Worldwide, cardiovascular disease remains the leading cause of death and a major cause of disability affecting quality of life.1 Elevated cholesterol is one of the key risk factors accounting for a substantial proportion of this disease burden. In developed countries, at least one-third of all cardiovascular disease is attributable to five risk factors: smoking, excessive alcohol intake, elevated blood pressure, elevated cholesterol and obesity.2 In particular, elevated cholesterol accounted for 56% of all cases of coronary heart disease (CHD) and 18% of cases of ischaemic stroke (2002 data).2
Improved management of risk factors and better care, especially in the secondary prevention setting, has undoubtedly been successful in reducing cardiovascular disease mortality in the UK over the last few decades.3 Better care of patients after myocardial infarction (MI) has also increased the longevity of these patients.3 However, these gains are now seriously challenged by the impact of the global epidemics of obesity and type 2 diabetes, arising from overconsumption and an increasingly sedentary society. As clinicians, we need to rise to this challenge to improve management.
Improving guideline implementation
Improved control of cholesterol, one of the key risk factors associated with cardiovascular disease, is one priority. Statin therapy is clearly recognised in guidelines as the cornerstone of treatment for managing dyslipidaemia.4 However, implementation is still less than optimal. In the primary care setting, EURIKA (European Study on Cardiovascular Risk Prevention and Management in Usual Daily Practice) showed that less than one-half of treated dyslipidaemic patients attained both total and low-density lipoprotein (LDL) cholesterol targets.5 Similarly, in the secondary prevention setting, the EUROASPIRE (European Action on Secondary and Primary Prevention by Intervention to Reduce Events) III survey showed that only 55% of patients across Europe achieved total cholesterol targets. It has to be pointed out that control was somewhat better in the UK (72% of patients achieved total cholesterol targets) compared with the average for all countries.6
More aggressive statin therapy, in accordance with local guidance, can further improve LDL cholesterol lowering. However, LDL cholesterol lowering alone does not eliminate the risk of cardiovascular events.7
Considering other lipid targets: HDL cholesterol
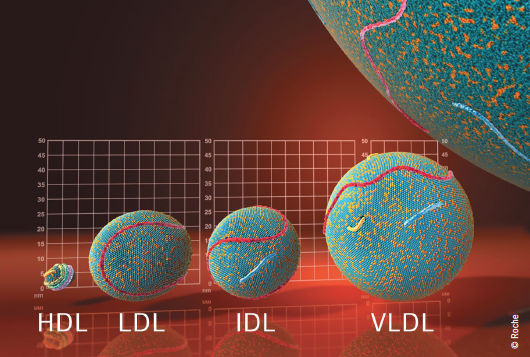
The INTERHEART Study, a global case–control study, highlighted the relevance of both atherogenic apolipoprotein (apo) B-containing lipids, including LDL cholesterol, intermediate-density and very low-density lipoproteins, and atheroprotective lipoproteins, such as apoA-I contained in high-density lipoprotein (HDL) cholesterol to coronary risk. The study showed that, after smoking, the ratio of apoB/apoA-I was the most important contributor to population-attributable MI risk, accounting for almost one-half (49.2%) of this risk. Individuals with apoB/apoA-I ratios in the highest quintile had over three-fold increase in population attributable MI risk.8 In INTERSTROKE, there was also a strong association between apoA-I and HDL cholesterol levels and the risk of ischaemic stroke.9 These data clearly emphasise that achieving the right balance between atherogenic and atheroprotective lipoproteins can favourably impact the atherosclerotic process and reduce cardiovascular events.
Atherosclerosis is an inflammatory process which occurs over many decades. The initial trigger for this process is the accumulation of apoB-containing lipoproteins in the artery wall.10 These then undergo oxidation, with the end products (oxidised LDL) then stimulating further processes involved in atherosclerosis. As a result, monocytes are attracted to the endothelial layer, attach to the endothelium, and migrate into the subendothelial space, where the monocytes differentiate into macrophages. Macrophages take up the modified LDL, becoming foam cells, and also release a number of chemicals, including cytokines and interleukin-1, leading endothelial cells to express adhesion molecules, which, in turn, bind monocytes to the endothelium, thus, continuing the cycle of atherosclerosis. Macrophages and foam cells secrete growth factors, which lead to cell proliferation and matrix production, as well as metalloproteinases, which lead to matrix degeneration. Thus, macrophages and foam cells contribute to lesion growth, plaque instability and ultimately clinical events.
Evidence from in vitro and in vivo studies points to HDL having a number of important atheroprotective properties that can help in slowing this process. HDL comprise a heterogeneous population of lipoproteins that differ by size, shape and composition. Essentially, HDL have the same structure as LDL, with a surface monolayer of phospholipids and free cholesterol and a hydrophobic core consisting mainly of cholesteryl esters, as well as some triglyceride.10,11
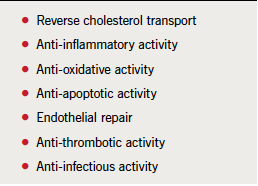
HDL play a key role in reverse cholesterol transport, the process by which excess cholesterol is transferred from macrophage foam cells in the arterial wall or peripheral tissues to the liver for excretion into the bile. However, HDL have other potentially atheroprotective functions including anti-inflammatory, anti-oxidative, and anti-thrombotic activities (table 1).11 HDL also play a role in stabilising atherosclerotic plaque.12 An analysis of four intravascular ultrasound studies involving 1,455 patients showed that both LDL cholesterol lowering and HDL cholesterol raising were relevant to atheroma progression.13
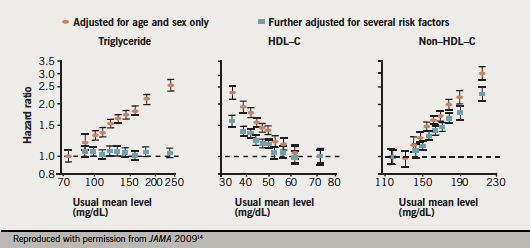
The epidemiological evidence base for the association of HDL cholesterol and cardiovascular risk is indisputable. The largest analysis to date, the ERFC (Emerging Risk Factors Collaboration) in more than 300,000 individuals without cardiovascular disease at baseline, provides the strongest evidence (figure 1). After adjustment for both lipid and non-lipid risk factors, each 0.38 mmol/L (15 mg/dL) increment in HDL cholesterol was associated with 22% reduction in CHD risk. A significant relationship was also shown for HDL cholesterol and risk of ischaemic stroke. However, the relationship between the level of HDL cholesterol and coronary risk appeared to plateau at 1.6 mmol/L (∼61 mg/dL).14 The jury is still out on whether raising HDL cholesterol levels beyond this value confers additional clinical benefit.
Current guidelines identify HDL cholesterol as a strong cardiovascular risk factor but refrain from identifying HDL cholesterol as a target for intervention given the lack of outcomes data.15 HDL cholesterol is incorporated in SCORE risk estimation charts as it has been shown to contribute to risk as the individual variable but not as the ratio.15 Clinically, HDL cholesterol can be readily measured in non-fasting samples as a simple marker of cardiovascular disease risk. Non-HDL cholesterol (or apoB) is a preferable measure of atherogenic apoB-containing lipoproteins to LDL cholesterol, and also readily measured in non-fasting samples (see practice point). Considering management strategies for low HDL cholesterol may be relevant in the overweight individual with the metabolic syndrome.
Relevance of inflammatory biomarkers?
There has been much debate about incorporation of inflammatory factors in risk estimation. Because C-reactive protein (CRP) is present in atherosclerotic plaques, it has been proposed that it may have a causal role in cardiovascular disease. Indeed, another comprehensive analysis by the ERFC showed that CRP levels were linearly associated with an increased risk of cardiovascular events, although more modestly than previously believed.16 It is, however, unlikely that CRP is causal as genes associated with elevations in CRP are not associated with increased risk of CHD, suggesting that CRP is a marker of risk rather than a target for treatment.17 However, this does preclude the potential causal role of inflammation with upstream factors such as interleukin 1 or 6, as progression from a stable to unstable atherosclerotic plaque culminating in the clinical event undoubtedly involves inflammation and the complex interplay of genetic and environmental risk factors.
The balance of evidence from epidemiological and mechanistic studies supports the HDL hypothesis. Whether raising HDL cholesterol levels translates to reduction in cardiovascular outcomes is being tested by several ongoing major prospective studies (see review on pages S14–S16) and answers should be available within the next two to four years. Finally, outstanding questions remain as to whether HDL cholesterol levels or the biological activities of HDL (i.e. its functionality) are more important. The HDL cholesterol hypothesis remains an intriguing concept, for which we hope to have definitive answers in the near future.
Key messages
- Achieving the right balance between atherogenic lipoproteins (as in LDL) and atheroprotective lipoproteins (as in HDL) is key to reducing cardiovascular risk
- HDL has been shown to have a number of atheroprotective properties
- Epidemiological data confirm HDL cholesterol as an independent risk factor for cardiovascular disease
- Ongoing clinical trials will help to determine whether HDL cholesterol is a target or only a risk factor
References
- World Health Organization. The top 10 causes of death. Fact sheet N°310, June 2011. Available at: http://www.who.int/mediacentre/factsheets/fs310/en/index.html [accessed 13 December 2011].
- World Health Organization. The Atlas of Heart Disease and Stroke. Part 2 Risk factors. Available from: http://www.who.int/cardiovascular_diseases/resources/atlas/en/ [accessed 12 December 2011].
- Unal B, Critchley JA, Capewell S. Explaining the decline in coronary heart disease mortality in England and Wales between 1981 and 2000. Circulation 2004;109:1101–07. http://dx.doi.org/10.1161/01.CIR.0000118498.35499.B2
- National Collaborating Centre for Primary Care. NICE Clinical guideline 67. Lipid modification. Cardiovascular risk assessment and the modification of blood lipids for the primary and secondary prevention of cardiovascular disease. May 2008. Quick reference guide. Available at: http://guidance.nice.org.uk/CG67/QuickRefGuide/pdf/English [accessed 5 January 2012].
- Banegas JR, López-García E, Dallongeville J et al. Achievement of treatment goals for primary prevention of cardiovascular disease in clinical practice across Europe: the EURIKA study. Eur Heart J 2011;32:2143–52. http://dx.doi.org/10.1093/eurheartj/ehr080
- Kotseva K, Wood D, De Backer G et al.; EUROASPIRE Study Group. EUROASPIRE III: a survey on the lifestyle, risk factors and use of cardioprotective drug therapies in coronary patients from 22 European countries. Eur J Cardiovasc Prev Rehabil 2009;16:121–37. http://dx.doi.org/10.1097/HJR.0b013e3283294b1d
- Cholesterol Treatment Trialists’ (CTT) Collaboration, Baigent C, Blackwell L, Emberson J et al. Efficacy and safety of more intensive lowering of LDL cholesterol: a meta-analysis of data from 170,000 participants in 26 randomised trials. Lancet 2010;376:1670–81. http://dx.doi.org/10.1016/S0140-6736(10)61350-5
- Yusuf S, Hawken S, Ounpuu S et al.; INTERHEART Study Investigators. Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): case-control study. Lancet 2004;364:937–52. http://dx.doi.org/10.1016/S0140-6736(04)17018-9
- O’Donnell MJ, Xavier D, Liu L et al. Risk factors for ischemic and intracerebral haemorrhagic stroke in 22 countries (the INTERSTROKE study): a case-control study. Lancet 2010;376:112–23. http://dx.doi.org/10.1016/S0140-6736(10)60834-3
- Barter P. The role of HDL cholesterol in preventing atherosclerotic disease. Eur Heart J 2005;7(suppl F):F4–F8. http://dx.doi.org/10.1093/eurheartj/sui036
- Rye KA, Bursill CA, Lambert G, Tabet F, Barter PJ. The metabolism and anti-atherogenic properties of HDL. J Lipid Res 2009;50(suppl):S195–S200. http://dx.doi.org/10.1194/jlr.R800034-JLR200
- Ibanez B, Giannarelli C, Cimmino G et al. Recombinant HDL(Milano) exerts greater anti-inflammatory and plaque stabilizing properties than HDL(wild-type). Atherosclerosis 2012;220:72–7. http://dx.doi.org/10.1016/j.atherosclerosis.2011.10.006
- Nicholls SJ, Tuzcu EM, Sipahi I et al. Statins, high-density lipoprotein cholesterol, and regression of coronary atherosclerosis. JAMA 2007;297:499–508. http://dx.doi.org/10.1001/jama.297.5.499
- The Emerging Risk Factors Collaboration. Major lipids, apolipoproteins, and risk of vascular disease. JAMA 2009;302:1993–2000. http://dx.doi.org/10.1001/jama.2009.1619
- Reiner Z, Catapano AL, De Backer G et al. ESC/EAS guidelines for the management of dyslipidaemias: the Task Force for the management of dyslipidaemias of the European Society of Cardiology (ESC) and the European Atherosclerosis Society (EAS). Eur Heart J 2011;32:1769–818. http://dx.doi.org/10.1093/eurheartj/ehr158
- Emerging Risk Factors Collaboration, Kaptoge S, Di Angelantonio E, Lowe G et al. C-reactive protein concentration and risk of coronary heart disease, stroke and mortality: an individual participant meta-analysis. Lancet 2010;375:132–40. http://dx.doi.org/10.1016/S0140-6736(09)61717-7
- Elliott P, Chambers JC, Zhang W et al. Genetic loci associated with C-reactive protein levels and risk of coronary heart disease. JAMA 2009;302:37–48. http://dx.doi.org/10.1001/jama.2009.954
Practice point
 Non-HDL-C, LDL-C and apoB: what do they measure?
Non-HDL-C, LDL-C and apoB: what do they measure?
Non-HDL cholesterol = the sum of cholesterol in all atherogenic apolipoprotein B (apoB) containing lipoprotein particles (i.e. low-density lipoprotein [LDL] + intermediate-density lipoprotein [IDL] + very-low-density lipoprotein [VLDL]) = Total cholesterol – HDL cholesterol
LDL cholesterol = cholesterol in LDL. Calculated using Friedewald’s formula (invalid if non-fasting or if triglycerides [TG] >4.5 mmol/L)
ApoB = the total number of atherogenic apoB lipoprotein particles in LDL + IDL + VLDL. Useful in diagnosis but no advantage over non-HDL cholesterol in risk assessment14