Temporary transvenous pacing (TTVP) is a procedure that carries significant risk to the patient. We performed a retrospective analysis of TTVP in an outer London hospital between July 2003 and March 2009 to establish who performed the procedure and the outcomes.
Introduction
 Temporary transvenous pacing (TTVP) has been used to treat life-threatening bradycardic, and tachycardic emergencies for 50 years. We present a retrospective analysis of TTVP in an outer London hospital between July 2003 and March 2009.
Temporary transvenous pacing (TTVP) has been used to treat life-threatening bradycardic, and tachycardic emergencies for 50 years. We present a retrospective analysis of TTVP in an outer London hospital between July 2003 and March 2009.
Results
The results from 51 patients, undergoing a total of 58 procedures were identified. The mean age was 77 years. Almost two-thirds (62%) of all procedures were performed within working hours. The majority (74%) were performed within four hours of an identified indication. Of the patients delayed up to four hours, half were maintained on external pacing.
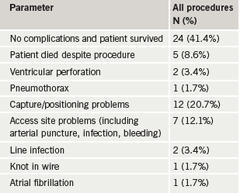
Less than half the patients (41.7%) had an uncomplicated procedure and survived the hospital admission (table 1). Five patients died despite the procedure and a further two patients experienced ventricular perforation, one dying from tamponade, despite undergoing pericardiocentesis. The second patient survived cardiothoracic surgery for significant tamponade. Fifty-three per cent of procedures were performed by trainees in cardiology. General medical (GIM) registrars performed six procedures (10%), always out of hours and generally unsupervised. Half of all procedures not performed by a consultant were supervised (26 of 51 procedures, 51%).
Long term, 27% of patients died during their hospital admission and 33% within six months.
Discussion
The general outcome of this patient cohort is very poor. A six-month mortality of 33% suggests these patients require intensive therapy both before and after TTVP insertion.
A high proportion (three of six, 50%) of TTVP inserted after hours by GIM registrars resulted in death. All occurred without consultant supervision. This low total procedure volume (approximately 10 per year) raises questions regarding the training and maintenance of skills for trainees in general medicine.1-3
If GIM registrars are to continue pacing acutely unwell patients then solutions need to be identified. Instruction could involve mannequins or simulators, and should form part of the core medical training. Flotation pacing devices are often easier to place and are less rigid, reducing the risk of cardiac perforation. The assistance of anaesthetists and/or dedicated ultrasound equipment in line placement may also reduce complications. The option of transfer to a 24/7 primary angioplasty centre; on-call rotas with cardiologists in neighbouring hospitals or collaboration with on-call senior-grade anaesthetists are further options. Transcutaneous pacing should always be available and provides an extended time window to summon an experienced operator.
Conclusion
TTVP is a procedure that carries significant risk to the patient, particularly out of hours by operators with ever-decreasing exposure to training. Hospitals need to establish local mechanisms to reduce this risk.
Conflict of interest
None declared.
Editors’ note
See also Editorial by Artis et al. on pages 11–12 and clinical article by Yassin et al. on pages 34–5.
Key messages
- Temporary transvenous pacing is a procedure that carries significant risk to the patient
- Analysis of procedures performed at an outer London hospital reveals that a third of patients die within six months
- Low total procedure volume raises questions regarding the training and maintenance of skills for trainees
- Hospitals need to establish local mechanisms to reduce risk
References
- Davis GK, Roberts DH. Experience and training in temporary transvenous pacing. J R Coll Physicians Lond 1996;30:424–4.
- Murphy JJ, Frain JP, Stephenson CJ. Training and supervision of temporary transvenous pacemaker insertion. Br J Clin Pract 1995;49:126–8.
- Sankaranarayanan R, Msairi A, Davis G. Ten years on: has competence and training in temporary transvenous cardiac pacing improved? Br J Hosp Med 2007;68:384–7.
