A 52-year-old man presented to the emergency department with increasingly frequent anginal chest pain. He had had an anterior ST elevation myocardial infarction two years previously, for which he received thrombolysis. He was an ex-smoker, hypercholestrolaemic and had a family history of ischaemic heart disease. During stress electrocardiography, he developed chest pain at nine minutes of a standard Bruce protocol, but no significant ST changes.
A computed tomography (CT) coronary angiogram (CTA) was performed, as the patient was not keen on an invasive angiogram, and demonstrated sub-endocardial hypoattenuation at rest in the anterior wall, apex and apical inferior walls (figure 1B). It was not clear if there was any reversible ischaemia so a myocardial perfusion scintigraphy (SPECT) was performed, and demonstrated a partial thickness infarction involving the anterior wall, apex and apical inferior wall (figure 1A). A research cardiac magnetic resonance (CMR) scan demonstrated late Gadolinium enhancement in the same territories as the other two studies (figure 1C).
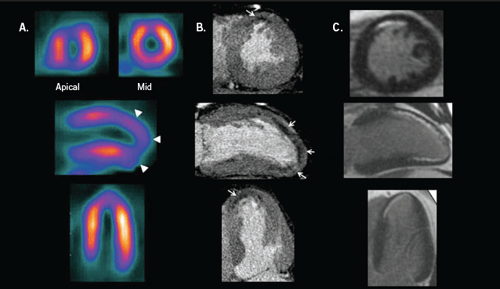
Recent advances in non-invasive imaging have resulted in the ability to assess myocardial infarction with multiple modalities. Each technique relies on a different methodology for the assessment of irreversible myocardial injury. For SPECT, a comparison of images obtained at rest and during hyperaemic stress demonstrates the absence or delayed uptake of a radioisotope, while CMR detects infarction by the delayed clearance of a paramagnetic contrast agent. CTA may detect infarction by either reduced first-pass perfusion or via delayed clearance of iodinated contrast. Given these inherent differences, the relative strengths and weakness of these techniques for the detection of myocardial injury are likely to be clinically important.
Conflict of interest
None declared.
