We report the early and late results of coronary artery bypass graft (CABG) for protected and unprotected left main coronary artery (LMS) stenosis in an era of growing interest in LMS stenting.
We identified 1,707 patients who had CABG for LMS stenosis between February 1996 and December 2009, and compared their clinical characteristics and outcomes with a contemporaneous group of 6,260 people with non-LMS disease. A subgroup analysis of protected versus unprotected LMS cohorts was also performed. Follow-up data were 99.9% complete.
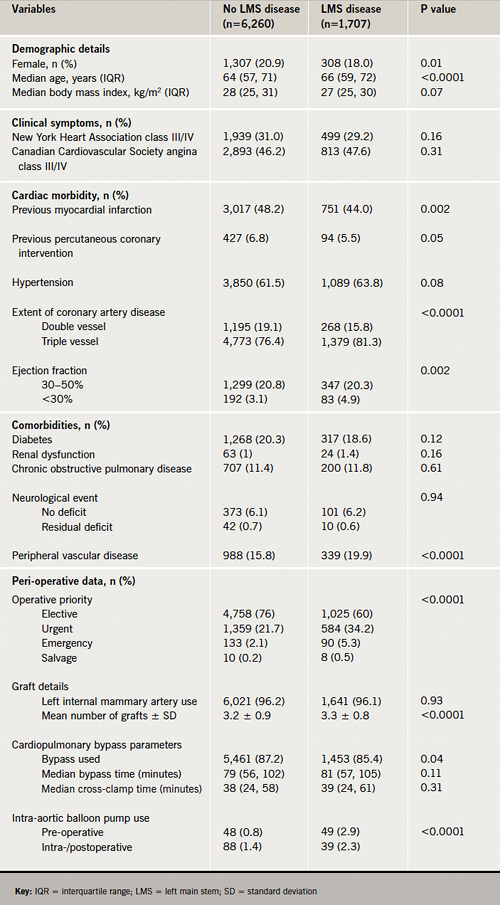
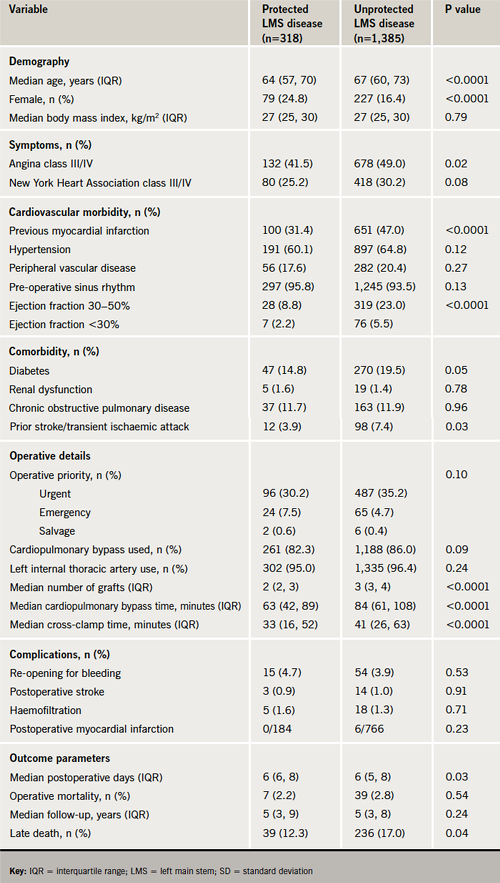
The LMS group, often male (82% vs. 79%, p=0.01) and older (mean 65.3 ± 9 vs. 63.6 ± 9 years, p<0.0001), frequently had ejection fraction <0.50 (25.2% vs. 23.9%, p=0.002) and urgent/emergency surgery (40% vs. 24%, p<0.0001). Overall, operative mortality was higher for the LMS group (2.7% vs. 1.1%, p<0.0001), and there was improvement over time (2.3% vs. 0.8% in the later period). There was no difference between protected and unprotected LMS cohorts (operative mortality 2.2 vs. 2.8, p=0.54).
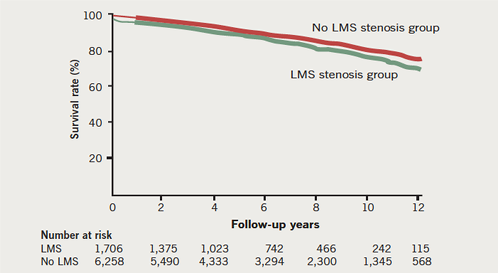
The respective 10-year survival rates for LMS and non-LMS patients were 75% and 79% (p=0.001). By multi-variate analysis, LMS stenosis was a predictor of operative mortality (odds ratio 2.05, 95% confidence interval 1.29–3.25, p=0.002) but not a determinant for late death.
In conclusion, CABG yields good early and late survival benefit for LMS stenosis (protected and unprotected), although operative result is adversely affected by LMS disease.
Introduction
Traditionally, coronary artery bypass grafting (CABG) was the preferred management strategy for left main stem (LMS) disease, but the success of percutaneous coronary intervention (PCI) with stenting for other anatomical variants of coronary artery disease has driven a growing interest in the same revascularisation strategy for LMS stenosis. However, PCI for LMS stenosis is not a low-risk procedure. Rathore and associates1 reported a 12-fold increase in the risk of death following PCI for LMS stenosis in a large retrospective study of 9,914 patients. In the setting of randomised clinical trials, however, procedural survival are comparable but late outcomes for PCI are marred by higher rates of re-intervention.2-4 The RESEARCH (Rapamycin-Eluting Stent Evaluated at Rotterdam Cardiology Hospital) and T-SEARCH (Taxus – Stent Evaluated at Rotterdam Cardiology Hospital) registries data5 showed a four-year mortality rate of 35.8% following PCI for LMS stenosis. At one year, the SYNTAX (Synergy between PCI with Taxus and Cardiac Surgery) trial reported lower rates of major adverse cardiac and cerebrovascular events with CABG compared with PCI for the subgroup of patients with LMS disease.3 The four-year data from the SYNTAX trial for all-comers, including patients with LMS stenosis, shows an overall progressive increase in all-cause (11.7% vs. 8.8%, p=0.048) and cardiac mortality rates (7.6% vs. 4.3%, p=0.004) for PCI compared with CABG.6
We, therefore, conducted this study to:
- elucidate the early and late clinical outcomes of CABG for LMS stenosis as compared with non-LMS stenosis
- determine if LMS stenosis imposes additional risk for early and late mortality after CABG.
Materials and methods
Patients
We obtained approval for this study from the local ethics committee and a waiver for individual patient consent. Prospectively collected pre-, intra- and post-operative data were then retrieved for all primary isolated CABG patients from April 1996 through December 2009 from the cardiothoracic surgery database of our hospital. Patients were divided into LMS (n=1,707) and non-LMS (n=6,260) groups. The LMS group was further subdivided into protected (n=318) or unprotected LMS (n=1,385) patients.
Survival data were obtained using the United Kingdom National Health Service tracking system in January 2011 and was 99.9% complete.
Statistical analysis
The primary outcome measures of interest were operative (in-hospital and/or 30-day) and long-term all-cause mortality.
Baseline clinical characteristics and outcome variables were compared between LMS and non-LMS groups; and between protected and unprotected LMS patients.
Categorical variables are presented as percentages and compared between groups, and subgroups with Pearson’s chi-square test, while continuous variables are presented as medians with the interquartile range or means with standard deviation and compared between the groups/subgroups using Mann-Whitney U-test or Student t-test, as appropriate. The independent effect of baseline variables (table 1), including LMS stenosis, on operative and late mortality were respectively assessed using 1,000 Bootstraps of a stepwise, multi-factorial logistic regression and Cox proportional hazards models. The odds ratio (OR) and 95% confidence interval (CI) for the predictors of operative mortality, and the hazard ratio (HR) and 95% CI for the determinants of late all-cause mortality are reported. The probability of long-term survival was estimated using the Kaplan-Meier methods and compared between the groups with log-rank test. The analysis was performed using the Statistical Package for the Social Sciences (SPSS) version 20.0 for Windows (IBM Corp, 2011, New York), and statistical significance was set at p≤0.05.
Results
Baseline characteristics
About 21% (n=1,707) of the 7,967 patients who underwent CABG during the study period had LMS stenosis. Patients with LMS stenosis were older, more often male, and tended to have more extensive coronary artery disease, peripheral vascular disease and severely impaired left ventricular systolic function, but were less likely to have had myocardial infarction and PCI, in comparison to those without LMS stenosis (table 1). The risk for operative mortality, as defined by the European System for Cardiac Operative Risk Evaluation (EuroSCORE), was higher for the LMS group. The mean additive EuroSCOREs were 3.8% for LMS and 3.2% for non-LMS patients (p=0.03). The requirement for peri-operative intra-aortic balloon pump and urgent/emergency CABG were more frequent for patients with LMS stenosis.
Early operative outcomes
In general, major postoperative cardiac, renal and neurological morbidity were observed in greater proportions of LMS stenosis patients (table 2).
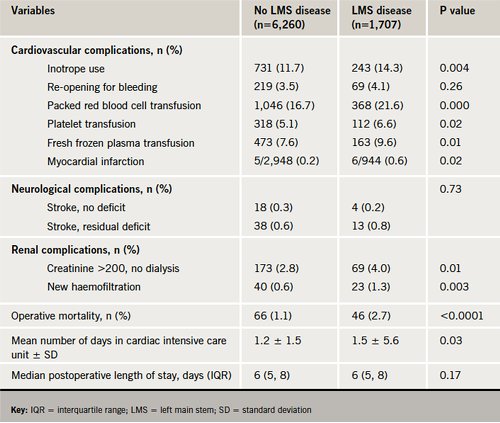
The operative mortality rate was higher for patients with LMS stenosis (2.7%) compared with non-LMS stenosis patients (1.1%, p<0.0001). Multi-factorial logistic regression analysis identified LMS stenosis (OR 2.02, 95% CI 1.26–3.22, p=0.003) as an independent predictor of operative mortality.
During the study period, there was a steady increase in the proportion of patients with LMS disease undergoing surgery, with a corresponding decline in operative mortality. From 1996 to 2000, there were a total of 2,126 CABG patients and 367 (17.3%) had LMS disease. In the later part of the study period, 2001 to 2009, there were 1,340 patients with LMS out of 5,841 (22.9%). The crude operative mortality rates for LMS patients dropped from 4.1% to 2.3%, and for non-LMS patients from 1.8% to 0.8%.
Late operative outcomes
During the follow-up period (maximum 15 years, mean 6.1 ± 3.7 years), there were 276 deaths (16.2%) among LMS stenosis patients compared with 941 (15.0%) for non-LMS stenosis patients. The probability of survival by Kaplan-Meier analysis at five and 10 years were 88% and 75% for LMS stenosis patients, compared with 91% and 79% for non-LMS stenosis group (p=0.001), respectively, as shown in figure 1. After controlling for other variables in a multi-variate analysis, however, left main coronary artery stenosis (HR 1.05, 95% CI 0.90–1.22, p=0.53) did not exhibit a significant influence on late death after CABG.
Subgroup analysis: protected versus unprotected LMS stenosis
The characteristics and outcomes for patients with protected and unprotected LMS stenosis are compared in table 3. Patients with unprotected LMS stenosis were more often male, older and presented with severe symptoms, cardiovascular morbidities and comorbidities more frequently than those with protected LMS stenosis. Despite these differences, the operative outcomes were comparable for both groups. In the long term, however, a significantly higher rate of late all-cause mortality was observed among the unprotected LMS patients compared with the protected LMS subgroup.
Discussion
Our study shows that increasing numbers of LMS stenosis patients are undergoing CABG and that, although LMS had direct and indirect associations with operative morbidity and mortality, the operative results are acceptable and steadily improving. The more regular co-existent with older age, cardiovascular morbidity and comorbidities on the one hand, and the frequent surgical exigency it imposes, contribute to the relatively higher adverse outcomes observed. Two decades ago, Chaitman et al.7 identified similar risk factors for operative mortality in 1,172 patients with LMS disease from the Collaborative Study in Coronary Artery Surgery (CASS). It is noteworthy that there is a steady decline in the operative risk for this growing population of patients requiring surgical revascularisation, and that there is no difference in operative outcomes between protected or unprotected LMS disease.
This study provides a ‘real-life’ experience of surgical revascularisation for LMS stenosis, which has been scarcely reported. An operative mortality of 2.7% compares well with higher mortality rates reported for PCI in some observational studies.8 Although randomised clinical trials2-4,9 and registry data10,11 reveal comparable procedural risks for both PCI and CABG, the rates of subsequent re-intervention remain high with PCI.12 Also, the complexity of the atherosclerotic lesion appears to have a prognostic impact on the outcome of PCI as the SYNTAX score has shown, which is not the case for CABG.3,13 The cohort of patients best suited for PCI was identified by Ghenim et al.14 to include older patients with high creatinine and EuroSCORE.
In the current era of myocardial revascularisation with low operative risk, the determination of clinical benefit should focus on long-term prognosis for competing revascularisation strategies. CABG for LMS disease is associated with good long-term survival comparable with non-LMS patients.
This study, like all retrospective studies, is constrained by inherent limitations of the study design. Angiographic details, such as the anatomical sites of LMS stenosis, were not available. Also data about postoperative myocardial infarction were not available for all the patients, however, a good number of patients had entries based on electrocardiographic changes, echocardiographic findings and enzyme (troponin and/or creatine kinase myocardial band [CKMB]) rise to enable a comparison between groups. The long-term follow-up data did not distinguish cardiac deaths from all-cause mortality, and did not capture late major adverse cardiac events like re-intervention, hence only late survival is reported.
The number of patients undergoing CABG for LMS stenosis is growing as the operative mortality is declining. Although LMS is associated with increased operative risk for CABG, long-term survival for protected and unprotected LMS disease is excellent following CABG.
Acknowledgement
We wish to acknowledge the contribution of Miss Catherine Malpas, the cardiothoracic database manager at Blackpool teaching hospital, for helping with data retrieval and obtaining follow-up survival data. This study was first presented at the 25th Annual meeting of The European Association of Cardiothoracic Surgeons held in Lisbon, Portugal from October 1st to 5th, 2011.
Conflict of interest
None declared.
Key messages
- Patients undergoing coronary artery bypass grafting (CABG) with left main stem (LMS) coronary artery stenosis are at higher operative risk than those without
- Operative mortality and morbidity for CABG for non-LMS and LMS disease is steadily improving
- Surgical revascularisation is as safe for protected LMS disease, as it is for unprotected LMS disease
- CABG for LMS disease yields excellent long-term survival comparable with non-LMS disease
References
- Rathore S, Grayson AD, Sastry S et al. Circumstances and mode of in-hospital death following 9,914 consecutive patients undergoing percutaneous coronary interventions in the northwest of England. J Invasive Cardiol 2008;20:386–90.
- Park SJ, Kim YH, Park DW et al. Randomized trial of stents versus bypass surgery for left main coronary artery disease. N Engl J Med 2011;364:1718–27. http://dx.doi.org/10.1056/NEJMoa1100452
- Serruys PW, Morice MC, Kappetein AP et al. Percutaneous coronary intervention versus coronary-artery bypass grafting for severe coronary artery disease. N Engl J Med 2009;360:961–72. http://dx.doi.org/10.1056/NEJMoa0804626
- Seung KB, Park DW, Kim YH et al. Stents versus coronary-artery bypass grafting for left main coronary artery disease. N Engl J Med 2008;358:1781–92. http://dx.doi.org/10.1056/NEJMoa0801441
- Onuma Y, Girasis C, Piazza N et al. Long-term clinical results following stenting of the left main stem: insights from RESEARCH (Rapamycin-Eluting Stent Evaluated at Rotterdam Cardiology Hospital) and T-SEARCH (Taxus-Stent Evaluated at Rotterdam Cardiology Hospital) Registries. JACC Cardiovasc Interv 2010;3:584–94. http://dx.doi.org/10.1016/j.jcin.2010.03.017
- Serruys P. SYNTAX at four years: death rates diverge but no change in advice. 2011. Available from: http://www.theheart.org/article/1293047.do [accessed 12 January 2012].
- Chaitman BR, Rogers WJ, Davis K et al. Operative risk factors in patients with left main coronary-artery disease. N Engl J Med 1980;303:953–7. http://dx.doi.org/10.1056/NEJM198010233031701
- Hertting K, Harle T, Krause K, Reimers J, Boczor S, Kuck KH. Stenting of unprotected left main stem stenosis: results from a German single-centre registry. Exp Clin Cardiol 2008;13:37–41.
- Park DW, Seung KB, Kim YH et al. Long-term safety and efficacy of stenting versus coronary artery bypass grafting for unprotected left main coronary artery disease: 5-year results from the MAIN-COMPARE (Revascularization for Unprotected Left Main Coronary Artery Stenosis: Comparison of Percutaneous Coronary Angioplasty Versus Surgical Revascularization) registry. J Am Coll Cardiol 2010;56:117–24. http://dx.doi.org/10.1016/j.jacc.2010.04.004
- Caggegi A, Capodanno D, Capranzano P et al. Comparison of one-year outcomes of percutaneous coronary intervention versus coronary artery bypass grafting in patients with unprotected left main coronary artery disease and acute coronary syndromes (from the CUSTOMIZE registry). Am J Cardiol 2011;108:355–9. http://dx.doi.org/10.1016/j.amjcard.2011.03.050
- Kang SH, Park KH, Choi DJ et al. Coronary artery bypass grafting versus drug-eluting stent implantation for left main coronary artery disease (from a two-center registry). Am J Cardiol 2010;105:343–51. http://dx.doi.org/10.1016/j.amjcard.2009.09.036
- Cohen DJ, Van Hout B, Serruys PW et al. Quality of life after PCI with drug-eluting stents or coronary-artery bypass surgery. N Engl J Med 2011;364:1016–26. http://dx.doi.org/10.1056/NEJMoa1001508
- Park DW, Kim YH, Yun SC et al. Complexity of atherosclerotic coronary artery disease and long-term outcomes in patients with unprotected left main disease treated with drug-eluting stents or coronary artery bypass grafting. J Am Coll Cardiol 2011;57:2152–9. http://dx.doi.org/10.1016/j.jacc.2011.01.033
- Ghenim R, Roncalli J, Tidjane AM et al. One-year follow-up of nonrandomized comparison between coronary artery bypass grafting surgery and drug-eluting stent for the treatment of unprotected left main coronary artery disease in elderly patients (aged >or=75 years). J Interv Cardiol 2009;22:520–6. http://dx.doi.org/10.1111/j.1540-8183.2009.00503.x
