Plasma natriuretic peptide (NP) testing is not widely used in heart failure clinical practice in the UK or Ireland, despite a large evidence base. This article reports the views of a consensus group that was set up to develop guidance on the place of NP testing for clinicians in primary and secondary care.
 There is firm evidence for NP testing as part of the heart failure diagnostic pathway. Measuring NPs is also a useful prognostic tool and can help with discharge planning, and there is emerging evidence for use in treatment monitoring particularly in younger patients. For the future, NP measurement might also prove to be useful for screening high-risk patients for asymptomatic left ventricular systolic dysfunction.
There is firm evidence for NP testing as part of the heart failure diagnostic pathway. Measuring NPs is also a useful prognostic tool and can help with discharge planning, and there is emerging evidence for use in treatment monitoring particularly in younger patients. For the future, NP measurement might also prove to be useful for screening high-risk patients for asymptomatic left ventricular systolic dysfunction.
Introduction
The prognosis for patients with heart failure is considerably better than it was 10 years ago, but certain aspects of care need to be improved. A Healthcare Commission audit in 2007 reported that the delivery of heart failure diagnostic services is poor or only average in 50% of the country (England, Wales and Northern Ireland).1 Diagnosis is difficult because symptoms are non-specific and physical signs are often not obvious, but early and accurate diagnosis is important so that patients can start appropriate life-saving treatment.
Rates of hospitalisation for decompensated heart failure remain high, and there is also a problem of limited access to heart failure specialists: only 20% of patients admitted to hospital with heart failure have any specialist follow-up,1 highlighting the need to target specialist resources to high-risk patients.
Plasma B-type natriuretic peptides (BNP or NT-proBNP) are raised in patients with heart failure, with concentrations rising in line with the severity of symptoms (New York Heart Association [NYHA] class). There is a large and increasing evidence base on the value of natriuretic peptides (NPs) in clinical practice, particularly for helping with diagnosis, but use is still low. In 2007, only around 40% of acute trusts and primary care trusts (PCTs) in England offered NP testing for diagnosis,1 despite guideline recommendations for use (Panel).
This article reports the recommendations of a consensus group that was set up to develop clinical guidance on the current place of NP testing in the UK and Ireland. Four main areas of use were considered.
1. NP testing in diagnosing heart failure
The priority for NP testing in the National Health Service (NHS) should be as part of the process of heart failure diagnosis.
National and international heart failure guidelines recommend NP testing in the diagnostic pathway and a recent Health Technology Assessment (HTA) in England confirmed from individual patient data meta-analysis that measuring NPs is the single most useful test to add to the diagnostic process in primary care.2 This confirms what was recommended by Quality Improvement Scotland in 2007.3
NP testing is primarily used as a ‘rule-out’ test in patients with breathlessness and suspected heart failure. A raised plasma NP level does not diagnose heart failure, as there can be other reasons for the level to be raised, such as atrial fibrillation, ischaemic heart disease and renal dysfunction. But the test has a high negative predictive value: a ‘normal’ level means heart failure is unlikely and other causes for symptoms should be determined.
Since it is difficult to provide timely echocardiography for all patients with suspected heart failure in primary care, NP testing can be used to select patients who need priority referral for echocardiography, i.e. raised BNP or NTproBNP can be used as a ‘ticket for echo’.
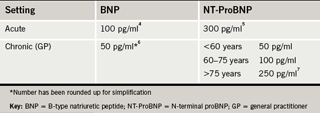
The decision cut-points recommended by the consensus group for use in acute and chronic healthcare settings are shown in table 1.4-7 While the manufacturers cite a single cut-point for both settings, the group felt that having a lower value for primary care would increase GPs’ confidence in the test as there will be minimal risk of false-negative results. Referral is always an option if heart failure is still suspected despite a negative NP test – no one test can be considered definitive, although NP testing is probably the single most useful test in the diagnostic work-up of patients with new symptoms.
NP testing is more effective than electrocardiography (ECG) as a ‘rule-out’ test for heart failure;8 also, it can be difficult for non-specialists to interpret ECGs. An ECG can provide valuable information about the cause of a patient’s heart failure (signs of previous myocardial infarction, arrhythmia, or left ventricular hypertrophy) but it does not need to be carried out at this early stage of the diagnostic work-up, if NP testing is available. In the elderly, the ECG is most unlikely to be completely normal in any case.
Using NP to select patients for echocardiography is a sensible use of health service resources. It will give overstretched echocardiography services more time to concentrate on patients with likely cardiac abnormalities. NP testing has been shown to be cost-effective in most circumstances for diagnosis both in primary care,2,9,10 and in patients presenting to an emergency room with acute dyspnoea.11
Using NP testing as a ‘rule out’ test will mean fewer inappropriate referrals. This is important as PCTs are increasingly scrutinising referrals to secondary care.
The evidence clearly points to the need for increased availability and uptake of NP testing in heart failure diagnosis, and such access is recommended by recent formal HTAs in both Scotland and England. The latter HTA recommended that the National Institute for Health and Clinical Excellence (NICE) guidelines be revised to take this evidence into account.
Recommendation 1: NP testing is an essential part of the diagnostic pathway for heart failure and is cost-effective. Use is recommended in all patients in whom heart failure is suspected.
2. Risk stratification and prognostication
NP testing can also be useful for risk stratification and prognostication in patients with heart failure.
Many studies have confirmed a strong, independent association of NP level with prognosis in chronic heart failure. There are also data showing that prognosis is associated with NP level in acute decompensation and in patients presenting with dyspnoea to the emergency room (ER).
The US Acute Decompensated Heart Failure National Registry (ADHERE), with data on around 50,000 patients with acute decompensated heart failure, shows a strong relationship between admission BNP level and in-hospital mortality, whatever the ejection fraction.12 Admission NP in the ER is also powerfully associated with mortality and cardiovascular hospitalisations at 90 days.13
Admission NP level is therefore important, but the discharge level is more useful for longer-term prognostication. Discharge NP level has been shown to predict outcome (hospital re-admission or death) for at least six months after an admission for decompensated heart failure.14,15
Furthermore, it has been suggested that the change in NP level during hospitalisation is the strongest predictor of adverse outcome, with increasing levels during admission being associated with poor prognosis and decreasing levels with better prognosis.16 In one study, increase of ≥30% in NT-proBNP during admission was a strong independent predictor of a very high risk of death or hospital re-admission within six months.14
Similarly, a retrospective evaluation of patients with acute heart failure showed that among patients treated intensively to try to reach BNP level of <250 pg/ml, those who had achieved this level on discharge had a lower rate of death or heart failure re-admissions at six months than patients who were clinically stable but had a discharge BNP of >250 pg/ml.17
The evidence, therefore, strongly suggests that measuring NP on discharge (and, ideally, on both admission and discharge to assess change during admission) can identify high-risk patients who might need intensification of therapy or closer monitoring. It can also help with discharge planning, as these patients are likely to benefit most from referral to the specialist community heart failure service and early specialist hospital review.
NP testing might also find a use for risk stratification in other areas. It is not formally used at present to select patients for cardiac transplantation, but NP levels have been shown to be better than the Heart Failure Survival Score in predicting death in advanced heart failure.18 The NP level can also identify increased risk of sudden death,19 and in specialist clinics, serial NP measurement might, therefore, help with identification of candidates for device therapy, although the evidence base for this approach is not definitive.
A high plasma NP concentration, despite optimum drug treatment, is associated with a poor prognosis. A level that does not fall despite attempts to improve management might, therefore, also help with decisions on a patient’s need for end-of-life care.
Recommendation 2: Admission and discharge NP measurement is useful for hospitalised heart failure patients. It can help to identify high-risk patients and help with discharge planning and targeting of resources. This, in turn, should help to reduce the rate of hospital re-admission.
3. Monitoring heart failure therapy
Trial data have become available over the past few years on the use of serial NP measurements to help with titration of therapy in patients with chronic heart failure. These trials have compared outcome in patients in whom therapy was titrated to an NP target (NP-guided therapy) with those receiving standard symptom-guided therapy.
Patients on NP-guided treatment have been shown to receive more intensive drug therapy. Some trials have indicated that this is associated with improved outcomes, but there does appear to be an age effect, with the suggestion that the benefit is greatest in those aged below 75 years.
For example, in the Trial of Intensified versus standard Medical therapy in Elderly patients with Congestive Heart Failure (Time-CHF),20 NT-proBNP-guided management had no significant effect in the overall trial population on the primary end point of 18-month survival free of all-cause hospitalisations compared with symptom-guided therapy, although survival free of heart failure hospitalisations (a secondary end point) was reduced. When analysed by age, NP-guided treatment improved clinical outcomes in patients aged <75 but not in those >75.
Similarly, the Battlescarred trial (which has been presented but is not yet published) is reported to have shown positive effects of NT-proBNP-guided therapy only in patients aged <75.
A recent meta-analysis of six randomised controlled trials – including TIME-CHF and Battlescarred – found that NP-guided therapy was associated with a significant reduction in all-cause mortality compared with usual care (hazard ratio 0.69),21 but the authors cautioned that their findings may be less applicable to elderly patients.
The case for NP monitoring is, thus, promising but not proven. The position may become clearer with larger trials. The current data suggest that patients on NP-guided treatment tend to receive better heart failure drug therapy. But there is also a signal that in elderly patients the risks might outweigh the benefits if therapy is intensified without considering patients’ co-morbidities. It is also important to note that most studies were from heart failure centres rather than ‘real world’ practice.
It is not yet clear how frequently NP levels should be measured (in several of the trials measurements were made every three months), and whether it is better to treat to a target NP or to reduce NP level by a specific percentage.
Biological variability also has to be considered when using NPs to titrate drug doses in chronic heart failure. There is marked intra-individual variability in NP levels in stable heart failure patients and it has been suggested that large changes in serial NP concentrations (perhaps 50–80% reduction) are needed for the change to be clinically relevant.22,23
Recommendation 3: The evidence supports the use of serial monitoring of NP levels to titrate therapy in specialist centres looking after younger heart failure patients in whom heart failure is the predominant pathology. Monitoring might encourage clinicians to intensify treatment in these patients. But such monitoring cannot at present be recommended for general medical out-patients or for primary care. For these patients, clinicians should continue to titrate therapy on the basis of target doses of neurohormonal antagonists, such as angiotensin-converting enzyme (ACE) inhibitors or beta blockers, as recommended in national and international heart failure guidelines.
4. Screening for left ventricular systolic dysfunction
Plasma concentrations of NPs are raised in those with asymptomatic left ventricular systolic dysfunction (LVSD), raising the possibility that NP testing could be used to screen for asymptomatic LVSD, particularly in high-risk populations, such as older patients with hypertension, ischaemic heart disease or diabetes.24
The idea is that with early identification of LVSD, it may be possible to slow or prevent progression to heart failure by initiating treatment, or ensuring that current management is optimised, for example in patients who are already taking ACE inhibitors for hypertension and are now identified as having high-risk cardiovascular disease.
Screening might also pick up other cardiovascular disease, including asymptomatic left ventricular (LV) diastolic dysfunction, and this could highlight the need for good cardiovascular risk factor control.
Screening of high-risk subjects has been shown to be more cost-effective than general population screening and to miss few cases of LVSD.10
However, NPs have not as yet been adopted in the UK as a screening tool. There is no randomised controlled trial to show that a screening strategy will change cardiovascular outcomes. There is also uncertainty over the optimum interval for repeated screening and the NP cut-point, given that lack of specificity means that the positive predictive value will be considerably lower in these groups.
There are currently no data to support NP testing for general (as opposed to high-risk) population screening.
Recommendation 4: NP testing might be considered for screening high-risk groups for LVSD but there are not yet enough data on the benefits of screening for this to be a priority for health service resources.
Practical aspects of NP testing
Are sex-related cut-offs needed?
The data suggest that different cut-offs are not needed for men and women for use of NP testing in diagnosis of heart failure.
To what extent is the NP level affected by current treatment?
Although some cardiovascular drugs in particular diuretics and ACE inhibitors, can reduce the NP level, and beta blockers can increase the NP level in the short term, in practice this does not appear to have any significant effect when testing is carried out for diagnostic purposes.
However, clinical judgement should be applied, and if GPs suspect heart failure despite a negative NP test, the patient should be referred for further assessment.
What effect does body mass index (BMI) have on NP levels?
NP tests can be affected by BMI. The reason for this is unknown but levels may be decreased in overweight and obese individuals, in both acute25 and chronic26 heart failure. This should be taken into account when interpreting test results, but is unlikely to influence diagnostic testing other than in severe obesity.
Should we use BNP or NT-proBNP tests?
Either test can be used perfectly well. For in-patient use, there is no difference between the two tests. The improved stability of NT-proBNP might be a factor in its favour for primary care if sample transportation time is high, as BNP needs to be measured within four hours of sampling or the sample separated and plasma frozen.
It makes sense to stick to one test within a geographical area to avoid confusion of healthcare staff – and patients – with different values.
Both tests are affected to some extent by renal dysfunction, which tends to raise NP levels.
Should we use point-of-care (POC) or laboratory-based tests?
NP testing can be carried out in the central laboratory or using a POC test. Either method is suitable. With the POC test, it is important for users to take part in an external quality assurance scheme and to use the test in accordance with the manufacturer’s recommendations. It makes sense to measure the same NP as the local laboratory. Use of POC tests is likely to be cost-effective for GPs, unless a blood sample also needs to be sent to the laboratory for other tests.
‘Know your number’
It is a good idea to tell patients their NP level. Patients like to have this information and, in theory, this might help to improve compliance with their therapy. Also, if the patient is ill when away from home it could be useful for them to be able to report their usual NP level.
Members of the consensus group
Professor Martin Cowie (Imperial College, London) (chair), Professor Paul Collinson (St George’s Hospital, London), Professor Henry Dargie (Golden Jubilee National Hospital, Glasgow), Professor Richard Hobbs (University of Birmingham), Dr Theresa McDonagh (Royal Brompton Hospital, London), Professor Kenneth McDonald (St Vincent’s University Hospital, Dublin), Dr Nigel Rowell (GP, Middlesbrough).
Conflict of Interest
The consensus group was funded by an unrestricted educational grant from Roche Diagnostics, but Roche had no influence on the deliberations or in the preparation of the manuscript.
What do the guidelines say?
- The 2003 NICE heart failure guideline recommends use of NPs in diagnosis “where available”. This guideline is currently being updated and the revised version (due to be published in 2010) is expected to give a stronger recommendation for use of the test
- The 2007 Scottish Intercollegiate Guidelines Network (SIGN) guideline on chronic heart failure has a firm recommendation for NP measurement in its diagnostic algorithm, in response to the findings of an HTA by NHS Quality Improvement Scotland3
- The 2008 European Society of Cardiology (ESC) heart failure guideline says that there is evidence supporting the use of NPs in diagnosing, staging, making hospitalisation/discharge decisions, and identifying patients at risk for clinical events27
References
- Healthcare Commission. Pushing the boundaries: improving services for people with heart failure. London: Healthcare Commission, 2007.
- Mant J, Doust J, Roalfe A et al. Systematic review and individual patient data meta-analysis of diagnosis of heart failure, with modelling of implications of different diagnostic strategies in primary care. Health Technol Assess 2009;13(32).
- Craig J, Bradbury I, Cummins E et al. The use of B-type natriuretic peptides (BNP and NT-proBNP) in the investigation of patients with suspected heart failure. Glasgow: NHS Quality Improvement Scotland, 2005.
- Maisel AS, Krishnaswamy P, Nowak RM et al. Rapid measurement of B-type natriuretic peptide in the emergency diagnosis of heart failure. N Engl J Med 2002;347:161–7.
- Januzzi JL, Van Kimmenade R, Lainchbury J et al. NT-proBNP testing for diagnosis and short-term prognosis in acute destabilised heart failure: an international pooled analysis of 1256 patients. Eur Heart J 2006;27:330–7.
- Fuat A, Murphy JJ, Hungin APS et al. The diagnostic accuracy and utility of a B-type natriuretic peptide test in a community population of patients with suspected heart failure. Br J Gen Pract 2006;56:327–33.
- Hildebrandt P, Collinson PO. Amino-terminal pro-B-type natriuretic peptide testing to assist the diagnostic evaluation of heart failure in symptomatic primary care patients. Am J Cardiol 2008; 101:25A-28A.
- Lim TK, Collinson PO, Celik E, Gaze D, Senior R. Value of primary care electrocardiography for the prediction of left ventricular systolic dysfunction in patients with suspected heart failure. Int J Cardiol 2007;115:73–4.
- Collinson PO. The cost effectiveness of B-type natriuretic peptide measurement in the primary care setting – a UK perspective. Congest Heart Fail 2006;12:103–07.
- Galasko GIW, Barnes SC, Collinson P et al. What is the most cost-effective strategy to screen for left ventricular systolic dysfunction: natriuretic peptides, the electrocardiogram, hand-held echocardiography, traditional echocardiography, or their combination? Eur Heart J 2006;27:193–200.
- Mueller C, Laule-Kilian K, Schindler C et al. Cost-effectiveness of B-type natriuretic peptide testing in patients with acute dyspnea. Arch Intern Med 2006;166:1081–7.
- Fonarow GC, Peacock WF, Phillips CO et al. Admission B-type natriuretic peptide levels and in-hospital mortality in acute decompensated heart failure. J Am Coll Cardiol 2007;49:1943–50.
- Maisel A, Hollander JE, Guss D et al. Primary results of the Rapid Emergency Department Heart Failure Outpatient Trial (REDHOT). A multicentre study of B-type natriuretic peptide levels, emergency department decision making, and outcomes in patients presenting with shortness of breath. J Am Coll Cardiol 2004;44:1328–33.
- Bettencourt P, Azevedo A, Pimenta J et al. N-terminal-pro-brain natriuretic peptide predicts outcome after hospital discharge in heart failure patients. Circulation 2004;110:2168–74.
- Logeart D, Thabut G, Jourdain P et al. Predischarge B-type natriuretic peptide assay for identifying patients at high risk of re-admission after decompensated heart failure. J Am Coll Cardiol 2004;43:635–41.
- Cheng V, Kazanagra R, Garcia A et al. A rapid bedside test for B-type natriuretic peptide predicts treatment outcomes in patients admitted for decompensated heart failure: a pilot study. J Am Coll Cardiol 2001;37:386–91.
- Valle R, Aspromonte N, Giovinazzo P et al. B-type natriuretic peptide-guided treatment for predicting outcome in patients hospitalized in sub-intensive care unit with acute heart failure. J Cardiac Fail 2008;14:219–24.
- Gardner RS, McDonagh TA, MacDonald M et al. Who needs a heart transplant? Eur Heart J 2006;27:770–2.
- Berger R, Huelsman M, Strecker K et al. B-type natriuretic peptide predicts sudden death in patients with chronic heart failure. Circulation 2002;105:2392–7.
- Pfisterer M, Buser P, Rickli H et al. BNP-guided vs symptom-guided heart failure therapy. The trial of intensified vs standard medical therapy in elderly patients with congestive heart failure (TIME-CHF) randomized trial. JAMA 2009;301:383–92.
- Felker GM, Hasselblad V, Hernandez AF, O’Connor CM. Biomarker-guided therapy in chronic heart failure: a meta-analysis of randomized controlled trials. Am Heart J 2009;158:422–30.
- O’Hanlon R, O’Shea P, Ledwidge M et al. The biologic variability of B-type natriuretic peptide and N-terminal pro-B-type natriuretic peptide in stable heart failure patients. J Cardiac Fail 2007;13:50–5.
- Miller WL, Hartman KA, Grill DE et al. Only large reductions in concentration of natriuretic peptides (BNP and NT-proBNP) are associated with improved outcome in ambulatory patients with chronic heart failure. Clin Chem 2009;55:78–84.
- McDonagh TA, Robb SD, Murdoch DR et al. Biochemical detection of left-ventricular systolic dysfunction. Lancet 1998;351:9–13.
- Krauser DG, Lloyd-Jones DM, Chae CU et al. Effect of body mass index on natriuretic peptide levels in patients with acute congestive heart failure: a proBNP investigation of dyspnea in the emergency department (PRIDE) substudy. Am Heart J 2005;149:744–50.
- Frankenstein L, Remppis A, Nelles M et al. Relation of N-terminal pro-brain natriuretic peptide levels and their prognostic power in chronic stable heart failure to obesity status. Eur Heart J 2008;29:2634–40.
- Dickstein K, Cohen-Solal A, Filippatos G et al. European Society of Cardiology guidelines for the diagnosis and treatment of acute and chronic heart failure 2008. Eur Heart J 2008;29:2388–442.
