Blackout is a common, alarming symptom occurring across patients of all ages, and can create enormous psychological and social distress. In this review, we describe a new clinical approach that improves healthcare delivery to patients suffering blackouts.
Introduction
Case history 1
PL is a 19-year-old female who presented with two episodes of blackout accompanied with convulsions. She was diagnosed with epilepsy and prescribed carbamazepine. Episodes continued, however, and one year later she was further investigated by tilt-testing and discovered to have cardioinhibitory vasovagal syncope. A dual-chamber rate-drop-response pacemaker was implanted and no further episodes occurred during five years of follow-up. Anticonvulsant medication was stopped without ill effect.
Case history 2
CM is a 72-year-old male admitted for pain control following an unwitnessed fall, which although initially believed to be a mechanical fall, was later revealed to be unexplained. He denied any prodromal symptoms or loss of consciousness and had suffered five previous falls in the last 12 months, developing symptoms of depression as a result. Previous investigations (Holter monitoring, echocardiogram and Doppler studies) were unremarkable. Tilt-testing, however, confirmed a diagnosis of vasodepressor vasovagal syncope. After being given preventive advice, he remained asymptomatic after two years of follow-up, regained confidence and no longer suffers from depressive symptoms.
Diagnosis
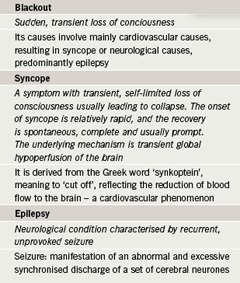
Blackout (a sudden, transient loss of consciousness, table 1) is a frightening symptom for many patients. The current convention of having entirely separated cardiological and neurological pathways is hampering speedy, accurate and cost-effective diagnosis. As a consequence, a significant proportion of sufferers are either not assessed or are misdiagnosed (for example, with epilepsy) with potentially disastrous effects on their well-being.
In this review, we highlight the challenges in managing patients presenting with transient loss of consciousness, the implications of misdiagnosis, and present the concept of rapid access blackout clinics – a novel clinical pathway that can streamline and improve the healthcare delivery to patients suffering blackouts.
The scale of the problem
Epilepsy
Even though epilepsy (the principal neurological cause of blackout) is one of the most common serious neurological conditions in the UK with a prevalence between 0.7–1%,1 only one to two new cases occur per year within the average list size of a UK general practitioner.2 The condition, nevertheless, can confer significant morbidity and mortality for patients. For instance, important medical complications include status epilepticus, injuries from falls, aspiration and sudden unexpected death, which is estimated to account for 500 deaths per year in the UK.3 In addition, patients are faced with a high social burden including mistreatment, social stigma, educational difficulties and driving and employment restrictions.
Syncope
Syncope, in contrast to epilepsy, is far more common: it affects half of the UK population at some point in their lives, and is responsible for 3% of accident and emergency admissions and 1% of all admissions to hospital.4 It shows a similar bi-modal incidence to epilepsy5 as it appears to be increased in two age clusters – the young and the elderly.6 In the young, there is a peak around 15 years of age, with females having more than twice the incidence of males. In the elderly, it affects 35% of adults over 65 years and 45% over 80 years.7 Syncope, therefore, just like epilepsy, imposes an important medical, social and economic burden on the general population.
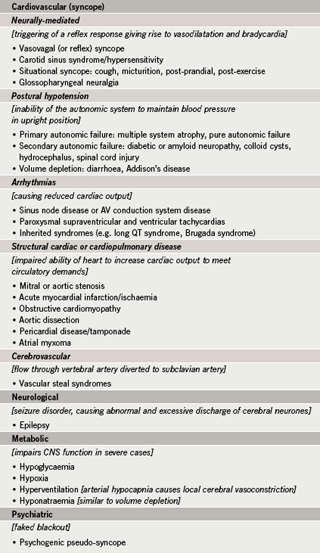
Among the causes (table 2), the most common is neurally-mediated syncope, which refers to a group of cardiovascular disturbances that are characterised by the triggering of a reflex response. Despite extensive research, the afferent arc remains to be elucidated but the efferent arc involves a reduction in sympathetic outflow to the vasculature and the heart and activation of vagal efferents, causing vasodilatation and a variable degree of bradycardia, which causes transient global cerebral hypoperfusion leading to transient loss of consciousness.8
The most common form of neurally-mediated syncope is ‘vasovagal syncope’, which causes 40% of syncopal events.9 Precipitating factors include emotional distress, fear, or prolonged standing, and there are usually early symptoms and signs such as pallor, weakness or nausea. On regaining consciousness, the patient may complain of persistent weakness.8 Indeed, in common with other causes of syncope, although there is rapid and complete recovery from the transient loss of consciousness, patients may continue to experience unpleasant symptoms such as exhaustion, dizziness and dyspnoea for hours or days after the syncopal episode.10
Syncope as a disability
Recurrent syncopal events, which affect one in three patients, can dramatically impair all aspects of physical and social functioning, affecting activities of daily living, driving, employment, and impacting on interpersonal relationships.10 Affected patients are also predisposed to sustain injury from collapse11 and the functional impairment has been reported to be similar to patients suffering from rheumatoid arthritis or chronic back pain. Psychologically, there is a high prevalence of chronic anxiety and depression.12
Prognosis
Decisive management of patients can reverse the physical and psychosocial morbidity associated with syncope. Nevertheless, patients affected by recurrent episodes of vasovagal syncope have a favourable prognosis, as they are at no increased risk of cardiovascular mortality.13 In contrast, patients with an underlying cardiac cause, which includes those with structural heart disease and arrhythmias, are at an increased risk of non-fatal and fatal cardiovascular events,13 especially sudden cardiac death. Indeed, syncope is a key early symptom in children and young adults who have congenital life-threatening arrhythmias such as long QT syndrome and Brugada syndrome. Such patients need to be accurately diagnosed as life-saving treatment can be offered. However, evidence reveals that diagnostic difficulties hinder the effective management of patients who present with transient loss of consciousness.
Diagnostic challenges
Half of all patients presenting with syncope do not attain a diagnosis while in hospital despite investigation.14 Even for the half receiving a diagnosis, that diagnosis can often be wrong, with blackouts wrongly attributed to epilepsy or a mechanical fall (especially in the elderly).
A presumptive diagnosis of epilepsy is often made initially in a patient presenting with syncope, and may be discovered to be incorrect later.15 This bias may be because a number of cardiovascular causes of blackouts, such as vasovagal syncope or primary cardiac arrhythmia, can masquerade as epilepsy. It is important to remember that prolonged syncope can result in secondary seizures. Even in the absence of secondary seizures, there can be urinary incontinence.16 Such similar features arise because transient global cerebral hypoperfusion in syncope causes cerebral anoxia that may result in myoclonic jerks and sometimes a full reflex anoxic seizure. Indeed, Lempert et al.17 reported that myoclonic activity, predominantly multifocal jerking in proximal and distal muscles, occurred in 90% of healthy subjects in whom syncope was induced using a combination of hyperventilation, orthostasis and the Valsalva manoeuvre. The underlying mechanism of epilepsy is different, with seizures resulting from neuronal hyper-excitability rather than transient hypoperfusion. Regardless of underlying mechanisms, the manner of presentation understandably causes a diagnostic hindrance, although there is a propensity towards overdiagnosing epilepsy.
Syncope masquerading as epilepsy
Around 20–30% of adults and 40% of children18 who are diagnosed with epilepsy do not actually have the condition. In children, syncopal events are commonly due to ‘neurally-mediated syncope,’ also called ‘reflex asystolic seizures,’ which highlight a cardiorespiratory disturbance, not a neurological disturbance like epilepsy. Diagnosis is particularly difficult in children because a clear first-person history is often unavailable in the very young, and clinical features are easily mistaken to be due to epilepsy.
This is a critical public health issue, therefore, due to the number of patients affected, approximately 100,000 in the UK alone, and due to the consequences of misdiagnosis for patients, such as:
- denial of potentially life-saving treatment, such as a pacemaker or defibrillator
- commencement on potentially harmful anticonvulsant therapy
- symptom recurrence may lead to more expensive drugs being employed (with high cost to both the patient and the hospital budget)
- symptom recurrence may also lead to diagnostic ambiguity, further investigative costs and further delay for correct treatment to be initiated
- impingement of high social burden in education, employment, driving and life insurance.
Substantial financial savings could be made from correct management of patients, as reported by the All Parliamentary Group on Epilepsy in 2007:19 the annual cost of epilepsy misdiagnosis in England is estimated at around £189 million a year, which takes into account unnecessary treatment costs, economic costs of lost work and payments of the Disability Living Allowance, which itself totals £55 million a year.
Syncope masquerading as mechanical fall
Syncope and mechanical falls are the most common reasons for elderly patients to present at an accident and emergency department.20 Misdiagnosis of mechanical falls is most problematic in this group of patients and represents another challenge in obtaining a correct diagnosis: 30% of patients aged ≥ 65 may not admit to loss of consciousness due to retrograde amnesia, but the resultant fall will be reported.21 This is further hampered by the lack of an eyewitness account in 50% of cases.22 As a result, doctors may be swayed to diagnose a fall and patients will not be treated for the actual precipitating cause, such as an arrhythmia. This increases the likelihood of more falls with an allied increase in morbidity and mortality, and also contributes to the rising costs of managing falls, estimated to cost the NHS over £1 billion each year.
The rapid access blackout clinic
Historic assessment and management pathways appear to be failing patients presenting with transient loss of consciousness. One study8 reported that the length of stay in hospital after acute admission for those over 65 years was 5–17 days, highlighting the implementation of variable management plans. This has been contributed to by disparity among hospitals in the investigative approach to patients and highlights the difficulty in acquiring the correct diagnosis.14
Effective handling of patients with blackouts comes from early clinical evaluation by specialist staff trained to do this rapidly and efficiently, and who have access to all necessary facilities without requiring elaborate inter-referrals, which create confusion and delay. Within this model of care is the opportunity to apply management strategies to patients presenting with blackouts that deliver diagnostics decisions.
The Department of Health Heart Team Expert Reference Group for the National Service Framework for Arrhythmias and Sudden Cardiac Death23 formulated algorithms for the management of patients presenting with blackout at four points of call: ambulance service, accident and emergency department, general practitioner, and secondary referral. The rapid access blackout clinic is the secondary referral care pathway, a single out-patient clinic accessible within two weeks of referral that eliminates referral delays arising from uncertainty about the mechanism of the presenting symptom. In some localities there are rapid access seizure clinics and syncope clinics, which make it easy for referrers to get patients through to specialist review. However, even in these regions, referrers may hesitate, especially in the many patients where they cannot be immediately confident of which group of aetiologies to suspect more strongly. Access to a blackout clinic eliminates this final block to specialist assessment of the patient.
By making diagnostic clarity its paramount interest, the aim of the clinic is simple: to complete a global assessment of patients (referred by accident and emergency or their general practitioner) that will secure a definitive diagnosis efficiently and cost-effectively.
Clinical expertise
A dedicated, specialist nursing team with blackout skills will provide the first stage of the diagnostic service. The nursing team may include separate neurologically and cardiologically trained specialist nursing sisters or, as these skills become more widespread, individual specialist nurses who possess both sets of skills. Other members of the multi-disciplinary team are brought in after initial evaluation including specialist neurology and cardiology doctors, geriatricians, and (where available) clinical autonomic scientists.
Initial assessment
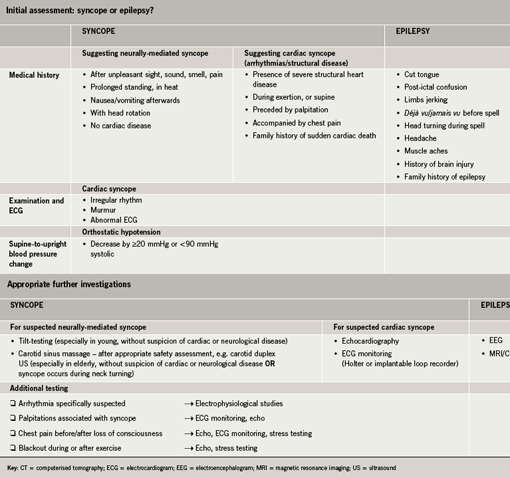
As highlighted in the Imperial College Healthcare NHS Trust protocol for the rapid access blackout clinic (figure 1), modelled on the European Society of Cardiology guidelines,24 the initial assessment is primarily focused on deciding whether the patient is likely to have syncope or epilepsy. It involves four key components: medical history with the aid of a computer-based extended questionnaire, a physical examination, electrocardiogram (ECG) and supine and upright blood pressure, and thus ensures that the various causes of syncope are all taken into account; suspicion of epilepsy is principally raised through an accurate medical history.
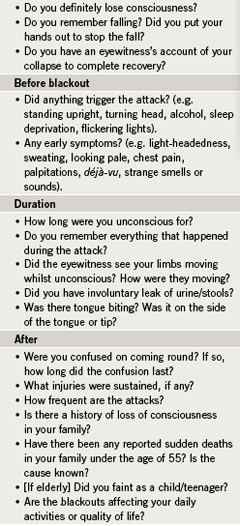
The questionnaire acts as a pre-assessment form, establishing the patient’s background medical history, which includes past cardiac and neurological history. An eyewitness account is a very valuable way to ascertain an accurate history, and patients will be asked to answer the questionnaire with the help of any eyewitnesses before attending the clinic. The questionnaire also contains focused questions regarding the transient loss of consciousness: the circumstances and experiences before, during and after the episode (table 3). To help guide diagnosis, the most important clinical features differentiating between epilepsy and various causes of syncope are outlined in the protocol.25 This initial approach, which may result in a diagnosis or a suspected diagnosis, can thus discover quickly if and where further investigative priorities need to be placed (table 4), and will help avoid unnecessary hospital admissions, which alone are responsible for 74% of the cost of investigating patients.7
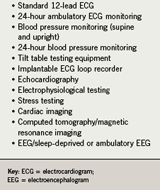
Appropriate further investigation
With regards to syncope, further investigations will be most necessary in determining if the mechanism is neurally-mediated or of a cardiac origin. The most valuable tests at present for neurally-mediated syncope include the use of tilt-testing (figure 2) to diagnose and categorise vasovagal syncope and performing carotid sinus massage to diagnose carotid sinus hypersensitivity. For patients who are young, in whom there is no suspicion of cardiac or neurological disease, there is a strong likelihood that vasovagal syncope is the culprit for transient loss of consciousness, and so tilt-testing can be particularly helpful in securing a positive diagnosis.
A variety of protocols are employed for tilt-testing among clinical institutions, and many incorporate pharmacological provocation if the initial tilt-test is negative. Our centre uses the Westminster protocol.26

Carotid sinus hypersensitivity is a disease of the elderly and so older patients (over 50 years) are most likely to respond to carotid sinus massage, especially those without features suggesting the existence of cardiac or neurological disease or in those who have a typical history of syncope during neck turning. A standardised safe technique exists although there are contraindications, such as previous ventricular tachyarrhythmias or carotid bruit.27 Some centres use carotid duplex ultrasound, rather than clinical examination, to exclude carotid disease before carotid sinus massage.
Ultimately, the protocol places most stress on evaluating patients suspected of cardiac syncope as they have a poorer prognosis than patients with neurally-mediated syncope. For instance, an abnormal ECG creates a strong suspicion of an arrhythmic cause of syncope, especially important for some potentially life-threatening inherited arrhythmias in children. Further investigation of patients likely to have cardiac syncope may involve echocardiography (if structural heart disease is suspected) or the implantable loop recorder, which provides a new opportunity to diagnosing arrhythmias in patients in whom tilt-testing does not usefully reproduce the presenting symptom.28 Once implanted, the patient simply activates the device with a hand-held control after any subsequent episode of syncope and the device automatically retains the previous 40 minutes of ECG to memory, which almost always includes the period of syncope itself. The ‘Additional testing’ section under ‘syncope’ is a supplementary list of specific recommendations that are all directed at appropriately investigating the underlying cardiac cause of syncope, emphasising the need for a comprehensive investigative approach in this group of patients.
In contrast, further investigations for epilepsy are not essential for diagnosis but instead are used to classify the type of epilepsy, which is important when considering the best treatment approach. Investigations include the electroencephalogram (EEG) and magnetic resonance imaging (MRI). EEG may be useful in assessing the likelihood of further epileptic seizures after an isolated seizure as well as assisting syndromic classification. MRI is often useful for identifying aetiology, especially in localisation-related cases, such as in hippocampal sclerosis, focal cortical scars, malformations of cortical development, tumours, cavernomas and arteriovenous malformations.
Impact of STARS
The blackout charity, Syncope Trust And Reflex anoxic Seizures (STARS – www.stars.org.uk), is the leading resource for support and information for both patients and medical professionals on syncope and reflex anoxic seizures. The STARS Medical Advisory Committee developed a blackouts checklist, a patient-directed checklist of important information regarding blackouts that aims to educate and empower patients. Almost 10,000 downloads of this document were made in less than three months. Components of this checklist have also been used to structure the questionnaire that forms part of the initial assessment of patients.
Conclusion
The effective management of patients presenting with transient loss of consciousness is an important clinical challenge. Pioneered at the Manchester Royal Infirmary, and developed further into a multi-disciplinary cardiology–neurology collaboration at Imperial College Healthcare NHS Trust (part of the UK’s first Academic Health Science Centre), the rapid access blackout clinic creates a single entry point through which every patient can undergo a cohesive and thorough assessment. It establishes an easy referral pathway (for general practitioners and accident and emergency departments), and attempts to overcome common diagnostic difficulties, which otherwise lead to high rates of clinical uncertainty, misdiagnosis and unnecessary financial costs. Widespread availability of these clinics, now a national priority in the UK as part of the National Service Framework, will provide improved healthcare for all patients affected by blackouts.
Acknowledgements
The authors are grateful for support from Sister Andrea Meyer, Sister Kicki Franzen-McManus and from the NIHR Biomedical Research Centre funding scheme.
Conflict of interest
None declared.
Editors’ note
An editorial on the rapid access blackout clinic by Byrne and O’Shea can be found on pages 9–10 of this issue.
Key messages
- The assessment of transient loss of consciousness is a common clinical problem
- A substantial proportion of patients presenting with syncope are either not diagnosed or are misdiagnosed, for instance with epilepsy or, especially in the elderly, a mechanical fall
- The rapid access blackout clinic attempts to overcome important diagnostic challenges by providing an integrated and complete evaluation of patients that aims to secure a definitive diagnosis efficiently and cost-effectively
References
- Stokes T, Shaw EJ, Juarez-Garcia A et al. Clinical guidelines and evidence review for the epilepsies: diagnosis and management in adults and children in primary and secondary care. London: Royal College of General Practitioners, 2004.
- Macdonald BK, Cockerell OC, Sander JW, Shorvon SD. The incidence and lifetime prevalence of neurological disorders in a prospective community-based study in the UK. Brain 2004;123(Pt 4):665–76.
- Petkar S, Cooper P, Fitzpatrick AP. How to avoid a misdiagnosis in patients presenting with transient loss of consciousness. Postgrad Med J 2006;82:630–41.
- Ammirati F, Colivicchi F, Minardi G et al. The management of syncope in the hospital: the OESIL Study (Osservatorio Epidemiologico della Sincope nel Lazio). G Ital Cardiol 1999;5:533–9.
- Sander JW, Hart YM, Johnson AL, Shorvon SD. National general practice study of epilepsy: newly diagnosed epileptic seizures in general population. Lancet 1990;336:1267–71.
- Wieling W, Ganzeboom KS, Krediet CTP et al. Initiele diagnostische strategien bij wegrakingen: het belang van de anamnese (Initial diagnostic strategy in the case of transient losses of consciousness: the importance of the medical history). Ned Tijdschr Geneesk 2003;147:849–54.
- Kenny RA, O’Shea D, Walker HF. Impact of a dedicated syncope and falls facility for older adults on emergency beds. Age & Ageing 2002;31:272–5.
- Fenton AM, Hammill C, Rea RF, Low PA, Shen WK. Vasovagal syncope. Ann Intern Med 2000;133:714–25.
- Kapoor WN. Evaluation and outcome of patients with syncope. Medicine (Baltimore) 1990;69:160–75.
- Shaffer C, Jackson L, Jarecki S. Characteristics, perceived stressors, and coping strategies of patients who experience neurally mediated syncope. Heart Lung 2001;30:244–9.
- Kapoor W, Petersen J, Wieand HS, Karpf M. Diagnostic and prognostic implications of recurrences in patients with syncope. Am J Med 1987;83:700–08.
- Kapoor WN, Foruanto M, Hanusa BH, Schulberg HC. Psychiatric illnesses in patients with syncope. Am J Med 1995;99:505–12.
- Soteriades ES, Evans JC, Larson MG et al. Incidence and prognosis of syncope. N Engl J Med 2002;347:878–85.
- Kapoor WN, Karpf M, Wieand S, Peterson JR, Levey GS. A prospective evaluation and follow-up of patients with syncope. N Engl J Med 1983;309:197–203.
- Zaidi A, Clough P, Cooper P, Scheepers B, Fitzpatrick A. Misdiagnosis of epilepsy: many seizure-like attacks have a cardiovascular cause. J Am Coll Cardiol 2000;36:181–4.
- Fitzpatrick AP, Cooper P. Diagnosis and management of patients with blackouts. Heart 2006;92:559–68.
- Lempert T, Bauer M, Schmidt D. Syncope: a videometric analysis of 56 episodes of transient cerebral hypoxia. Ann Neurol 1994;36:233–7.
- Uldall P, Alving J, Buchholt J, Hansen L, Kibak M. Evaluation of a tertiary referral epilepsy centre for children. Epilepsia, Proceedings of International League Against Epilepsy, 2001.
- Report by the All Parliamentary Group on Epilepsy 2007. The human and economic cost of epilepsy in England. Available at: http://www.epilepsy.org.uk/campaigns/lobbying/appg/index.html [accessed 1st August 2007].
- Kenny RA, Richardson DA, Steen N, Bexton RS, Shaw FE, Bond J. Carotid sinus syndrome is a modifiable risk factor for non-accidental falls in older adults. J Am Coll Cardiol 2001;38:1491–9.
- Benditt DG, Blanc JJ, Brignole M, Sutton B, eds. The evaluation and treatment of syncope. A handbook of clinical practice. New York: Blackwell, 2003.
- Shaw FE, Kenny RA. The overlap between syncope and falls in the elderly. Postgrad Med J 1997;73:635–9.
- Department of Health. The national service framework for coronary heart disease. Available at: http://www.dh.gov.uk/en/Publicationsandstatistics/Publications/publicationsPolicyAndGuidance/DH_4094275 [accessed 26th July 2007].
- European Society of Cardiology Task Force on Syncope. Guidelines on Management (Diagnosis and Treatment) of Syncope – Update 2004. Eur Heart J 2004;25:2054–72.
- Sheldon R, Rose S, Ritchie D et al. Historical criteria that distinguish syncope from seizures. J Am Coll Cardiol 2002;40:142–8.
- Fitzpatrick AP, Theodorakis G, Vardas P, Sutton R. Methodology of head-up tilt testing in patients with unexplained syncope. J Am Coll Cardiol 1991;17:125–30.
- Munro NC, McIntosh S, Lawson J, Morley CA, Sutton R, Kenny RA. Incidence of complications after carotid sinus massage in older patients with syncope. J Am Geriatr Soc 1994;42:1248–51.
- Farwell DJ, Freemantle N, Sulke AN. Use of implantable loop recorders in the diagnosis and management of syncope. Eur Heart J 2004;14:1547–63.
