Highlights of the recent American College of Cardiology (ACC) meeting, 24th–27th March 2012, held in Chicago, USA, included a study showing the benefit of CT scans in diagnosing chest pain, more about the role of LDL in the body, and a study raising concern over not treating hypertension in the young.
CORONARY: off-pump and on-pump CABG similar
The largest trial ever to compare off-pump and on-pump coronary artery bypass surgery (CABG) has shown no difference between the two techniques in terms of the primary composite end point. There were, however, some differences in certain end points, leading to the suggestion that the decision as to which approach to choose could be individualised with each patient.
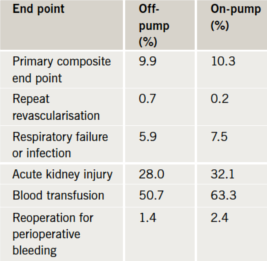
The CORONARY trial enrolled 4,752 patients who were randomised to off-pump or on-pump surgery. At 30 days the primary end point – a composite of death, myocardial infraction (MI), kidney failure and stroke, were similar in both groups. But off-pump surgery was associated with fewer transfusions, reoperations for bleeding and pulmonary complications, while on-pump surgery showed fewer revascularisations (table 1).
Presenting the results, Dr André Lamy (McMaster University, Canada) said that surgeons should train in both methods and decide which approach would be best for each individual patient. For a patient with some kidney dysfunction, off-pump might be better, while for someone with diabetes and diffuse disease, on-pump may be preferable in terms of the revascularisation results.
Further results from the trial will include neurocognitive and cost results as well as five-year follow-up.
GIK may still have a role in MI patients
After many negative trials, the combination of glucose-insulin-potassium (GIK) has finally shown some positive effects in myocardial infarction (MI) patients in its latest study. In the IMMEDIATE trial, giving GIK in the first hours of a suspected acute coronary syndrome (ACS) event, did not improve 30-day survival rates but it was associated with reductions in the end point of cardiac arrest or in-hospital mortality, and in infarct size among patients who underwent cardiac imaging at 30 days.
Dr Harry Selker (Tufts Medical Center, Boston, USA), who presented the trial, cited experimental data suggesting that GIK provided metabolic support to the heart in the ACS setting, protecting the myocardium and preventing arrhythmias.
Dr Selker speculated that previous trials may have shown no benefit of GIK because it was given too late. In the current trial, GIK was administered by paramedics at the first signs of an MI in the community. He said the
US$ 50 treatment appears to have promise in reducing mortality and morbidity from MI if given early.
The researchers are continuing to follow patients up to 12 months.
ROMICAT II – CT scans improve diagnosis of MI in ER
Use of computed tomography (CT) scans to evaluate patients with chest pain in the emergency room (ER) can save time and money in the diagnosis of myocardial infarction, according to the ROMICAT II study.
The study, in 1,000 patients with chest pain from nine US centres, showed that using CT scans reduced the average time spent in hospital by 18 hours. Half of the patients receiving the scan were safely discharged within nine hours compared to only 15% of patients receiving standard care. The use of CT resulted in 10-20% cost savings over standard care.
Lead investigator, Dr Udo Hoffmann (Massachusetts General Hospital, Boston, USA) said: “CT allows you to spend your healthcare dollars focusing on the people who are actually sick.” He added that the scans also provided useful prognostic information that can be referred back to if the patient experiences chest pain again.
Other studies have shown conflicting results on the use of CT scans in chest pain patients. This trial is different as the scan was done earlier in the evaluation process.
Surgery best option for obese patients with uncontrolled diabetes
Bariatric surgery is more effective than intensive medical management for both weight loss and in reducing blood sugar levels in obese, uncontrolled type 2 diabetes patients, according to the STAMPEDE trial.
STAMPEDE, the first randomised controlled trial to compare surgery with intensive medical therapy in helping patients with diabetes achieve blood sugar goals, included 150 patients who were randomly assigned to:
- intensive medical therapy only
- medical therapy plus gastric bypass or
- medical therapy plus sleeve gastrectomy.
The primary end point was achievement of an HbA1c of ≤ 6.0%. This was achieved in 12.2% of the medical treatment group versus 42% for gastric bypass and 36.7% for sleeve gastrectomy. Surgery patients also showed significantly greater weight loss (around 60 pounds compared to 12 pounds in the medication alone group), and reduced reliance on medications.
At the start of the trial, the average patient had an HbA1c of 9.2%, had been living with uncontrolled diabetes for eight or more years and was taking three or more antidiabetic medications and three or more cardiovascular medications. There was, however, a higher rate of complications in the surgery groups, with short-term dehydration, bleeding and one leak, and 4% of patients needed operative intervention to manage complications occurring within the 12-month follow-up period.
Lower LDL early in life for best results
Lowering low-density lipoprotein (LDL) cholesterol beginning early in life results in a three-fold greater reduction in the risk of coronary heart disease (CHD) than treatment with a statin started later in life, the results of a new ‘natural’ randomised trial suggest.
Dr Brian Ference (Wayne State University School of Medicine, US) explained how his team studied the effect of nine single-nucleotide polymorphisms (SNPs), each of which is associated with lower levels of LDL cholesterol. Because each of these SNPs is allocated randomly at the time of conception, inheriting one of these SNPs is like being randomly allocated to a treatment that lowers LDL cholesterol beginning at birth. Dr Ference found that all nine SNPs were associated with a consistent 50–60% reduction in the risk of CHD for each 1 mmol/L lower lifetime exposure to LDL cholesterol.
“The increased benefit of lowering LDL beginning early in life appeared to be independent of how LDL was lowered. This means that diet and exercise are probably as effective as statins or other medications at reducing the risk of CHD when started early in life,” he said.
Designated discussant of the study, Dr Noel Bairey Merz (Cedars-Sinai Medical Center, Los Angeles, USA) said: “The big public-health question is whether it is better to start early and lower LDL in everyone rather than to wait to find the high-risk subjects and just treat them later. And these data suggest it is better to go for the first option; you get three times more bang for your buck that way.”
Low LDL predates cancer risk by decades
The debate about whether low low-density lipoprotein (LDL) cholesterol is associated with cancer risk has been reignited with a new study showing that low LDL cholesterol in patients with no history of taking cholesterol-lowering drugs predates cancer risk by decades.
“There has been some debate as to whether or not medications used to lower cholesterol may contribute to cancer, but the evidence so far tells us that the drugs themselves do not increase the risk of cancer. We wanted to take those medications out of the equation and just look at the link between cancer and low LDL cholesterol in people who had never taken cholesterol-lowering drugs,” said Paul Michael Lavigne (Tufts Medical Center, Boston, USA).
He reported a matched case control study, using data from the Framingham Heart Study Offspring Cohort, and compared 201 cancer cases with 402 controls matched for many factors including age, gender, diabetes, smoking status, blood pressure and body mass index.
Results showed that LDL cholesterol values were lower in cancer subjects than matched controls at each of four time points throughout an average of 18.7 years prior to cancer diagnosis. “There is no evidence to indicate that lowering your cholesterol with a medication in any way predisposes to a risk for cancer. We suspect there may be some underlying mechanism affecting both cancer and low LDL,” he concluded.
Hypertension in young needs closer attention
The current practice of not treating hypertension in younger people may be leading to irreversible heart damage, according to a UK study. The study found that a sharp rise in blood pressure in midlife can increase the risk of heart disease later in life, and that antihypertensive medications do not fully reverse this risk.
Dr Arjun Ghosh (Imperial College London) noted that antihypertesives are rarely prescribed for people in their 30s, as their risk of an event in the next 10 years is low. But he stated: “If people have a rapid rise in blood pressure, early treatment should be considered, because we know from this study that, 30 years down the line, they’re going to have more heart damage than somebody with a slower rise in blood pressure.”
The study has followed 1,653 men and women born in 1946. Participants were screened for blood pressure and other health indicators at ages 36, 43 and 53 years. From age 60–64 years, participants underwent echocardiography and results showed that people who experienced a relatively rapid increase in blood pressure during midlife typically had a larger left ventricle. Those taking antihypertensive medication had a larger left ventricle than those with the same blood pressure who had never taken medication, suggesting that treatment in later life did not reverse the consequences of a rapid rise in blood pressure in earlier years.
TRA2P TIMI-50: mixed results for vorapaxar
A new antiplatelet agent vorapaxar (Merck) with a novel mechanism of action, has shown some benefit in a secondary-prevention population in the TRA2P TIMI-50 trial, although bleeding will be a issue.
Study investigators suggested the drug, which blocks the protease-activated receptor 1 (PAR-1) on the platelet, does have a net clinical benefit in the subgroup patients with a prior myocardial infarction (MI) without a history of stroke or transient ischaemic attack (TIA) and who weighed over 60 kg. But outside commentators were worried about the high rate of intracranial haemorrhage (ICH) in the whole trial population.
TRA 2P TIMI 50 was conducted to investigate whether vorapaxar could reduce thrombotic events in stable patients with atherosclerosis treated for one year or more in addition to standard therapy. It included 26,449 patients who had had an MI or ischaemic stroke/TIA within the past year or who had peripheral arterial disease (PAD) who were randomised to vorapaxar 2.5 mg per day or placebo. Vorapaxar was discontinued early in patients with a history of stroke after an increase in ICH was seen in this group.
Results showed that after a median follow-up of 2.5 years, there was a significant 13% relative reduction in the primary efficacy end point (cardiovascular death/MI/stroke) for the whole patient population, with the greatest effect seen in the post-MI patients. But there was a significant increase in all measures of major bleeding, including ICH, with vorapaxar in the total population, although this was less severe in patients with no history of stroke.
Presenting the results, Dr David Morrow (Brigham and Women’s Hospital, Boston), estimated that for every 1,000 patients with no history of stroke/TIA and weight over 60 kg treated with vorapaxar, there would be 11 fewer MIs, six fewer cardiovascular deaths, and five fewer strokes, at the cost of two ICHs and 10 GUSTO moderate or severe bleeds
But one of the designated discussants, Dr Eduardo Marban (Cedars-Sinai Medical Center, Los Angeles), said he thought the benefits were limited although the risks are “not minor”.
