This year’s European Society of Cardiology (ESC) Congress took place in Rome, Italy, from 27th–31st August 2016 and attracted over 33,000 delegates from across the globe, including His Holiness Pope Francis. Here we present some of the highlights from this key event in the cardiology calendar.
More news from ESC available online
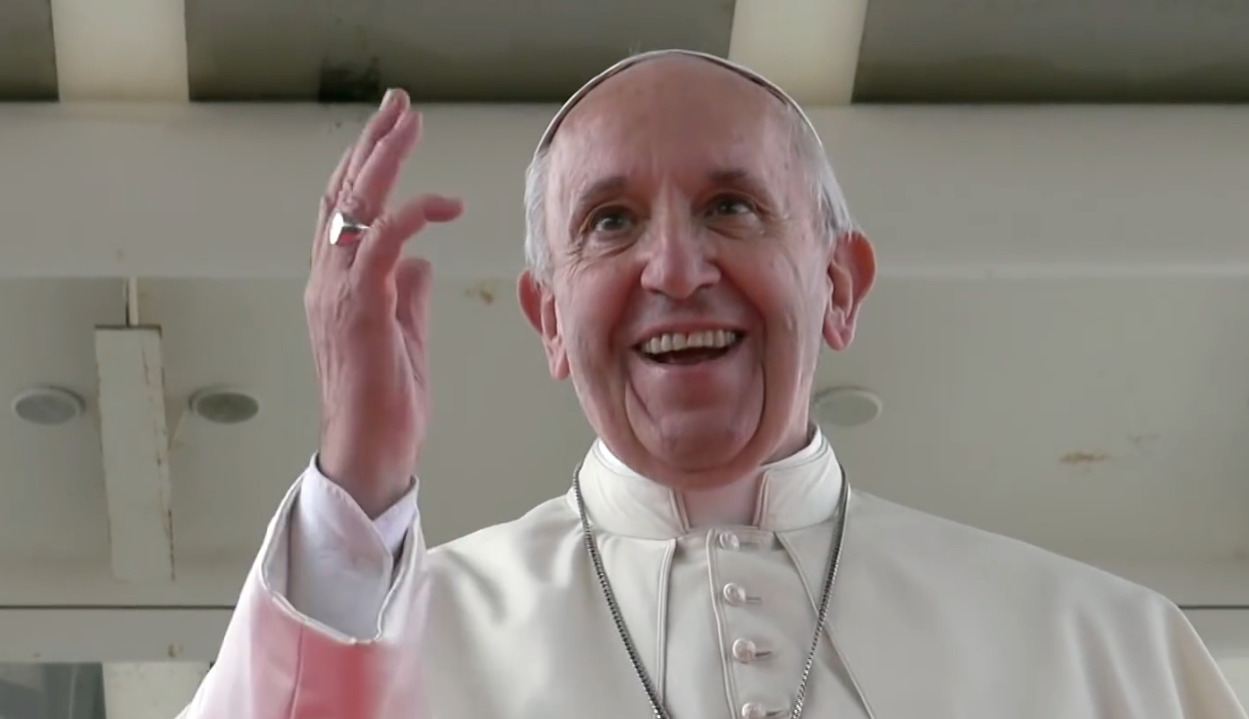
• His Holiness Pope Francis (below) makes historic visit
• REM-HF study shows no benefit with remote monitoring of cardiac devices
• ODYSSEY ESCAPE: alirocumab reduces need for apheresis in FH
• Apheresis shows promise in refractory angina
• Pulmonary hypertension and anticoagulation highlights at congress
• Our practice message podcasts (see below)
ENSURE AF: edoxaban allows prompt cardioversion in AF
Patients with atrial fibrillation (AF) who need anticoagulation before undergoing cardioversion may benefit from treatment with the non-vitamin K antagonist oral anticoagulant (NOAC), edoxaban, compared to best possible conventional therapy (warfarin and enoxaparin), according to results from the ENSURE-AF study presented during a hotline session at the meeting.
The study also showed that newly diagnosed non-anticoagulated AF patients can start edoxaban as early as two hours prior to their cardioversion procedure if they have access to transoesophageal echocardiography (TOE) or three weeks prior to the procedure without.
ENSURE-AF (Edoxaban versus Enoxaparin/Warfarin in Subjects Undergoing Cardioversion of Atrial Fibrillation), the largest randomised clinical trial of anticoagulation for cardioversion in AF patients, involved 239 study sites in 19 countries in Europe and the USA, and included 2,199 patients with non-valvular AF.
At the discretion of the physician, patients either received delayed cardioversion (non-guided TOE stratum) or early cardioversion (TOE stratum). They were then randomised equally into two anticoagulation treatments groups per stratum receiving either edoxaban (60/30 mg once daily) or enoxaparin and warfarin (INR 2.0–3.0). Some 1,095 patients were randomised to receive edoxaban and the remaining 1,104 received enoxaparin/warfarin.
Primary efficacy outcomes (a composite of stroke, systolic embolic event, myocardial infarction and cardiovascular death) were not significant being reached in 0.5% patients (n=5) in the edoxaban arm versus 1.0% (n=11) in the enoxaparin and warfarin arm.
Safety outcomes showed no increased risk of major or clinically relevant non-major bleeding, which were similarly low between the two arms.
Net clinical outcome showed a trend to better outcome in the edoxaban arm but this was not significant.
The study presenter Dr Andreas Goette (St Vincenz Hospital, Paderborn, Germany) said that while conventional anticoagulation works well, it has a major limitation in that it requires regular monitoring and dose adjustment to ensure that patients reach anticoagulation targets, which means cardioversion can sometimes be delayed for several weeks.
“Edoxaban,” he continued “may allow prompt cardioversion to be performed following the start of anticoagulation.”
Discussant of the study at the hotline session, Dr Riccardo Cappato (Policlinico San Donato, Milan, Italy) said: “Edoxaban administered at the maximally tolerated single daily dose in the peri-procedural phase of elective AF cardioversion can be considered a safe and effective alternative to VKA therapy”.
The study was simultaneously published in The Lancet (doi: 10.1016/S0140-6736(16)31474-X) on August 30th 2016.
ANNEXA-4: reversal agent shows efficacy in acute bleeding
Preliminary results in the ongoing ANNEXA-4 study have shown that andexanet can rapidly reverse anti-factor Xa activity in acutely bleeding patients and is associated with excellent or good haemostasis in most.
ANNEXA-4 (Andexanat Alfa, a Novel Antidote to the Anticoagulation Effects of FXA inhibitors) is the first study to look at andexanet in acutely bleeding patients. The study was not randomised for ethical reasons and 67 patients, who required urgent reversal of acute major bleeding within 18 hours of receiving either a direct or indirect factor Xa inhibitor, were given andexanet alfa in a bolus over 15–30 minutes followed by a two-hour infusion.
An efficacy assessment carried out in 47 patients showed an 89% decrease in anti-factor Xa activity from baseline to end of bolus for those exposed to rivaroxaban (n=26) and 93% for those exposed apixaban (n=20). At 12 hours, clinical haemostatic efficacy was rated as good to excellent in 79% of patients.
Thrombotic events occurred in 18% of patients during the 30-day follow up. “This rate of events is not unexpected considering the thrombotic potential of the patients and the fact that in most of them anticoagulation was discontinued at the time of bleeding and not restarted,” said Dr Stuart J Connolly (McMaster University, Hamilton, Ontario, Canada) speaking at the ESC hotline session where the data was presented.
CE-MARC 2: functional imaging reduces unnecessary coronary angiography
Initial investigation of patients with suspected coronary heart disease (CHD) using functional imaging – rather than National Institute for Health and Care Excellence (NICE) guideline-directed care – resulted in significantly less unnecessary angiography, according to results of the CE-MARC 2 trial.
Findings from CE-MARC 2 (Clinical Evaluation of Magnetic Resonance Imaging in Coronary Heart Disease 2) presented in a hotline session at the meeting could have an important impact on referral rates for invasive coronary angiography, and potentially healthcare costs, according to principal investigator Professor John Greenwood (University of Leeds).
The study included 1,202 patients with suspected CHD from six UK centres. Patients were randomised to functional imaging-based investigation with either:
- cardiac magnetic resonance (CMR) (n = 481)
- myocardial perfusion scintigraphy (MPS) (n = 481)
- guideline-directed investigation (n=240) based on current NICE guidelines. Within this group, those with a pre-test likelihood of 10–29% (meaning low risk for CHD based on age, gender, symptom characteristics and clinical history) were scheduled for cardiac computed tomography (CCT); those with a pre-test likelihood of 30–60% (intermediate risk) were scheduled MPS; and those with a high pre-test likelihood were sent directly to coronary angiography.
The primary end point was unnecessary coronary angiography within 12 months, (defined by absence of significant stenosis measured by fractional flow reserve or quantitative coronary angiography), with secondary end points of major adverse clinical events (MACE), and positive angiography within this same time period.
Overall, 22% of the study population underwent coronary angiography within 12 months, with unnecessary angiograms occurring in 28.8% of the NICE guidelines group, 7.5% of the CMR group, and 7.1% of the MPS group, reported Professor Greenwood.
The adjusted odds ratio of unnecessary angiography for the CMR group versus the NICE guidelines group was 0.21 (95% CI, 0.12–0.34; P < .001), with no statistically significant difference between the CMR and MPS groups. Between the three strategies, there was no difference in short-term MACE or positive angiography rates.
“Rates of invasive angiography are considered too high among patients with suspected coronary heart disease,” explained Professor Greenwood. “Our findings show that both cardiovascular magnetic resonance (CMR) and myocardial perfusion scintigraphy (MPS) significantly reduced rates of unnecessary angiography compared to guideline-directed care, with no penalty in terms of major adverse cardiovascular events (MACE). This suggests that functional imaging should be adopted on a wider basis, even in high-risk patient subgroups.”
“Worldwide, MPS is the most commonly used test to assess suspected CHD, but CMR is increasingly recognised as having high diagnostic accuracy and prognostic value,” noted Professor Greenwood. “Although the results of CE-MARC 2 showed no difference between the CMR and MPS strategies in terms of unnecessary angiography rates, our original CE-MARC study showed that CMR had a higher diagnostic accuracy compared to MPS2 and was also a stronger predictor of risk for MACE.3
He concluded that “these results show that a broader use of functional imaging (CMR or MPS), in low, intermediate and high risk patient groups, could reduce the rates of invasive angiography that ultimately show no obstructive coronary disease. In addition, CE-MARC and CE-MARC 2 further support the role of CMR as an alternative to MPS for the diagnosis and management of patients with suspected CHD.”
The study is discussed in our podcast from the meeting by Dr Jubin Joseph (St Thomas’ Hospital, London, and President of the British Junior Cardiologists’ Association). He says the results show that functional imaging should be adopted on an even wider basis than currently even in high-risk subgroups, which could potentially reduce rates of coronary angiography and costs.
References
- Greenwood JP, Ripley DP, Berry C, et al. JAMA 2016;316:1051–60. http://dx.doi.org/10.1001/jama.2016.12680
- Greenwood JP, Maredia N, Younger JF, et al. Cardiovascular magnetic resonance and single-photon emission computed tomography for diagnosis of coronary heart disease (CE-MARC): a prospective trial. Lancet 2012;379:453–60. http://dx.doi.org/10.1016/S0140-6736(11)61335-4
- Hunink MGM, Fleischmann KE. The role of randomized and nonrandomized studies in evaluating diagnostic strategies. Ann Intern Med 2016;165:61–2. http://dx.doi.org/10.7326/M16-0811
NORSTENT: drug-eluting stents no better than bare-metal stents
New generation drug-eluting stents (DES) are not superior to contemporary bare-metal stents (BMS) according to a surprise finding of the largest randomised stent trial to date, NORSTENT (the Norwegian Coronary Stent Trial).
“The efficacy of new DES versus contemporary BMS is lower than expected,” said Professor Kaare Harald Bønaa (University of Tromso – The Arctic University of Norway, and the Norwegian University of Science and Technology, Trondheim, Norway) at the ESC hotline session where the data was presented.
“Patients treated with DES do not live longer and they do not live better (in terms of quality of life) than patients treated with BMS,” he said.
With 9,013 patients and more than 40,000 patient years of follow-up, NORSTENT was an all-comers study in a usual care setting, and therefore had “the potential to yield outcomes of great relevance to clinical practice,” he added.
The multi-centre study included patients with stable angina pectoris (n=2,636) or acute coronary syndromes (n=6,377) who needed percutaneous coronary intervention (PCI). Patients were randomised to receive either BMS or DES, with 83% of DES patients receiving everolimus-eluting stents and 12% receiving zotarolimus-eluting stents.
After six years of follow-up, there was no significant difference between the DES and the BMS groups in the primary outcome of total mortality or nonfatal myocardial infarction (cumulative rate of 16.9% in the DES group versus 17.4% in the BMS group; HR 0.98), as well as secondary outcomes of unstable angina, or quality of life.
“As expected, the need for repeat revascularisation was lowered by DES, but this effect was much less than anticipated,” said Professor Bønaa. “The six-year cumulative rate of repeat revascularisation was 14.9% in the DES group versus 17.7% in the BMS group – an absolute risk reduction of 2.8%.
“Although ESC guidelines recommend new DES over BMS as default for coronary revascularisation, this recommendation may need to be modified in light of the NORSTENT findings…both stent types may be recommended,” Professor Bønaa concluded.
But discussant of the study, Professor Stefan James (Univeristy of Uppsala, Sweden), disagreed. While noting that the results were surprising, he thought the ESC guidelines should stand. “DES (new generation) should remain recommended over BMS due to better performance with 5% (53% relative risk reduction) reduction of target lesion revascularisation, 3.3% (24% relative) of any revascularistaion and a 0.4% (36% relative) reduction in stent thrombosis.
The implications of the study are also discussed in our podcast from the meeting.
The study was published simultaneously in the New England Journal of Medicine on August 30th 2016 (doi: 10.1056/NEJMoa1607991).
REM-HF trial: no benefit with remote monitoring of cardiac devices
Remote monitoring of cardiac implantable electronic devices (CIEDs) does not improve outcomes (mortality or hospitalisations) in heart failure compared to usual care, according to results from the REM-HF (The Remote Management of Heart Failure Using Implantable Electronic Devices) study.
The study was conducted in a setting “intended to maximise the benefit of remote monitoring,” commented Professor Martin Cowie (Imperial College London, and Royal Brompton Hospital, London) the co-principal investigator of the study, at the hotline session where he presented the results.
Thus the results “do not support its routine use in the management of patients with CIEDs…If patients are well-treated already, and have well-controlled symptoms, looking at remotely collected data weekly is no better than usual care,” he said.
CIEDs that are equipped with remote monitoring capabilities store data that can be downloaded and transmitted via the internet or telephone connections to their physicians for interpretation. The REM-HF study was conducted at nine British hospitals in 1,650 heart failure patients (mean age 70 years), with one of three types of CIEDs equipped for remote monitoring:
- cardiac resynchronization therapy (CRT) device with pacemaker (CRT-P);
- CRT device with defibrillator function (CRT-D);
- or implantable cardioverter-defibrillator (ICD);
Patients were randomised to receive either usual care (UC) or remote monitoring (RM).
- RM patients had data downloaded automatically from their device on a weekly basis, which was transmitted to their healthcare professional who used it to advise them about medication and lifestyle, need for additional clinic visits, or recommendations to visit their general practitioner or the emergency room. They also had the usual care delivered by their local heart failure service.
- UC patients did not have weekly automatic downloads, but had usual remote monitoring of the device (typically three to six monthly) in addition to usual care from their heart failure service.
The study’s primary end point was the first event of death from any cause or unplanned hospitalisation for cardiovascular reasons. Secondary end points included death from any cause, death from cardiovascular reasons, and unplanned hospitalisation.
After a median follow-up period of 2.8 years, no significant difference was seen between the groups in the primary end point, which occurred in 42.4% of the RM group and 40.8% of the UC group (hazard ratio 1.01; 95% confidence interval [CI] 0.87 to 1.18; P=0.87).
Secondary end points also occurred at a similar rate in both groups. “Although some studies investigating a range of remote monitoring strategies have suggested potential benefit, and adoption of remote monitoring is quite widespread, results of the REM-HF trial offer a new perspective that has the potential to change clinical practice,” said Professor John Morgan (University of Southampton) co-principal investigator of the study.
“Despite a large number of patients, considerable follow-up time, acceptable patient adherence to weekly downloads, and additional contacts with patients driven by the remotely collected data, we did not demonstrate any improvement in outcome for patients randomised to remote monitoring compared to usual care in nine English hospitals,” said Professor Cowie.
“It is possible that an effect could be demonstrated in health care systems with less well developed usual care, where patients are less-well treated and have more severe symptoms”, he concluded.
Practice messages from the study are discussed in our podcast from the meeting.
ODYSSEY ESCAPE: alirocumab reduces need for apheresis in FH
Treatment with the PCSK9 monoclonal antibody alirocumab offered the possibility of sparing lipoprotein apheresis, a therapy which is used to filter excess cholesterol from the blood, in patients with severe heterozygous familial hypercholesterolaemia (FH), according to results from the ODYSSEY ESCAPE study.6
In the UK, lipoprotein apheresis is being performed with increasing frequency, but still lags behind use in other European countries. Despite this, it is an essential treatment for homozygous FH, as well as severe heterozygous FH with progressive cardiovascular disease (CVD) refractory to combined drug therapy.
“Being able to reduce or eliminate apheresis would be a major breakthrough for these patients who spend US$50,000 to US$75,000 a year, and three to four hours every one to two weeks to clear their blood of excess LDL-C’” said Professor Patrick Moriarty (University of Kansas Medical Center, Kansas City, USA) at the hotline session where he presented the results.
ODYSSEY ESCAPE (Effect of Alirocumab on the Frequency of Lipoprotein Apheresis) was conducted in 62 patients from 14 centres in the USA and Germany undergoing regular (either every week or two weeks) lipoprotein apheresis. Patients were randomised to treatment with alirocumab 150 mg (n=41) or placebo (n=21) every two weeks for 18 weeks, while still continuing other lipid-lowering treatment. During the first six weeks, apheresis frequency was fixed to the individual’s established schedule but from week seven was only performed if low-density lipoprotein (LDL) cholesterol was <30% lower than the baseline pre-apheresis value.
Results showed that treatment with alirocumab significantly reduced the need for apheresis treatment in 75% of patients versus placebo (p<0.0001). In patients receiving alirocumab, LDL cholesterol was reduced by 54% (versus an increase of 2% on placebo), led to avoidance of at least half of apheresis treatments in 93% of patients (compared to 14.3% on placebo), and all apheresis treatment in 63% of patients.
There was some discussion about the comparability of patients enrolled by the two countries, as fewer US patients were on maximally tolerated statin (due to more statin intolerance), and consequently had higher LDL-C levels at baseline than those in Germany. Additionally, apheresis was used every two weeks in the USA but weekly in Germany. Despite these confounders, the findings have important implications for patient care and cost, according to lead author Professor Patrick Moriarty (University of Kansas Medical Center, Kansas City, USA).
According to Professor Moriarty, who speaks about the study in our podcast from the meeting, “We now have a class of drugs that should be implemented before transferring a patient for apheresis.”
The study was published simultaneously in the European Heart Journal (doi: 10.1093/eurheartj/ehw388)
Apheresis shows promise in refractory angina
A UK study presented at the lipids hotline session suggested a potential role for lipoprotein apheresis in the management of patients with refractory angina (RA) and high lipoprotein(a) [Lp(a)] levels >500 mg/dL.
Elevated Lp(a) is a cardiovascular risk factor which may promote atherosclerosis via both lipid-related, prothrombotic and anti-fibrinolytic actions. In the study ‘Apheresis as a Novel Treatment for RA and Lp(a),’ 20 patients were randomised to weekly lipoprotein apheresis or sham treatment for three months following a one month washout, crossed over to the alternative treatment for a further three months.
There was a sharp rise in myocardial blood flow post-apheresis. Compared with sham, apheresis treatment significantly improved (increase from 1.45 to 1.93, p<0.001) the primary outcome of myocardial perfusion reserve (MPR), the ratio of the myocardial blood flow at stress versus rest measured by cardiac magnetic resonance imaging. There were also significant improvements in the secondary end points of carotid wall volume and distensibility, exercise capacity, symptoms of angina, and quality of life scores.
“These findings suggest a much needed novel treatment option for these therapeutically challenging patients,” said study presenter Dr Tina Zubaida Khan (Royal Brompton and Harefield NHS Trust and Imperial College, London).
Discussant Dr Peter Libby (Brigham and Women’s Hospital, Boston, USA) said that as PCSK9 inhibitors were able to reduce Lp(a), “we may be entering an era when we could be offering patients and their families a non-apheresis treatment for reducing Lp(a)”.
New ESC clinical practice guidelines published
Four new clinical practice guidelines were published by the ESC at the Congress on:
- ESC guidelines for the diagnosis and treatment of acute and chronic heart failure
- ESC and European Association for Cardio-Thoracic Surgery (EACTS) guidelines for the management of atrial fibrillation
- ESC and European Atherosclerosis Society (EAS) guidelines for the management of dyslipidaemia (see Appendix 1, below)
- ESC Position paper on Cancer Treatments and Cardiovascular Toxicity (see Appendix 2, below).
ESC practice messages podcasts available

Watch our podcasts from the meeting, which highlights key studies and their implications for your everyday practice. We interview Professors John Camm (St George’s, University of London), Patrick Moriarty (University of Kansas Medical Center, Kansas City, USA), and Dr Jubin Joseph (St Thomas’ Hospital, London, and President of the British Junior Cardiologists’ Association).
Appendix 1: New lipid guidelines
Updated Joint ESC/European Atherosclerosis Society (EAS) Guidelines for the Management of Dyslipidaemia were published at the start of ESC Congress.1 According to EAS President, Professor Alberico L. Catapano (University of Milan and Multimedica IRCCS, Italy) lead author of this initiative, there are three key messages for clinicians.
- Although LDL-C targets have not changed, for both high and very high risk patients, a secondary target is to attain at least 50% reduction from baseline LDL‑C
- Nonfasting – rather than fasting – lipid measurement is recommended for screening, supported by evidence from a recent consensus statement2
- The guidelines re-emphasise the importance of lifestyle intervention in prevention of cardiovascular disease (CVD), across the spectrum of cardiovascular risk.
The guidelines include added information on the benefits of dietary intervention such as adoption of the Mediterranean diet. This is not just relevant for the primary prevention setting,3 but also in patients with established CVD, as shown by a report from the MOLI-SANI study.4 Among 1,197 patients with established CVD followed for a median of 7.3 years, improved adherence to the Mediterranean diet (i.e. a 2-point increase in the 9-point Mediterranean diet score) led to a 21% reduction in mortality. For patients with the highest adherence, there was a 37% risk reduction, exceeding the effects of statins.
In addition, a hotline report of a Mendelian randomisation study (a type of ‘natural clinical trial’) reinforced the potential benefit from ‘the earlier the better’ CVD prevention.5 Data from over 100,000 individuals (mean age 60.5 years, 57% women, mean LDL-C 3.4 mmol/L and mean systolic blood pressure [SBP] 126 mmHg) were evaluated using genetic scores for LDL-C (based on 46 polymorphisms or genetic variants associated with lower LDL-C) and SBP (based on 33 polymorphisms associated with lower blood pressure). Long-term exposure to even modestly lower LDL-C (by 1 mmol/L) and SBP (by 10 mmHg) was associated with 86.1% reduction in the risk of major vascular events, dramatically reducing lifetime CVD risk.
Appendix 2: New position paper on cardio-oncology
This ESC position paper aims to raise awareness of the cardiac toxicity of anticancer therapies.11 It offers guidance on how to define patients at risk; detect and prevent toxicity; and treat and follow up affected patients. The development of multidisciplinary teams, including cardiologists, oncologists, nurses, and heart failure and imaging specialists, is key to provision of best patient care.
