Multi-detector computed tomography coronary angiography (CTCA) is now an established highly effective non-invasive test in patients with chest pain and a low-to-intermediate pre-test likelihood of having coronary artery disease (CAD), as it has excellent sensitivity and negative predictive value (NPV).1 The limiting factors for CTCA are fast or irregular heart rate, a very high body mass index (BMI), the presence of extensive calcium in the coronary arteries and radiation. Recent introduction of prospectively gated acquisition in CTCA, where the acquisition is limited to 10% of the cardiac cycle at end-diastole, has dramatically reduced the radiation dose to 2–3 mSv for CTCA of the native coronary arteries, but this is only possible in patients with a regular rhythm below 60 bpm. Otherwise, retrospectively gated CTCA with electrocardiographically controlled tube current modulation (ECTCM) during the cardiac cycle keeps the dose below 10 mSv. The CTCA scan range in patients with coronary artery bypass grafts (CABG) is from the level of the subclavian arteries to below the diaphragm, which is twice the length of a CTCA for the native coronary arteries, and, hence, doubles the radiation dose. However, while the low-dose prospectively gated CTCA technique may not be possible in all patients having CTCA of the native coronary arteries, the minimal motion of the grafts means that CABG patients can be adequately imaged even with higher or irregular heart rates or higher BMI with the low-dose technique. The American College of Cardiology (ACC) has recently published appropriateness criteria for the use of CTCA, which included the use in patients with recurrent symptoms after CABG.2

Limitations
CTCA is highly accurate at detecting stenoses in bypass grafts with sensitivity, specificity, negative and positive predictive values of 97%, 97%, 93% and 99%, respectively.3 The limitation of CTCA in patients with CABG is in the assessment of the native coronary arteries distal to the grafts and the coronary arteries that did not receive bypass grafts at the time of CABG, as they tend to be heavily calcified and often of small calibre. This has limited the use of CTCA in CABG patients. However, invasive coronary angiography (ICA) in these patients can be a long and difficult procedure, particularly if both internal mammary arteries (IMA) have been used, and is associated with use of larger volumes of contrast and higher radiation doses than routine diagnostic ICA for native coronary arteries, which is a simple procedure comparatively. Furthermore, cardiac catheter manipulation to engage the IMA grafts is associated with a small risk of embolic strokes or dissection.
The use of CTCA in patients with CABG can be limited to the assessment of the patency of the grafts and the course of the IMA in relation to the sternum, which can be useful for the cardiac surgeons if the patient is being considered for re-do CABG. In some patients, the distal run offs and native arteries will be adequately seen and no further investigation will be needed. CABG patients are also likely to have functional tests for the assessment of the presence of ischaemia. The combined CTCA and functional assessment may adequately answer the clinical question; if not, then a limited ICA could be performed with relative ease and minimal use of iodinated contrast and radiation. In patients who are found to have stenotic grafts on CTCA, they can be listed for ICA with a view to proceeding to percutaneous coronary intervention (PCI) and the CTCA data can be used to reduce the procedure time, radiation and
contrast use.
Application
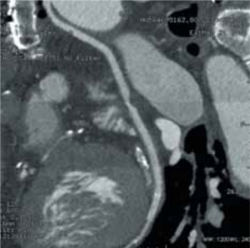
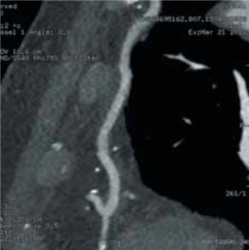
The following case demonstrates the useful application of CTCA to identify and assess grafts in a 79-year-old man with CABG who was admitted to a district general hospital with acute coronary syndrome where he had a prospectively gated CTCA to identify and assess his grafts (figures 1–3). This demonstrated a patent left IMA to left anterior descending (LAD) artery, a patent right IMA to distal right coronary artery (RCA), both with good run offs, a moderate stenosis in the middle of the saphenous vein graft (SVG) to obtuse marginal branch (OM), with a patent stent in the distal end of the vein graft with a good run off. A focused invasive coronary angiogram confirmed proximal total occlusions of the LAD, circumflex and RCA, and the moderate stenosis in the vein graft, which did not need interventio.
Conflict of interest
None declared.
References
- Meijboom WB, Van Mieghem CA, Mollet NR et al. 64-slice computed tomography coronary angiography in patients with high, intermediate, or low pretest probability of significant coronary artery disease. J Am Coll Cardiol 2007;50:1469–75.
- Taylor AJ, Cerqueira M, Hodgson JM et al. ACCF/SCCT/ACR/AHA/ASE/ASNC/NASCI/SCAI/SCMR 2010 appropriate use criteria for cardiac computed tomography. J Am Coll Cardiol 2010;56:1864–94. http://dx.doi.org/10.1016/j.jacc.2010.07.005
- Meyer TS, Martinoff S, Hadamitzky M et al. Improved noninvasive assessment of coronary artery bypass grafts with 64-slice computed tomographic angiography in an unselected patient population. J Am Coll Cardiol 2007;49:946–50. http://dx.doi.org/10.1016/j.jacc.2006.10.066
