The Cardiac Prevention & Rehabilitation Service (CP&R) at Imperial College Healthcare NHS Trust in London uses both community- and hospital-based programmes. A community-based programme, called MyAction, serves the Westminster population, while a hospital-based service from Charing Cross Hospital serves the Hammersmith and Fulham population, and also accepts patients from Hounslow, Ealing and other areas.
The service at Charing Cross was used as the model for EUROACTION, a randomised, controlled trial of a preventive cardiology programme, conducted in eight European countries, including the UK. This nurse-led multidisciplinary programme significantly improved the management of lifestyle and medical risk factors for cardiovascular disease prevention in coronary patients and patients at high multifactorial risk for developing heart disease.1 The principles of the EUROACTION programme were used to found The MyAction community programme, commissioned in 2008 by NHS Westminster as a model for preventive cardiology care for its residents.
The Imperial College Healthcare NHS Trust CP&R programmes follow relevant guidelines and targets set out by the National Service Framework (NSF) for Coronary Heart Disease,2 the National Institute for Health and Clinical Excellence (NICE) guidance on secondary prevention post-myocardial infarction;3 the Joint British Societies’ recommendations on prevention of coronary heart disease in clinical practice;4 and the British Association for Cardiac Rehabilitation (BACR) Standards and Core Components for Cardiac Rehabilitation.5
In-patient care

Patients are admitted to the Trust from Primary Care Trusts within North West London for investigation and treatment. They are identified by a CP&R nurse, receive education and support (table 1), and are referred to their local cardiac rehabilitation centre on discharge. Between April 2009 and March 2010, a total of 1,100 patients received this service from the Charing Cross Hospital team.
The Charing Cross programme
Initial assessment
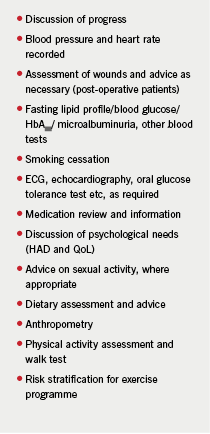
Patients referred to the Charing Cross Hospital programme are seen with family members in a nurse-led clinic within two weeks of discharge. Unless there is a specific clinical issue, patients will not see a doctor at this initial assessment. During the two-hour out-patient appointment (see table 2), a clinical nurse specialist (CNS) will undertake a holistic assessment of the patient and arrange any test or referrals required. A dietitian and an exercise specialist will also assess the patient.
A personalised CP&R plan which addresses individual needs and priorities is developed; all patients are offered the opportunity to undertake a group or home CP&R programme.
The multi-disciplinary team
At Charing Cross Hospital the multi-disciplinary team (MDT) meets weekly to discuss all patients who have had an initial assessment: the team includes a consultant cardiologist, nurse specialists, a dietitian, a cardiac exercise specialist and a clinical psychologist. Lifestyle, medical risk factors and laboratory results are reviewed. Medication is also reviewed, changed and up-titrated as required to national targets. Patients with psychological issues, such as high anxiety and depression scores, are discussed with the clinical psychologist and referred if necessary.
Patients who have already started the programme are also reviewed at the MDT meeting. Feedback is given at the start of each class by the CNS or, for those patients undertaking a home programme, via the GP.
The programme
Patients begin the programme within two weeks of the initial assessment. Those attending the group session are invited to eight weekly sessions and are given a concurrent home physical activity programme to follow. They receive a weekly health education talk and ongoing risk factor management and support. The programme has the capacity for a seated exercise circuit and, more recently, a separate low functional capacity class (including those with heart failure) has been set up. The nurse specialist reviews each patient’s personal plan, blood pressure, medication and blood test results throughout the programme.
Home programmes are delivered via the Heart Manual, a pedometer programme or a home exercise programme. The Heart Manual is used to provide health education and support for all three home programmes. Patients choosing this option are reviewed in the nurse-led clinic after four weeks and any set targets and medication are reviewed.
The re-assessment appointment
All patients are reviewed after completion of the programme, with the appointment having a similar content to the initial assessment. Progress is summarised and patients are referred to a community-based cardiac exercise class if they wish. Any outstanding issues, such as further improvement in lipid control, are discussed at the MDT and are then communicated to the patient and the GP.
Results
For the period 2008–2009, a total of 240 patients completed the programme and attended a re-assessment appointment. Results are summarised below.
Physical activity: at the initial appointment, 7% of patients reported undertaking 30 minutes of moderate intensity activity five days of the week. After the programme this had increased to 58%.6
Anthropometry: data for body mass index (BMI) and waist circumference show little difference from the start to the end of the programme. A snapshot of patients’ views on weight loss indicated that priority was given to other issues, such as smoking cessation, lipid modification and coping with anxiety. As a result, a weight management class was established for patients with a raised BMI at re-assessment. The first three cohorts achieved an average weight loss of 3 kg over 12 weeks.6
Smoking: only 20% of smokers had stopped at the time of their re-assessment. Following discussion with the MDT, a CP&R nurse has been given specific responsibility for smoking cessation. Smokers are now more intensively monitored as they pass through the programme.6
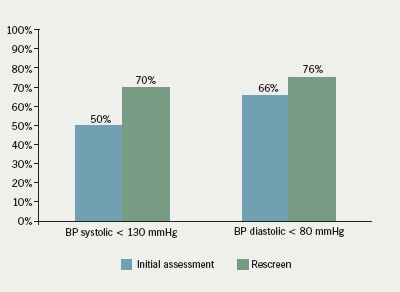
Achievement of blood pressure targets: figure 1 shows that by the end of the programme, 70% of patients were achieving the relatively stringent target of a systolic blood pressure (BP) of <130 mmHg, with 76% achieving a diastolic BP <90 mmHg.6
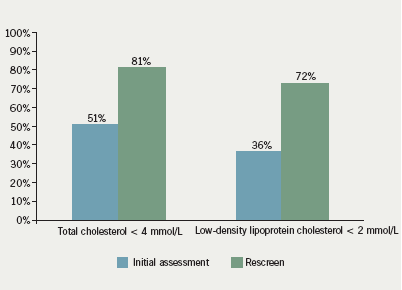
Achievement of lipid targets: figure 2 shows that a total cholesterol level of less than 4 mmol/L was achieved in 81% of patients on completion of the CP&R. In all, 72% achieved low-density lipoprotein cholesterol (LDL-C) levels of less than 2 mmol/L. Lipids were checked several times during the programme and medication changed as indicated.6
Cardioprotective medication: by the end of the programme, 98% of patients were on aspirin, 80% were taking a beta blocker, 88% were taking either an angiotensin-converting enzyme (ACE) inhibitor or angiotensin receptor blocker, and 98% were on a statin.6
Patient satisfaction: at the re-assessment, 83% of patients rated their satisfaction with the CP&R programme as either excellent or very good. When asked if they had made lifestyle changes during the programme, 92% said that they had.6
Uptake and attendance 2009 – 2010
- Between April 2009 and March 2010, a total of 477 patients were referred from phase 1 to the Charing Cross Hospital programme. Of these, 374 (80%) attended the initial assessment.6
- Of the 374 patients who attended the initial assessment, 332 (87%) attended
the programme, with a completion rate of 305 (92%).6 - Of the 305 who completed the class, 244 (80%) attended a re-screen appointment.6
Summary
The Imperial CP&R programme demonstrates that a nurse-led service, supported by a multi-disciplinary team, can produce a high-quality service which helps patients to achieve the recommended lifestyle and risk factor reduction targets for cardiovascular disease prevention.3,4 A flexible, menu-based approach to service delivery ensures that uptake of the programme is extremely high, achieving the requirements of the NSF and significantly exceeding the findings of the 2009 National Audit of Cardiac Rehabilitation6,7.
References
1. Wood DA, Kotseva K, Connolly S et al. Nurse-coordinated multidisciplinary, family-based cardiovascular disease prevention programme (EUROACTION) for patients with coronary heart disease and asymptomatic individuals at high risk of cardiovascular disease: a paired, cluster-randomised controlled trial. Lancet. 2008;371(9629):1999–2012.
2. Department of Health. Coronary Heart Disease: National Service Framework for a coronary heart disease – modern standards and service models. London: The Stationery Office, 2000.
3. National Institute for Health and Clinical Excellence. Secondary prevention in primary and secondary care following myocardial infarction. Clinical Guidelines CG 48. London: NICE, 2007.
4. Joint British Societies. JBS 2: Joint British Societies’ recommendations on prevention of coronary heart disease in clinical practice. Heart 2005;91 (suppl 5):v1–v52.
5. British Association of Cardiac Rehabilitation, 2007. Standards and Core Components for Cardiac Rehabilitation. www.tinyurl.com/3ydagw
6. Charing Cross & Hammersmith Hospitals (data on file).
7. National Audit of Cardiac Rehabilitation: Annual Statistical Report 2009. www.cardiacrehabilitation.org.uk/docs/2009.pdf
