We surveyed 510 patients to measure levels of patient satisfaction with our cardiac rehabilitation service and to compare health-related outcomes between patients who did, and did not, attend cardiac rehabilitation. Two hundred and sixty-five patients responded (52.4%). Our results showed that cardiac rehabilitation was associated with improved health behaviours, such as diet and exercise, and was popular with patients. The majority of non-attenders would have attended cardiac rehabilitation if certain features had been available. Following the survey, various improvements were made to the rehabilitation service, including a re-design of the patient literature and a designated lead consultant.
Introduction
Cardiac rehabilitation aims to address all modifiable behavioural risk factors that are susceptible to intervention, including smoking, exercise, diet and weight.1,2 Since less than half of eligible patients attended the out-patient-based cardiac rehabilitation programme at St George’s Hospital, we wanted to establish whether our service was beneficial and popular with patients, and what features might persuade others to participate. This evidence would enable us to improve our service and increase attendance, thereby reducing the risk of further cardiac events, with consequent benefits to patients, their families and healthcare providers. We surveyed patients who were offered cardiac rehabilitation after their admission to St George’s Hospital in 2006, in accordance with the National Service Framework (NSF) for Coronary Heart Disease (CHD).2
Methods
Questionnaires were posted to a cohort of 510 patients. Patients who attended cardiac rehabilitation (attenders) received a set of questions about their satisfaction levels with the service provided. Patients who did not attend (non-attenders) were asked what features would have made them more likely to attend. Four- and five-point Likert scales3 were used to enable respondents to specify their level of agreement with the relevant question. This produced ordinal data, which were reduced to a nominal level by summing the responses. Both sets of patients were asked the same questions about their health-related behaviour and cardiac risk factors.
The data were entered and analysed in Microsoft Excel® and Clinstat®. Where specific questions were not answered, these cases were excluded from the percentages. Statistical analysis was performed using the independent samples t-test or Chi-squared test. A probability value of p<0.05 was considered significant.
Exclusions
- Non-local patients, as defined by postcode of residence.
- Deceased patients.
- Questionnaires returned blank.
Results
We received completed questionnaires from 265 patients (52.4%). Of these, 144 (54%) had attended cardiac rehabilitation sessions. The mean age of respondents was 67.4 years and about one-third were female (31%). Thirteen (11%) non-attenders were current smokers, compared with five (3.5%) attenders (p=0.017).
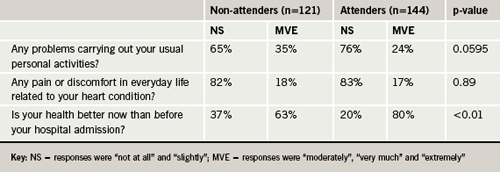
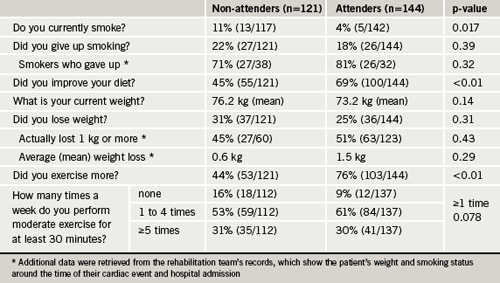
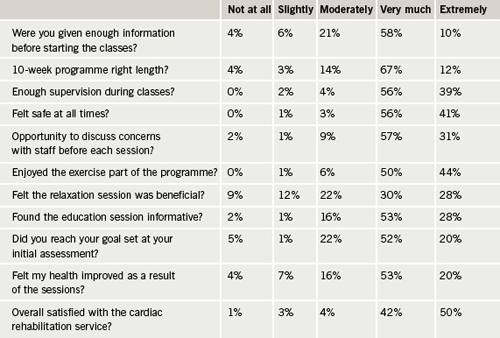
All patients in this sample were provided with advice and information about making healthy lifestyle changes after their cardiac event, but this was reinforced during cardiac rehabilitation. Table 1 shows that attenders were more likely to be non-smokers, to have improved their diet, to weigh less and to have exercised more. Attenders reported less problems experienced in carrying out their usual activities and better health now than before their hospital admission (table 2). Attenders reported high satisfaction levels with all aspects of the cardiac rehabilitation sessions (table 3); relaxation sessions were the least popular feature.
Discussion
These results clearly demonstrate the appeal and benefits of cardiac rehabilitation. Patients who attended were more likely to report healthy behaviour changes relating to smoking (p=0.017), diet (p<0.01), exercise (p<0.01) and perception of improved health since their hospital admission (p<0.01). Our demographics were comparable with published studies.4,5
Exercise is an important component of cardiac rehabilitation programmes and the health-related benefits are well evidenced.6,7 Ninety-one per cent of attenders were performing moderate exercise at least once a week, compared with 84% of non-attenders (p=0.078). Less than one-third of patients in each group were meeting the government target of performing moderate intensity physical exercise for at least 30 minutes, five times a week or more.8 Although this result falls short of the NSF target of 50%, it compares favourably with nationally reported exercise levels in the 65–74 years age group: 21% of men and 16% of women.9 These statistics confirm that exercise levels generally decline with age, a phenomenon compounded by reduced exercise tolerance following a cardiac event.10
The majority of patients, who responded to our survey, were very satisfied with all aspects of the cardiac rehabilitation service. Patient satisfaction is vital to ensure that patients comply with the interventions, complete the full programme and maintain healthy behaviour changes over the long term. Other studies have demonstrated the health-related benefits of using cardiac rehabilitation to educate, motivate and empower patients.11-13
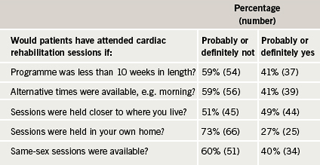
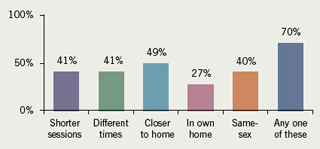
Our survey offered five different features to non-attenders, based on a review of the literature (table 4 and figure 1). Contrary to other published research,4,5 the least popular feature was holding rehabilitation sessions in the patient’s own home. The most popular feature – holding sessions closer to where they lived – was positively rated by 44 (49%) respondents. Other studies have reported that providing home-based and closer-to-home options contribute to improved attendance rates.4,14 However, preferences vary considerably between different patient groups,5,15,16 which demonstrates the difficulty of planning services to meet all needs, given the financial constraints in the National Health Service (NHS).
The survey has provided valuable information for improving and re-designing our rehabilitation service. Following the study, a lead consultant was designated for the rehabilitation team, which improved the patient literature and engagement process in order to increase attendance rates. We are now participating in the National Association for Cardiac Rehabilitation (NACR) database, which enables reporting against NSF standards.17 We have also become a pilot site for a new national tariff, based on Payment by Results. The feasibility of home visits will be considered, subject to available resources.
Acknowledgements
The cardiac rehabilitation team and clinical audit department at St George’s Hospital, Tooting.
Conflict of interest
None declared.
Editors’ note
Also see the editorial by Varghese and Flint on pages 211–12 of this issue.
Key messages
- Attendance at cardiac rehabilitation is associated with improvement in health-related behaviours and outcomes
- Patients reported high satisfaction levels with the cardiac rehabilitation service at St George’s Hospital
- Attendance at cardiac rehabilitation sessions could be increased if various features were available to patients, but the cost/benefit implications must be considered carefully
References
- Ogden J. Health psychology: a textbook. Buckingham: Open University Press, 1996.
- Department of Health. National Service Framework for Coronary Heart Disease. Chapter seven, cardiac rehabilitation. London: DoH, 2000. Available from: www.dh.gov.uk/en/Healthcare/NationalServiceFrameworks/Coronaryheartdisease/index.htm [Accessed 9 October 2008].
- Likert R. A technique for the measurement of attitudes. Arch Psychol 1932;140:1–55.
- Dalal HM, Evans PH. Achieving National Service Framework standards for cardiac rehabilitation and secondary prevention. BMJ 2003;326:481–4.
- Filip J, McGillen C, Mosca L. Patient preferences for cardiac rehabilitation and desired program elements. J Cardiopulm Rehabil 1999;19:339–43.
- Alexander JL, Wagner CL. How cardiac rehabilitation relates to quality of life. Rehabil Nurs 2006;31:155–7.
- Marchionni N, Fattirolli F, Fumagalli S et al. Improved exercise tolerance and quality of life with cardiac rehabilitation of older patients after myocardial infarction. Circulation 2003;107:2201–06.
- Department of Health. At least five a week; evidence on the impact of physical activity and its relationship to health. A report from the Chief Medical Officer. London: DoH, 2004. Available from: www.dh.gov.uk/en/Publicationsandstatistics/Publications/PublicationsPolicyAndGuidance/DH_4080994 [Accessed 9 October 2008].
- The Information Centre. Statistics on obesity, physical activity and diet: England, January 2008. Available from: www.ic.nhs.uk/statistics-and-data-collections/health-and-lifestyles/obesity/statistics-on-obesity-physical-activity-and-diet:-england-january-2008 [Accessed 9 October 2008].
- Myers J. Principles of exercise prescription for patients with chronic heart failure. Heart Fail Rev 2008;13:61–8.
- Carter B. Compliance and cardiac disease. Am J Nurs 1999;99:24.
- Schubmann RM, Vogel H, Placzek T, Faller H. Cardiac rehabilitation – expectations and appraisals of patients. Rehabilitation 2005;44:134–43.
- Simchen E, Naveh I, Zitser-Gurevich Y et al. Is participation in cardiac rehabilitation programs associated with better quality of life and return to work after coronary artery bypass operations? The Israeli CABG study. Isr Med Assoc J 2001;3:399–403.
- Grace SL, Evindar A, Kung T et al. Retrospective evaluation of automatic referral to cardiac rehabilitation (CR) closest to home. J Cardiopulm Rehabil 2003;23:387–9.
- Jones M, Jolly K, Raftery J et al. “DNA” may not mean “did not participate”: a qualitative study of reasons for non-adherence at home- and centre-based cardiac rehabilitation. Fam Pract 2007;24:343–57.
- Grace SL, McDonald L, Fishman D, Caruso V. Patient preferences for home-based cardiac rehabilitation versus hospital-based cardiac rehabilitation. J Cardiopulm Rehabil 2005;25:24–9.
- Lewin R, Thompson DR, Roebuck A. Development of the BACR/BHF minimum dataset for cardiac rehabilitation. Br J Cardiol 2004;11:300–01.
