Our objective was to compare the performance of computed tomography coronary angiography (CTCA) with exercise tolerance testing (ETT) in patients presenting with stable chest pain with low-to-intermediate predicted risk of coronary artery disease (CAD) as defined by the UK National Institute for Health and Care Excellence (NICE) clinical guideline 95. We investigated 85 patients with ETT and 102 patients with CTCA as first-line investigations after clinical assessment. Outcome measures assessed were diagnosis or exclusion of CAD, referral for second-line investigations, false-positive rate and cost of investigation to reach diagnosis for each modality.
CTCA was diagnostic in more patients than ETT (95.1% vs. 80.0%, p<0.05), had a lower false-positive rate (2.9% vs. 17.6%), led to fewer referrals for second-line investigations (4.9% vs. 21.2%, p<0.05) and resulted in overall comparable cost of investigation per patient (£183.44 vs. £165.16, p=0.49).
In conclusion, CTCA outperforms ETT as a first-line investigation in the investigation of patients presenting with stable chest pain with low-to-intermediate predicted risk of CAD as defined by NICE clinical guideline 95.
Introduction
For many years, the exercise tolerance test (ETT) has been the first-line investigation in patients presenting with stable chest pain. However, equivocal and false-positive results often lead to additional investigations. In recent years, computed tomography (CT) coronary angiography (CTCA) has been demonstrated to have excellent negative predictive value, making it a useful test to rule out obstructive coronary artery disease (CAD).1-3
In 2010, the UK National Institute for Health and Care Excellence (NICE) published clinical guideline 95: ‘Chest pain of recent onset’. This guideline advocates the use of a new risk estimation of CAD (CADScore); a calculation based on age, gender, nature of chest pain and cardiovascular risk factors using a modification of the Diamond Forrester criteria.4 The guideline recommends selecting the first-line investigation according to this calculated score: if CADScore 10–29%, CT calcium scoring ± CTCA is recommended; if CADScore 30–60%, functional imaging is recommended; if CADScore 61–90%, invasive coronary angiography (ICA) is recommended.5
Our experience is that the majority of patients presenting with stable chest pain are ultimately diagnosed with non-cardiac chest pain. A previous audit in our local area (from 2009 to 2010) of 401 consecutive patients presenting with stable chest pain, documented an overall incidence of 13.2% CAD requiring treatment (percutaneous coronary intervention [PCI], coronary artery bypass grafting [CABG] or medical therapy).6 The incidence in the low predicted risk subgroup (CADScore 10–29%) was 4.8%. In the intermediate predicted risk subgroup (CADScore 30–60%) the incidence was 6.4%.
In contrast with NICE clinical guideline 95, the current joint American College of Cardiology (ACC)/American Heart Association (AHA) guidelines7 recommend CTCA for the investigation of patients with stable chest pain and both low and intermediate predicted risk. In this study we compared the previous standard of care (ETT) with CTCA in patients with stable chest pain and low-to-intermediate predicted risk as determined by CADScore.
Methods
Patients
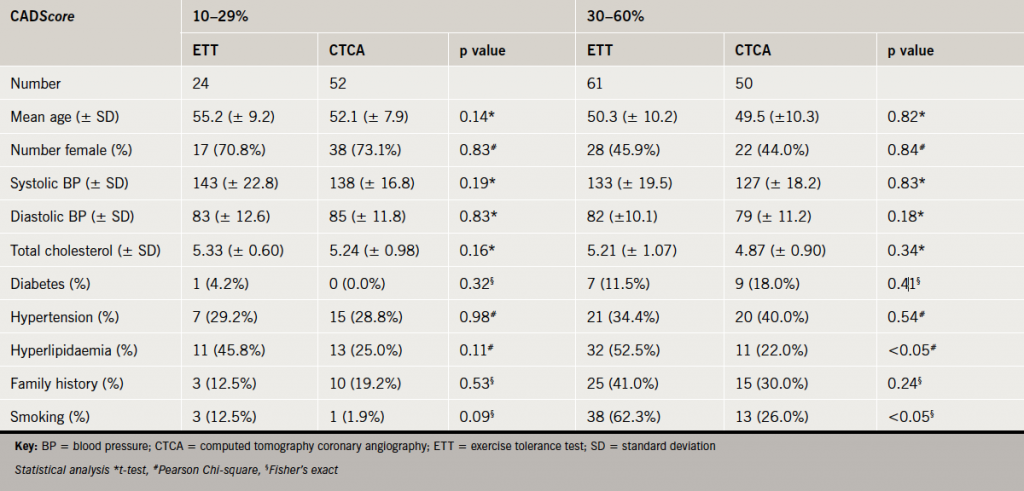
Two cohorts of consecutive patients presenting with stable chest pain were retrospectively compared. The first cohort consisted of patients referred for ETT as a first-line investigation over a six-month period, as per standard of care prior to introduction of CTCA in our hospital. The second cohort of consecutive patients consisted of patients referred for CTCA as a first-line investigation over a further six-month period, after the introduction of CTCA in our hospital. Each patient was retrospectively risk assessed according to NICE clinical guideline 95, and a CADScore was calculated. Only those with low-to-intermediate predicted risk (CADScore 10–60%) were included in this analysis: 85 patients from the first cohort (ETT) and 102 patients from the second cohort (CTCA). Baseline patient characteristics and statistical comparison of the two cohorts are summarised in table 1. Patients were followed until conclusion of investigations and final diagnosis was reached. Three patients in the ETT cohort did not complete their investigations and were lost to follow-up.
The exercise tolerance test
Bruce protocol was employed according to our hospital guidelines. The target heart rate (HR) was calculated as 85 × (220 – age). The test was terminated when the target HR was reached or the patient developed persistent chest pain and/or a shift in the ST segment of 1 mm in one or more leads.
Second-line investigations
Patients with a positive ETT were referred for ICA. Patients in whom target HR was not achieved, or in whom the test was considered equivocal, were further investigated with a functional test (stress echocardiography or nuclear myocardial perfusion stress test) and/or ICA as per standard clinical practice. Significant CAD found during ICA was defined as ≥70% diameter stenosis of at least one major epicardial coronary artery segment or ≥50% diameter stenosis in the left main coronary artery.
CTCA
Patients were either previously orally beta-blocked by the referring clinician and/or were intravenously beta-blocked with intravenous metoprolol (5–30 mg) aiming to achieve a heart rate of <60 bpm. All patients received two 400 µg doses of sublingual glycerol trinitrate. For the contrast part of the scan, 100 ml of loversol (Optiray 350 mg/ml, Covidien UK, Hampshire, UK), at a flow rate of 5 ml/s followed by 100 ml of saline solution, were injected into an antecubital vein via an 18-gauge peripheral venous catheter. Bolus tracking was used with a region of interest placed into the ascending aorta.
All CTCA were performed with a 64-slice LightSpeed VCT XTe GE scanner (GE Healthcare) and prospective gating. Using the commercially available protocol (SnapShot Pulse, GE Healthcare) and the following scanning parameters: slice acquisition 64 × 0.625 mm, selected field of view (SFOV) Cardiac, Z-axis detector coverage 40 mm, gantry rotation time of 350 ms. Patients’ size was visually judged for adapted tube voltage; 100 kV was used for small patients, 120 kV for average size patients, and two very large patients required 140 kV. Similarly, effective tube-current ranged between 500 mA and 650 mA based on patient’s size judged visually. A scout scan was followed by a prospectively gated calcium score scan. If the calcium score was >400, the CTCA was not performed and the patient was referred for an alternative investigation. Otherwise, the CTCA was performed from below the tracheal bifurcation to the diaphragm to just below the inferior border of the heart, with displayed field of view (DFOV) of 25 cm. By choosing the smallest possible window and limiting the acquisition to the 75% end-diastolic phase of the RR-cycle, we lowered the dose as much as possible. The effective radiation dose of CTCA was calculated as the product of the dose-length product (DLP) times a conversion factor coefficient for the chest (κ=0.014 mSv/mGy·cm). CTCA images were reconstructed with slice thickness of 0.625 mm, using a medium-soft tissue convolution kernel (standard). All images were transferred to an external workstation (ADW 4.5, GE Healthcare) for analysis.
Second-line investigations
Patients in whom CTCA demonstrated severe coronary artery stenoses (defined as >70% luminal narrowing) were referred for ICA. Patients in whom CTCA demonstrated moderate coronary artery stenoses (defined as 50–70% luminal narrowing) were referred for functional testing (stress echocardiography or nuclear myocardial perfusion stress test) and/or ICA. Functional imaging test was considered positive if there was significant ischaemia (≥10% myocardial ischaemia by nuclear perfusion imaging or ≥3 segments ischaemia on stress echocardiography). Significant CAD found during ICA was defined as ≥70% diameter stenosis of at least one major epicardial artery segment or ≥50% diameter stenosis in the left main coronary artery.
Statistical methods
Statistical analysis was performed with SPSS version 18.0 for Windows.
Cost analysis
The total cost of investigation to reach diagnosis was calculated for each patient based on the pricing scheme recommended in the NICE ‘Chest Pain of Recent Onset’ costing report 2011 (£75 for ETT and £173 for CTCA).8 If the first-line test was positive (i.e. >70% luminal narrowing on CTCA or positive ETT) and subsequent ICA confirmed obstructive CAD, then the cost of ICA was not included in the cost of investigation.
Results
Results were analysed by cohort (ETT or CTCA). Within each cohort, analysis was also performed in two subgroups defined by predicted risk: low predicted risk (CADScore 10–29%) and intermediate predicted risk (CADScore 30–60%).
ETT cohort
A total of 85 patients were referred for ETT as first-line investigation. ETT was reported as negative in 72.9%, positive in 7.1% and equivocal in 20.0% of patients. There were 11.8% of patients referred for second-line functional testing and 5.9% were referred for second-line ICA. Eventually, 4.7% of patients were confirmed to have obstructive CAD requiring treatment (PCI, CABG or medical therapy).
In the low predicted risk subgroup (CADScore 10–29%), ETT was reported as negative in 79.2%, positive in 8.3% and equivocal in 12.5% of patients. There were 8.3% of patients referred for second-line functional testing and 0% were referred for second-line ICA. Eventually, 4.2% of patients were confirmed to have obstructive CAD requiring treatment (PCI, CABG or medical therapy).
In the intermediate predicted risk subgroup (CADScore 30–60%), ETT was reported as negative in 70.5%, positive in 6.6% and equivocal in 23.0% of patients. There were 13.1% of patients referred for second-line functional testing and 8.2% were referred for second-line ICA. Eventually, 4.9% of patients were confirmed to have obstructive CAD requiring treatment (PCI, CABG or medical therapy).
CTCA cohort
A total of 102 patients were referred for calcium scoring ± CTCA as first-line investigation. The scan was performed without complication in all patients. Calcium scoring was performed in all but four patients, who were young, to minimise radiation dose. There were 2.9% of patients with a calcium score >400, who did not proceed to the contrast phase and were referred for alternative investigations (functional testing or ICA). Because of data from the Coronary Artery Evaluation Using 64-Row Multidetector Computed Tomography Angiography (CORE64) trial6 and Coronary CT Angiography Evaluation for Clinical Outcomes (CONFIRM) registry,7 which documented the presence of obstructive CAD in patients with zero calcium score, we elected to perform the contrast phase of the scan in all patients. Using the heart rate control measures described above, we were able to perform prospective gated studies in 97.8% of patients. Overall, this resulted in mean radiation dose of 3.19 ± 1.45 mSv per patient.
Calcium score
Overall, 70.6% of patients had zero calcium score. By subgroup, 73.1% of patients with low predicted risk (CADScore 10–29%) and 68.0% with intermediate predicted risk (CADScore 30–60%) had zero calcium score. Overall, 2.0% of patients had a calcium score >400 (0% in those with low predicted risk and 4.0% of those with intermediate predicted risk). A further 22.5% of patients had calcium score 1–400 (21.2% of those with low predicted risk and 24.0% of those with intermediate predicted risk).
Overall, the contrast phase of the scan demonstrated unobstructed coronary arteries in 92.1%, moderate stenoses in 1.0% and severe stenoses in 4.9% of patients (2.0% of patients did not proceed to the contrast phase of the scan because their calcium score was >400). There were 4.9% of patients referred for second-line functional testing and 0% were referred for second-line ICA. Eventually, 2.9% of patients were confirmed to have obstructive CAD requiring treatment (PCI or CABG).
In the low predicted risk subgroup (CADScore 10–29%), CTCA demonstrated unobstructed coronary arteries in 96.2%, moderate stenoses in 0% and severe stenoses in 3.8% of patients. There were 0% of patients referred for second-line functional testing and 0% were referred for second-line ICA. Eventually, 3.8% of patients were confirmed to have obstructive CAD requiring treatment (PCI or CABG).
In the intermediate predicted risk subgroup (CADScore 30–60%), CTCA demonstrated unobstructed coronary arteries in 88.0%, moderate stenoses in 2.0% and severe stenoses in 6.0% of patients. There were 4.0% of patients who did not have the contrast phase performed because their calcium score was >400 and were referred for alternative investigations (functional testing or ICA). There were 10.0% of patients referred for second-line functional testing and 0% were referred for second-line ICA. Eventually, 4.0% of patients were confirmed to have obstructive CAD requiring treatment (PCI or CABG).
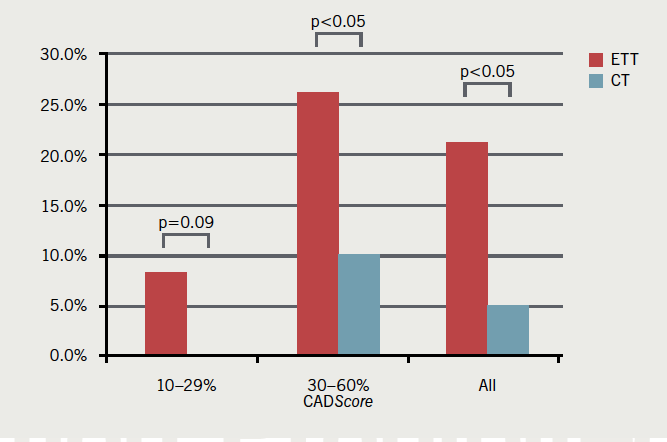
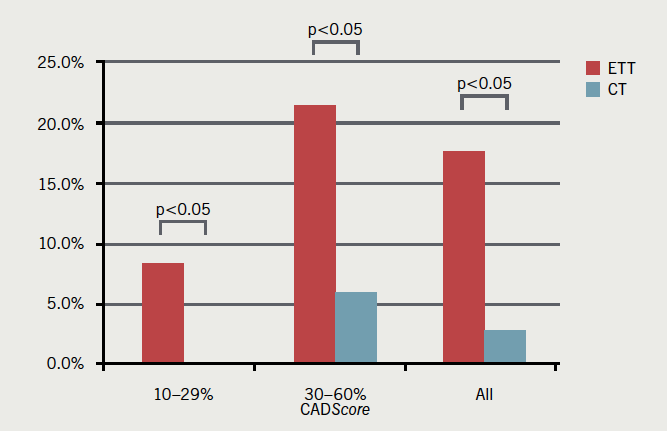
CTCA vs. ETT
As a first-line investigation, CTCA was diagnostic in more patients than ETT (95.1% vs. 80.0%, p<0.05). False-positive rates were calculated after invasive angiography. CTCA had a lower false-positive rate (2.9% vs. 17.6%). CTCA resulted in fewer referrals than ETT for second-line investigations (4.9% vs. 21.2%, p<0.05). These results are summarised in table 2 and figures 1–3.

In the low predicted risk subgroup (CADScore 10–29%), CTCA was diagnostic in more patients than ETT (100% vs. 87.5%, p<0.05) and had a lower false-positive rate (0% vs. 8.3%). CTCA resulted in fewer referrals than ETT for second-line investigations (0% vs. 8.3%, p=0.09).
In the intermediate predicted risk subgroup (CADScore 30–60%), CTCA was diagnostic in more patients than ETT (90.0% vs. 77.0%, p=0.07) and had a lower false-positive rate (6.0% vs. 21.3%). CTCA resulted in fewer referrals than ETT for second-line investigations (10.0% vs. 26.2%, p<0.05).
Cost analysis
Despite the higher cost of CTCA compared with ETT, overall mean cost per patient was not significantly higher in the CTCA cohort (£183.44 vs. £165.16, p=0.49). In the low predicted risk subgroup (CADScore 10–29%) mean cost per patient was 86.6% higher (£173.00 vs. £92.75, p<0.05), but In the intermediate predicted risk subgroup (CADScore 30–60%), mean cost per patient was only 0.3% higher (£193.66 vs. £194.30, p=0.98). These results are summarised in figure 4.

Study limitations
One limitation of this study is the comparison of two different cohorts of patients. However, statistical comparison of the two cohorts confirms very similar age, gender divide and burden of cardiovascular risk factors (table 1). CADScores were calculated retrospectively using clinical information gathered at the time of first presentation and so were potentially subject to error with regards to description of symptoms. However, all other elements of the CADScore were obtained from objective records (e.g. measured blood pressure, fasting glucose and serum cholesterol levels). Another potential limitation of this study is that not all patients with negative CTCA underwent ICA, which is considered the gold-standard test to rule out CAD. However, Maffei et al.9 demonstrated CTCA to be superior to ETT when compared with ICA in a similar low-to-intermediate predicted risk cohort (all patients underwent all three tests). The sensitivity, specificity, positive and negative predictive values for CTCA compared with ICA were, respectively, 100%, 98.7%, 92.9% and 100% compared with 46.2%, 16.6%, 8.7% and 64.1% for ETT. The prevalence of significant CAD (defined as >50% stenoses) in that study was 14.7%, which is a little higher than in our data. Similarly, patients in our study with negative functional imaging tests did not undergo further investigation with ICA. Although there is a potential for false-negative results, this represents standard clinical practice across the UK.
Discussion
In the CT cohort we performed CTCA on all patients, including those with zero calcium score. Published data from the CORE64 trial10 and the CONFIRM registry11 demonstrated the presence of CAD in patients with zero calcium score. This is particularly true for patients under 40 years of age in whom soft plaque coronary atheroma has not yet developed calcifications. The literature on calcium scoring has mostly been validated in asymptomatic populations and its application to symptomatic patients (albeit with low likelihood of CAD) remains under debate.12 With good heart rate control and optimisation of scanning protocols, our results show that mean radiation dose from CTCA can be kept very low.
Most patients presenting with stable chest pain with low-to-intermediate predicted risk do not have obstructive CAD after investigation. CTCA has been shown to be an excellent rule out test for CAD in patients with normal coronary arteries. The current NICE guideline only recommends calcium scoring ± CTCA in patients with low predicted risk of CAD (CADScore 10–29%). These results suggest that CTCA is also superior to ETT in patients with intermediate predicted risk (CADScore 30–60%). In patients with low-to-intermediate predicted risk, CTCA was diagnostic in more patients and led to fewer second-line investigations compared with ETT. As a result, the mean cost per patient was comparable, despite the higher upfront cost of CTCA compared with ETT. Furthermore, had we not proceeded to the contrast phase of the scan in patients with zero calcium score, the cost could have been lower.
A multi-centre clinical trial comparing ETT with CTCA in patients with stable chest pain and a low-to-intermediate risk of CAD (CRESCENT) is under way in the Netherlands and will report in 2016.13 Several North American multi-centre trials (PROSPECT,14 RESCUE15 and PROMISE16) are under way, comparing standard care ± functional testing versus CTCA in patients with stable chest pain and low-to-intermediate cardiovascular risk, and will report over the next few years. Furthermore, the use of CTCA in the emergency room to rule out CAD in patients presenting with possible acute coronary syndromes has already been shown to reduce length of stay, reducing overall cost, compared with standard of care and single-photon emission computed tomography (SPECT) in three clinical trials from the USA.17-19 Ultimately, the goal is to reduce the number of patients with normal coronary arteries having invasive coronary angiography, which is reported at up to 39% at present.20
Conclusion
These results support our hypothesis that CTCA is a clinically useful, safe and cost-efficient diagnostic test in patients with both low and intermediate predicted risk of CAD. Based on these results, we support NICE recommendations that patients with low predicted risk (CADScore 10–29%) would be most effectively investigated with cardiac CT as a first-line test. Furthermore, as the incidence of CAD in the intermediate risk patients is low, we suggest that CTCA would also be effective in patients with intermediate predicted risk (CADScore 30–60%)
Conflict of interest
None declared.
Key messages
- NICE guidance recommends risk assessment to direct choice of investigation in patients with stable chest pain
- Computed tomography coronary angiography (CTCA) has excellent negative predictive value in both low and intermediate risk patients
- CTCA leads to fewer second-line investigations than exercise tolerance testing (ETT), offsetting its higher upfront cost
- Several randomised-controlled trials comparing CTCA with functional imaging tests are currently recruiting
References
- Budoff MJ, Dowe D, Jollis JG et al. Diagnostic performance of 64-multidetector row coronary computed tomographic angiography for the evaluation of coronary artery stenoses in individuals without known coronary artery disease. Results from the prospective multicentre ACCURACY trial. J Am Coll Cardiol 2008;52:1724–32. http://dx.doi.org/10.1016/j.jacc.2008.07.031
- Meijboom WB, Meijs MF, Schuijf JD et al. Diagnostic accuracy of 64 slice computed tomography coronary angiography: a prospective multicentre multivendor study. J Am Coll Cardiol 2008;52:2135–44. http://dx.doi.org/10.1016/j.jacc.2008.08.058
- Min JK, Dunning A, Lin FY et al. CONFIRM Investigators. Age- and sex-related differences in all-cause mortality risk based on coronary computed tomography angiography findings results from the International Multicenter CONFIRM (Coronary CT Angiography Evaluation for Clinical Outcomes: An International Multicenter Registry) of 23,854 patients without known coronary artery disease. J Am Coll Cardiol 2011;58:849–60. http://dx.doi.org/10.1016/j.jacc.2011.02.074
- Pryor DB, Shaw L, McCants CB et al. Value of the history and physical in identifying patients at increased risk for coronary artery disease. Ann Intern Med 1993;118:81–90. http://dx.doi.org/10.7326/0003-4819-118-2-199301150-00001
- National Institute for Health and Clinical Excellence. Chest pain of recent onset – clinical guideline 95. London: NICE, 2010. Available from: http://www.nice.org.uk/CG95
- Rogers T, Dowd D, Yap HL, Claridge S, Alfakih K, Byrne J. Strict application of NICE Clinical Guideline 95 ‘chest pain of recent onset’ leads to over 90% increase in cost of investigation. Int J Cardiol 2012;published online. http://dx.doi.org/10.1016/j.ijcard.2012.09.180
- Taylor AJ, Cerqueira M, Hodgson JM et al. ACCF/SCCT/ACR/AHA/ASE/ASNC/NASCI/SCAI/SCMR appropriate use criteria for cardiac computed tomography. Circulation 2010;122:e525–e555. http://dx.doi.org/10.1016/j.jacc.2010.07.005
- National Institute for Health and Clinical Excellence. Chest pain of recent onset – costing report 2011. London: NICE, 2011. Available from: http://www.nice.org.uk/nicemedia/live/12947/55738/55738.pdf
- Maffei E, Seitun S, Martini C et al. CT coronary angiography and exercise ECG in a population with chest pain and a low to intermediate pre-test likelihood of coronary artery disease. Heart 2010;96:1973–9. http://dx.doi.org/10.1136/hrt.2009.191361
- Gottlieb I, Miller JM, Arbab-Zadeh A et al. The absence of coronary calcification does not exclude obstructive coronary artery disease or the need for revascularization in patients referred for conventional coronary angiography (CORE64). J Am Coll Cardiol 2010;55:627–34. http://dx.doi.org/10.1016/j.jacc.2009.07.072
- Villines TC, Hulten EA, Shaw LJ et al. CONFIRM Registry Investigators. Prevalence and severity of coronary artery disease and adverse events among symptomatic patients with coronary artery calcification scores of zero undergoing coronary computed tomography angiography: results from the CONFIRM (Coronary CT Angiography Evaluation for Clinical Outcomes: An International Multicenter) registry. J Am Coll Cardiol 2011;58:2533–40. http://dx.doi.org/10.1016/j.jacc.2011.10.851
- Miller R. Zero means nothing: ‘gatekeeper’ role of calcium scoring questioned. Available from: http://www.theheart.org/article/1046039.do [accessed 5 July 2013].
- Clinicaltrials.gov. Computed tomography versus exercise testing in suspected coronary artery disease (CRESCENT). Available from: http://clinicaltrials.gov/ct2/show/NCT01393028 [accessed 25 February 2013].
- Clinicaltrials.gov. Study comparing CT scan and stress test in diagnosing coronary artery disease in patients hospitalized for chest pain (PROSPECT). Available from: http://clinicaltrials.gov/ct2/show/NCT00705458 [accessed 25 February 2013].
- Clinicaltrials.gov. Randomized evaluation of patients with stable angina comparing diagnostic examinations (RESCUE). Available from: http://clinicaltrials.gov/ct2/show/NCT01262625 [accessed 25 February 2013].
- Clinicaltrials.gov. Prospective multicenter imaging study for evaluation of chest pain (PROMISE). Available from: http://clinicaltrials.gov/ct2/show/NCT01174550 [accessed 25 February 2013].
- Litt HI, Gatsonis C, Snyder B et al. CT angiography for safe discharge of patients with possible acute coronary syndromes. N Engl J Med 2012;366:1393–403. http://dx.doi.org/10.1056/NEJMoa1201163
- Goldstein JA, Chinnaiyan KM, Abidov A et al. The CT-STAT (Coronary Computed Tomographic Angiography for Systematic Triage of Acute Chest Pain Patients to Treatment) trial. J Am Coll Cardiol 2011;58:1414–22. http://dx.doi.org/10.1016/j.jacc.2011.03.068
- Hoffmann U, Truong QA, Schoenfeld DA et al. Coronary CT angiography versus standard of evaluation in acute chest pain. N Engl J Med 2012;367:299–308. http://dx.doi.org/10.1056/NEJMoa1201161
- Patel MR, Peterson ED, Dai D et al. Low diagnostic yield of elective coronary angiography. N Engl J Med 2010;362:886–95. http://dx.doi.org/10.1056/NEJMoa0907272