Chronic refractory angina results in significant NHS costs due to chronic high use of resources. This audit evaluated the clinical effectiveness of a cognitive-behavioural (CBT) programme in reducing angina symptoms after maximal medical and surgical intervention. The primary outcome was self-reported angina. Additional questionnaire data comprised perceived quality of life/disability, angina misconceptions, self-efficacy and mood. Data from the electronic patient administration system was used to compare use of cardiology hospital resources in the two years before and two years after attendance. Patients completing questionnaires reported significant improvements in all areas post-group and at two months. Resource use was lower in the two years post-programme than the two years prior. A CBT-based approach to symptom management could offer additional clinical benefits in the cardiac rehabilitation menu.
Introduction
Chronic refractory angina is defined as coronary insufficiency in the presence of coronary artery disease with clinically established reversible myocardial ischaemia that cannot be controlled by a combination of medical therapy, angioplasty and coronary bypass surgery (CABG).1 Symptom duration should exceed three months. It carries a small increased risk of mortality,2 a significant risk of morbidity3 and accounts for more than 1% of the UK’s total health service budget.4
Triggers for angina include behavioural factors, such as activity and stress. Common misconceptions (e.g. that angina may precipitate myocardial infarction) may cause patients to avoid these triggers, which could lead to de-conditioning, worsening angina and low mood.5 Of patients in cardiac rehabilitation (CR), 27% have angina as a comorbidity,6 and yet, traditional programmes have not generally measured their impact on symptoms. Small UK studies have suggested that cognitive-behavioural therapy (CBT)-based CR may benefit symptoms, quality of life7-9 and use of hospital resources.10 This audit looks at the outcomes of a programme, evolved from the angina management programme (AMP),7 for refractory angina patients considered by their cardiologists to be on optimal treatment and unsuitable for further intervention at that time (e.g. intervention not technically feasible or carrying unjustifiable risk).
Methods
Patients
Participants were referred between 2006 and 2013 by cardiologists and, occasionally, by GPs.
Recruitment procedure
Initial medical assessment:
- Acknowledged the benefits and limits of current medical/surgical therapy and introduced the benefits of a self-management approach.
- Assessed behavioural risk factors for coronary heart disease (CHD).
- Explored possible mechanisms for non-ischaemic chest pain, where this co-existed with angina.
- Risk stratified for exercise.
Pre-group therapist assessment explored:
- Current strategies for coping with angina and readiness to change.
- Valued areas of life, where change would impact on quality of life.
- Factors requiring programme modification (e.g. physical/cognitive limitations).
- Barriers/aids to change (e.g. low assertiveness, family support).
- Whether low mood was associated with health, i.e. amenable to change through this intervention.
Individual CBT formulations underpinned treatment. By linking thoughts, behaviours and emotional reactions to symptoms, areas where change could reduce symptoms are highlighted. Background and social issues were considered in a case formulation.11
Exclusion criteria
Unable to follow programme due to limitations in language or cognition, immediate life-threatening comorbidity or active psychosis, angina due to untreated valvular disease or hypertrophic cardiomyopathy. Previous attendance at CR was not an exclusion criterion.
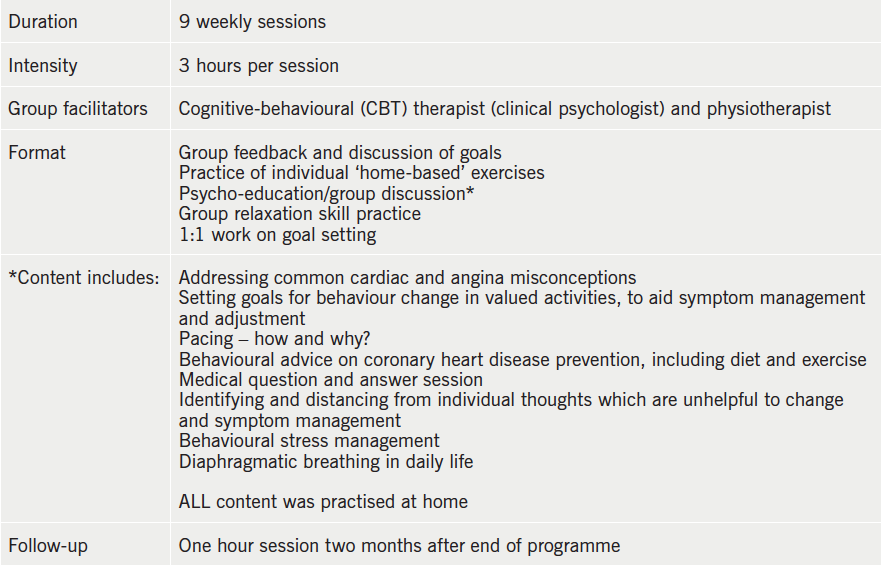
AMP intervention
The AMP intervention is shown in table 1.
Measures
Self-report questionnaires were sent/given out in advance, to be completed independently by the patient and returned to staff at first assessment, final session and at two-month follow-up. In order to minimise missing data, an assistant looked through questionnaires as they came in and, if items were missed, he/she explained the item to the patient at their next attendance.
- Angina symptoms diary – self-reported over a week: number and duration of episodes, severity rated on a scale from 0 to 100. Number of times glyceryl trinitrate (GTN) spray used.
- Hospital Anxiety and Depression Scale (HADS)12 is widely used and well validated. It can be used as a total measure of general distress or as separate anxiety and depression subscales. The latter range from 0–21, with 8 or more on each subscale indicating potential clinical significance.
- The Roland Morris Disability Questionnaire13 assesses impact of disability upon everyday life. Higher scores indicate greater interference, with a maximum score of 24. It has good reliability and external validity.14 This was devised for back pain, but modified, by us, for angina.
- The Pain Self-Efficacy Questionnaire15 assesses confidence in performing activities while in pain. It has 10 items with a maximum score of 60. Internal consistency and re-test reliability are high. The word ‘pain’ was changed, by us, to ‘angina’.
- The York Angina Misconceptions Questionnaire16 assesses common mistaken beliefs about angina. Reliability and validity are good. Higher scores indicate more misconceptions. The original four-point scale was modified to scores of one for ‘yes’ and zero for ‘no’, with a total of 14.
- Use of cardiology resources – for all patients starting a programme, data were collated (retrospectively and by a trained administrator) from the electronic patient administration system, for the two years before they started the programme and two years from the last session (excluding time on the programme).
Three categories of data were collected:
- Number of inpatient appointments – including angioplasty, CABG and other infrequent cardiac surgery.
- New outpatient appointments – including first visit to consultant, rapid access chest pain clinic, electrocardiography, pacemaker clinic, exercise treadmill test and transthoracic echo.
- Cardiology outpatient review – all visits (except heart failure service).
Additional post hoc analyses examined whether reduction in angina frequency differed in those with clinically low mood compared with normal mood, and, also, whether demographic and clinical variables were associated with dropout.
Statistical analysis
Statistical analysis used SPSS version 16.0. Self-report variables were not normally distributed and non-parametric statistics were used for these. Wilcoxon signed-rank tests compared before and after measures. Cohen’s d quantified effect size. McNemar’s test compared percentage reaching clinical anxiety and depression before and after. Friedman’s test compared before, after and two-month follow-up. Chi-square tests or t-tests compared dropouts and completers on clinical and demographic data. Cardiology resource use data were normally distributed and were compared using paired t-tests.
Results
There were 148 patients referred and considered suitable for the AMP: 13 did not start due to illness, holiday or change of mind, i.e. 135 started. There were 23 groups run, with an average of 5.9 patients per group.
Numbers completing at least one questionnaire were: 124 pre-group, 87 post-group and 69 at follow-up. Due to missing data items, some questionnaire numbers in table 2 are lower for each time point. Of 135 patients beginning the AMP, 105 attended six sessions or more and were deemed to have completed the intervention (77%). The data from ‘dropouts’ are included in this analysis.
Mean age of participants was 70.2 (46–92) years with 73.4% male. Overall, 81% had at least one comorbidity (excluding the cardiac risk factors diabetes and hypertension), such as obesity, arthritis, other chronic pain, Parkinson’s disease, asthma, chronic obstructive airways disease, alcohol dependence, cancer, irritable bowel syndrome, renal problems and cardiomyopathy. Previous myocardial infarction was documented in 41.6%, coronary artery bypass surgery in 23%, percutaneous coronary intervention in 56% and previous cerebrovascular accident or transient ischaemic attack in 11%.
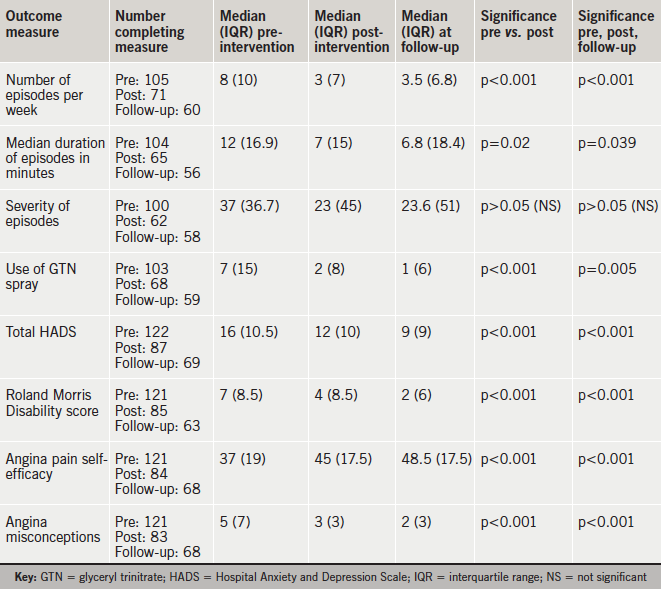
Significant improvement was found pre- to post-programme on all variables except severity of angina. Effect sizes were generally moderate (number of episodes 0.54, GTN 0.45, HADS 0.51, self-efficacy –0.46) though larger for misconceptions (0.66) and smaller for duration of episodes (0.23) and disability (0.33). Table 2 gives median variable values, interquartile range and significance of change, comparing before and after the AMP and follow-up.
Percentage of patients reaching clinical significance on the HADS depression subscale reduced from 45.1% before to 26.8% after the programme, which was significant (p=0.003). A reduction in anxiety from 58.5% to 42.7% was also significant (p=0.002).
Of participants, 69 attended follow-up groups and completed follow-up measures. Those who did had maintained benefits.
Cardiology resources use for all 135 patients starting the programme (including dropouts), reduced significantly. Mean admissions decreased from 1.6 prior to 0.5 post, t(149)=9.3, p<0.001. Mean new outpatient appointments decreased from 0.5 to 0.3, t(149)=2.3, p=0.02; and mean return outpatient appointments from 1.9 to 1.3, t(149)=3.8, p<0.001.
Post hoc analyses showed no difference in the decrease in angina frequency between people who initially had clinical levels of either anxiety or depression compared with people who reported no mood problems, t(59)=0.52, p=0.61. Dropout rate (attending five sessions or fewer) was 23%. This was not related to gender, χ2(df1, n=135)=0.13, p=0.72; number of comorbidities, t(116)=0.67, p=0.51; or initial total scores on HADS, t(112)=0.59, p=0.56; self-efficacy, t(27.8)=–1.1, p=0.3; or angina episodes, t(95)=1.88, p=0.06. Dropouts scored higher on initial misconceptions than completers, t(109)=3.3, p=0.001.
Discussion
The AMP was effective in its primary aim of reducing reported angina frequency and duration, though not angina severity. GTN use was reduced. There were significant improvements in perceived quality of life/disability, angina misconceptions, self-efficacy and mood, including clinical levels of anxiety and depression. These remained at two-month follow-up. Use of cardiology resources was significantly reduced two years post-programme.
What accounts for the reduction in angina? A randomised-controlled trial (RCT)17 of conventional exercise-based CR for angina patients, found improvements in functional ability, health anxiety and perceived angina threat but no difference in angina frequency and severity, suggesting that exercise alone is not sufficient to reduce symptom frequency. Our finding of reduced angina frequency is consistent with Lewin et al.8 The finding of no change in severity may suggest that the benefits of the AMP are not through altered pain perception. A recent meta-analysis of psycho-educational and CBT approaches for angina, found clear evidence of reduced symptom frequency.18 We would argue that improvements are attributable to the behavioural and home-focused nature of this programme.
This audit included patients who had other chronic illnesses or psychiatric history, who might be excluded from clinical trials. Improvements in self-reported symptoms, mental health and NHS resource use are important outcomes for patients with a long-term condition with multi-morbidities.19,20
It is a significant concern that the groups have not been running at full capacity. The dropout rate of 23% is comparable with recent UK studies,21 but, over the seven-year period studied, the referral rate has remained low and is falling. We are, therefore, considering how to integrate the symptom management approach into our general CR programmes, and use it with patients with other symptoms, such as fatigue and breathlessness.
This is a clinical audit and patients who completed the post-group and follow-up questionnaires are likely to be those who had made most gains. Assessment could not be ‘blind’ as the questionnaires were returned to programme staff. The reduction in use of cardiology resources needs to be interpreted with caution, as patients are most likely to be referred to CR at a time of high attendance in cardiology, and the latter might reduce naturally over time. The strength of a clinical audit lies in it being representative of the kinds of patients with chronic cardiac conditions and multi-morbidities who are being referred to CR in the UK.
Acknowledgement
The authors would like to thank the CTR data team Lothian.
Conflict of interest
None declared.
Funding
No external financial support was sought for this study.
Editors’ note
See also the article by Patel et al. on pages 57–60 and the editorial by Wright and de Silva on pages 45–6 of this issue.
Key messages
- The management of chronic refractory symptoms in long-term cardiac conditions is an important issue for the National Health Service (NHS)
- An approach that integrates cognitive-behavioural strategies into cardiac rehabilitation is acceptable and effective for patients with refractory angina, many of whom have multiple comorbidities
- Clinical trials are merited to evaluate rehabilitation approaches for this population
References
1. Mannheimer C, Camici P, Chester MR et al. The problem of chronic refractory angina: report from the ESC Joint Study Group on the treatment of refractory angina. Eur Heart J 2002;23:355–70. http://dx.doi.org/10.1053/euhj.2001.2706
2. Henry TD, Satran D, Hodges JS et al. Long-term survival in patients with refractory angina. Eur Heart J 2013;34:2683–8. http://dx.doi.org/10.1093/eurheartj/eht165
3. Moore RK, Groves D, Bateson S et al. Health related quality of life of patients with refractory angina before and one year after enrolment onto a refractory angina programme. Eur J Pain 2005;9:305–10. http://dx.doi.org/10.1016/j.ejpain.2004.07.013
4. Stewart S, Murphy NF, Walker A et al. The current cost of angina pectoris to the National Health Service in the UK. Heart 2003;89:848–53. http://dx.doi.org/10.1136/heart.89.8.848
5. Gravely-Witte S, De Gucht V, Heiser W et al. The impact of angina and cardiac history on health-related quality of life and depression in coronary heart disease patients. Chronic Illn 2007;3:66–76. http://dx.doi.org/10.1177/1742395307079192
6. British Heart Foundation. The National Audit of Cardiac Rehabilitation annual statistical report 2015. London: British Heart Foundation, 2015. Available from: http://www.cardiacrehabilitation.org.uk
7. Lewin B, Cay EL, Todd I. The angina management programme: a rehabilitation treatment. Br J Cardiol 1995;2:219–26.
8. Lewin RJP, Furze G, Griffith K et al. A randomized controlled trial of a self-management plan for patients with newly diagnosed angina. Br J Gen Pract 2002;52:194–201. Available from: http://bjgp.org/content/52/476/194.long
9. Zetta S, Smith K, Jones M et al. Evaluating the angina plan in patients admitted to hospital with angina: a randomized controlled trial. Cardiovasc Ther 2011;29:112–24. http://dx.doi.org/10.1111/j.1755-5922.2009.00109.x
10. Moore RK, Groves DG, Bridson JD et al. A brief cognitive-behavioural intervention reduces hospital admissions in refractory angina patients. J Pain Symptom Manage 2007;33:310–16. http://dx.doi.org/10.1016/j.jpainsymman.2006.10.009
11. Halford J, Brown T. Cognitive behavioural therapy as an adjunctive treatment in chronic physical illness. Adv Psychiatr Treat 2009;15:306–17. http://dx.doi.org/10.1192/apt.bp.107.003731
12. Zigmond AS, Snaith RP. The Hospital Anxiety and Depression Scale. Acta Psychiatr Scand 1983;67:361–70. http://dx.doi.org/10.1111/j.1600-0447.1983.tb09716.x
13. Roland MO, Morris RW. A study of the natural history of back pain. Part 1: Development of a reliable and sensitive measure of disability in low back pain. Spine 1983;8:141–4. http://dx.doi.org/10.1097/00007632-198303000-00004
14. Davies C, Nitz A. Psychometric properties of the Roland-Morris Disability Questionnaire compared to the Oswestry Disability Index a systematic review. Phys Ther Rev 2009;14:399–408. http://dx.doi.org/10.1179/108331909X12540993898134
15. Nicholas MK. The pain self-efficacy questionnaire: taking pain into account. Eur J Pain 2007;11:153–63. http://dx.doi.org/10.1016/j.ejpain.2005.12.008
16. Furze G, Bull P, Lewin RJ, Thompson DR. The York Angina Misconceptions Questionnaire. J Health Psychol 2003;8:307–15. http://dx.doi.org/10.1177/13591053030083002
17. Ashbury EA, Webb CM, Probert H et al. Cardiac rehabilitation to improve physical functioning in refractory angina: a pilot study. Cardiology 2012;122:170–7. http://dx.doi.org/10.1159/000339224
18. McGillion M, O’Keefe-McCarthy S, Carroll SL et al. Impact of self-management interventions on stable angina symptoms and health-related quality of life: a meta-analysis. BMC Cardiovasc Disord 2014;14:14. http://dx.doi.org/10.1186/1471-2261-14-14
19. British Association for Cardiovascular Prevention and Rehabilitation. The BACPR standards and core components for cardiovascular disease prevention and rehabilitation 2012. London: BACPR, 2012. Available from: http://www.bacpr.com/resources/46c_bacpr_standards_and_core_components_2012.pdf
20. Naylar C, Parsonage M, McDaid D, Knapp M, Fossey M, Galea A. Long-term conditions and mental health – the cost of co-morbidities. London: The Kings Fund and Centre for Mental Health, 2012. Available from: http://www.kingsfund.org.uk/sites/files/kf/field/field_publication_file/long-term-conditions-mental-health-cost-comorbidities-naylor-feb12.pdf
21. Sharp J, Freeman C. Patterns and predictors of uptake and adherence to cardiac rehabilitation. J Cardiopulm Rehabil Prev 2009;29:241–7. http://dx.doi.org/10.1097/HCR.0b013e3181adcf0f
