG-RCA]) with increasing angina and shortness of breath refractory to medical therapy. His background included a previous stroke, hypertension, chronic kidney disease stage 3, hyperlipidaemia and being an ex-smoker.
He was brought to the catheter lab for coronary restudy. His LRA had been used for grafting, therefore, the right radial artery was cannulated with a 6-French sheath. A JL3.5 6-French guide catheter (Launcher; Medtronic, Minneapolis, MN, USA) was used for native coronary angiography. This showed that the LAD was now severely diseased distal to the graft insertion (figure 1A, video 1). A decision was made at this stage to proceed to percutaneous coronary intervention (PCI) to his native LAD via the LIMA graft.
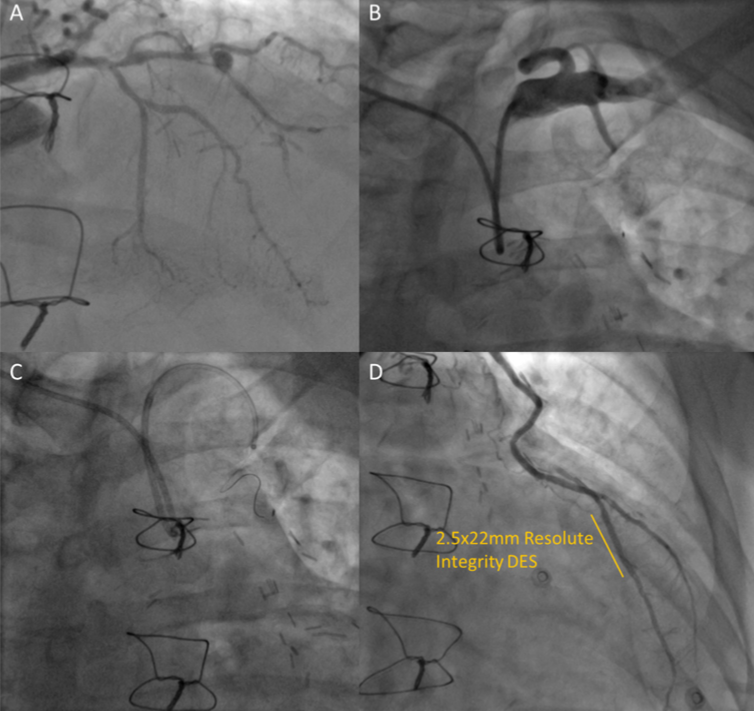
The guide catheter was withdrawn to the aortic arch and rotated cranially, allowing advancement of a 0.035 in 150 cm J-tip wire (Cordis, Milpitas, CA, USA) into the left subclavian artery. Advancement of the catheter over this wire was followed by sub-selective angiography revealing the origin of the LIMA (figure 1B). The graft was then wired with a Pilot 50 wire (Abbott Vascular, Chicago, IL, USA), which allowed railroading of a 6-French GuideLiner (Teleflex Inc., Wayne, PA, USA) for selective cannulation of the LIMA (figure 1C, video 2). The vessel was very tortuous and, therefore, a second Pilot 50 wire was advanced, however, this led to no flow within the mid-vessel, which was treated by stenting with a 3.0 × 33 mm Resolute Integrity (Medtronic). The mid-LAD was pre-dilated with 2.0 mm semi-compliant balloon, stented with a 2.5 × 22 mm Resolute Integrity (Medtronic), and then followed by post-dilation to 15 atm to a good final result (figure 1D, video 3).
Case 2
A 63-year-old man presented with shortness of breath and inducible ischaemia in the LAD territory on stress echocardiography, despite CABG including a LIMA to LAD graft the year before. During the operation there had been difficulty in grafting the LIMA, as the vessel was reportedly fragile, part occluded and calcified.
He attended for elective coronary angiography where his left radial was found to be occluded. His right radial artery was, therefore, cannulated with a 6-Fr sheath. The LIMA was accessed by using a JL3.5 6-Fr guide catheter to engage the left subclavian artery. A 6-Fr GuideLiner was then advanced to the origin of the LIMA with the aid of a Pilot 50 wire allowing selective angiography (figure 2A).

Case 3
A 68-year-old man had undergone CABG over 10 years ago with LIMA-OM, RIMA-LAD, SVG-first diagonal (D1) and SVG-RCA. Both vein grafts were known to be occluded. He had poor left ventricular (LV) systolic function, which was initially thought to be due to a significant ventricular ectopic burden, however, this persisted despite successful radiofrequency ablation. He was, therefore, admitted for a coronary restudy.
His right radial artery was cannulated with a 6-Fr sheath. After selective cannulation of the RIMA and native RCA, a JL3.5 6-Fr guide catheter was advanced. After the native left coronary artery (LCA) was visualised, as previously, the guide catheter was rotated to engage the left subclavian artery and a GuideLiner was deep‐seated into the LIMA over a Pilot 50 guidewire. Further graft angiography two years later, prior to transcatheter aortic valve implant, utilised the same technique from the left radial artery with the help of a Balance Middleweight guidewire (Abbott Vascular, Chicago, IL, USA) (figure 2B).
Case 4
A 63-year-old man, who had already required stenting to his SVG-RCA vein graft only one year after CABG, presented again with recurrent angina. Stress echocardiography showed inducible ischaemia in the LAD territory, therefore, he attended for day case coronary angiography.
A 6-Fr sheath was used to cannulate his right radial artery. After native and vein graft angiography were completed, a JL3.5 6-Fr guide catheter easily cannulated the left subclavian and allowed wiring of the LIMA with a Pilot 50 wire. In this case, we advanced a 3-Fr Slip-Cath infusion catheter (Cook Medical, Bloomington, IN, USA) down the graft, which allowed a superselective angiogram of the LIMA to OM (figure 2C).
Discussion
Patients with previous CABG surgery are common, and the left radial artery should be the access route of choice to the LIMA in most cases unless the radial artery has been grafted, or bilateral IMA grafts need to be visualised. However, angiography of the LIMA from the contralateral side is not a new concept,11-15 and in fact pre-dates the recent shift to radial access, having been proposed back in the era of brachial artery cannulation.16 PCI via this route, however, is less well described.17 The need to achieve co-axial alignment to deliver equipment to the vessel, combined with the loss of support from a tortuous approach, make it tempting to consider resorting to a femoral approach. However, iliac and aortic tortuosity and calcification present their own challenges, especially in the elderly, and we should be able to offer the benefits of radial access to these patients without defaulting to femoral puncture.
Nonetheless, the individual variations in arterial anatomy that the operator must navigate from the right radial artery will often not be known prior to the procedure. Even after negotiating right subclavian and aortic tortuosity and wiring the left subclavian, the takeoff of the LIMA will show significant variation and often prevent selective cannulation with the initial catheter of choice. Radial catheter exchange may then be poorly tolerated by the patient or provoke spasm, and often lead to the wire prolapsing back into the aorta, although techniques to trap the wire in the contralateral arm or wrist have been described to prevent this.18,19 In our case, the use of a ‘mother and child’ system with a monorail guide extension removes the need for catheter exchange, and provides the co-axial alignment and the backup necessary to enable delivery of equipment to the LIMA or the LAD.
Our centre performs over 200 graft angiography cases a year, yet the number of these cases without ipsilateral radial access are small. Although no major adverse events were seen in our cohort, the known association of increased fluoroscopy time with stroke (presumably as a surrogate of increased catheter manipulation in the aorta), should be taken into account when learning an unfamiliar technique in an infrequently encountered situation. Perhaps due to the durability of IMA grafts, there are scarce data available on IMA PCI, but registry data do also suggest that LIMA intervention is associated with worse procedural outcomes versus vein graft PCI.20 We, therefore, suggest that this technique is reserved for experienced interventionalists with capacity for bail-out PCI if complications arise, as seen in case 1.
The challenge in the coming years for interventional cardiologists may well be in maintaining femoral access skills, as the trainees of today are raised on the mantra of ‘radial first’. As transradial access continues to evolve, femoral access has also moved beyond blind puncture of the artery. As a minimum, fluoroscopy-guided puncture, but ideally the use of real-time ultrasound and micropuncture devices should be utilised to minimise potential bleeding risks. Despite being well supported by randomised evidence, these techniques remain far from widespread in cardiac catheter labs.21
Conclusion
IMA graft angiography is possible via the contralateral radial artery, and the support needed for PCI can be provided from a single standard guide catheter using a ‘mother and child’ technique with monorail guide extension. We suggest that when the ipsilateral radial artery is not available that experienced interventionalists consider the contralateral radial artery as an alternative to femoral access.
Key messages
- The use of arterial conduits for surgical revascularisation can pose a challenge in both vascular access and graft cannulation at subsequent angiography
- A modified ‘mother and child’ technique with monorail guide extension allows selective internal mammary artery (IMA) cannulation from the contralateral radial artery without catheter exchange
- Using this technique, graft angiography patients do not need to be subjected to the increased risks of femoral over radial access
Conflicts of interest
None declared.
Acknowledgements
We thank Mary Keal, Dinesh Sajnani and Stephen Brecker for their support in developing new techniques at our catheterisation laboratory.
Consent
Patient consent for publication was obtained in all cases.
Supplementary material
Video 1. Angiography of the left system. The distal LAD is difficult to visualise from this view due to competitive flow. Available from: https://1drv.ms/v/s!Ail45xIWPE2z1ml3pbiv1sCzn_dj
Video 2. A GuideLiner has been deep seated into the LIMA allowing better visualisation of the severe disease in the distal LAD. Available from: https://1drv.ms/v/s!Ail45xIWPE2z1m2-fZuVwavwCJBs
Video 3. Final angiographic result following PCI. Available from: https://1drv.ms/v/s!Ail45xIWPE2z2hN0mFUjH366SIMM
References
1. Ferrante G, Rao SV, Jüni P et al. Radial versus femoral access for coronary interventions across the entire spectrum of patients with coronary artery disease. JACC Cardiovasc Interv 2016;9:1419–34. https://doi.org/10.1016/j.jcin.2016.04.014
2. Kolkailah AA, Alreshq RS, Muhammed AM, Zahran ME, Anas El-Wegoud M, Nabhan AF. Transradial versus transfemoral approach for diagnostic coronary angiography and percutaneous coronary intervention in people with coronary artery disease. Cochrane Database Syst Rev 2018;4:CD012318. https://doi.org/10.1002/14651858.CD012318.pub2
3. Valgimigli M, Frigoli E, Leonardi S et al. Radial versus femoral access and bivalirudin versus unfractionated heparin in invasively managed patients with acute coronary syndrome (MATRIX): final 1-year results of a multicentre, randomised controlled trial. Lancet 2018;392:835–48. https://doi.org/10.1016/S0140-6736(18)31714-8
4. Hamon M, Pristipino C, Di Mario C et al. Consensus document on the radial approach in percutaneous cardiovascular interventions: position paper by the European Association of Percutaneous Cardiovascular Interventions and Working Groups on Acute Cardiac Care** and Thrombosis of the European Society of Cardiology. EuroIntervention 2013;8:1242–51. https://doi.org/10.4244/EIJV8I11A192
5. Jolly SS, Yusuf S, Cairns J et al. Radial versus femoral access for coronary angiography and intervention in patients with acute coronary syndromes (RIVAL): a randomised, parallel group, multicentre trial. Lancet 2011;377:1409–20. https://doi.org/10.1016/S0140-6736(11)60404-2
6. Bradley SM, Rao SV, Curtis JP et al. Change in hospital-level use of transradial percutaneous coronary intervention and periprocedural outcomes: insights from the national cardiovascular data registry. Circ Cardiovasc Qual Outcomes 2014;7:550–9. https://doi.org/10.1161/CIRCOUTCOMES.114.001020
7. Valle JA, Kaltenbach LA, Bradley SM et al. Variation in the adoption of transradial access for ST-segment elevation myocardial infarction. JACC Cardiovasc Interv 2017;10:2242–54. https://doi.org/10.1016/j.jcin.2017.07.020
8. Kok MM, Weernink MGM, von Birgelen C, Fens A, van der Heijden LC, van Til JA. Patient preference for radial versus femoral vascular access for elective coronary procedures: the PREVAS study. Catheter Cardiovasc Interv 2018;91:17–24. https://doi.org/10.1002/ccd.27039
9. Gaudino M, Puskas JD, Di Franco A et al. Three arterial grafts improve late survival. Circulation 2017;135:1036–44. https://doi.org/10.1161/CIRCULATIONAHA.116.025453
10. Neumann F-J, Sousa-Uva M, Ahlsson A et al. 2018 ESC/EACTS guidelines on myocardial revascularization. Eur Heart J 2019;40:87–165. https://doi.org/10.1093/eurheartj/ehy394
11. Suh WM, Kern MJ. Coronary and bypass graft angiography via the right radial approach using a single catheter. J Invasive Cardiol 2012;24:295–7. Available from: https://www.invasivecardiology.com/articles/coronary-and-bypass-graft-angiography-right-radial-approach-using-single-catheter
12. Patsilinakos S, Tsinivizov P, Papadakis E, Kyriakopoulos V, Marinos S, Poulimenos L. Left internal mammary arterial angiography via the right radial approach: description of technique, single-centre experience, and brief review of the literature. Hellenic J Cardiol 2015;56:522–6. Available from: https://www.hellenicjcardiol.org/archive/full_text/2015/6/2015_6_522.pdf
13. Valsecchi O, Vassileva A. Safety and feasibility of selective angiography of left internal mammary artery grafts via right transradial approach. Indian Heart J 2010;62:255–7.
14. Kwang Soo Cha, Moo Hyun Kim, Hung J-S, Jong Soo Woo, Young Dae Kim, Jong Seong Kim. Nonselective left internal mammary artery angiography during right transradial coronary angiography: a simple, rapid, and safe technique. Angiology 2001;52:773–9. https://doi.org/10.1177/000331970105201107
15. Cha KS, Kim MH. Feasibility and safety of concomitant left internal mammary arteriography at the setting of the right transradial coronary angiography. Catheter Cardiovasc Interv 2002;56:188–95. https://doi.org/10.1002/ccd.10164
16. Dorros G, Lewin RF. Angiography of the internal mammary artery via the contralateral brachial artery. Cathet Cardiovasc Diagn 1987;13:138–40. https://doi.org/10.1002/ccd.1810130213
17. Dato I, Porto I, Camaioni C, Crea F. Left anterior descending artery percutaneous coronary intervention from the right radial access via the left internal mammary artery: a case report. Cardiovasc Revascularization Med 2011;12:412–16. https://doi.org/10.1016/j.carrev.2011.03.005
18. Patel T, Shah S, Patel T. Cannulating LIMA graft using right transradial approach: two simple and innovative techniques. Catheter Cardiovasc Interv 2012;80:316–20. https://doi.org/10.1002/ccd.24321
19. García-Touchard A, Fernández-Díaz J, Francisco D, Goicolea-Ruigomez J. Intraarterial guidewire external compression: a simple technique for successful LIMA angiography through the right radial approach. J Interv Cardiol 2008;21:175–7. https://doi.org/10.1111/j.1540-8183.2007.00300.x
20. Azarbal F, Yeo KK, Shunk K. TCT-331 clinical characteristics and outcomes in patients undergoing PCI to LIMA grafts: a study from the ACC NCDR CathPCI registry. J Am Coll Cardiol 2016;68:B137. https://doi.org/10.1016/j.jacc.2016.09.462
21. Sandoval Y, Burke MN, Lobo AS et al. Contemporary arterial access in the cardiac catheterization laboratory. JACC Cardiovasc Interv 2017;10:2233–41. https://doi.org/10.1016/j.jcin.2017.08.058
