The promotion of exercise as a positive and powerful health intervention has never been more important, when consideration is given to the global epidemic of disease states related to a sedentary lifestyle. However, intensive exercise may be a trigger for sudden cardiac death in individuals harbouring quiescent cardiovascular diseases. Indeed, hereditary and congenital abnormalities of the heart are the most common cause of non-traumatic death during sport in young athletes.1
 The incidence of sudden cardiac death in young athletes (<35 years) is estimated at 1:50,000.2 The most common cause of death in young athletes worldwide is hypertrophic cardiomyopathy, which is implicated in over one third of all sudden cardiac deaths in young American athletes.1 Arrhythmogenic right ventricular cardiomyopathy is the most common cause of death in Italy.3 Data from a specialist cardiology pathology centre in the UK have shown that in up to 40% of cases, the heart is structurally normal. In many, such cases are often attributed to primary cardiac ion-channel disorders such as the long QT syndrome, Brugada syndrome, catecholaminergic polymorphic ventricular tachycardia, or congenital electrical accessory pathways.4 Almost 90% of deaths occur in males, and 40% of athletes are aged <18 years old.1 Data from the USA suggest that black athletes, and those participating in explosive sport of start-stop nature, such as football and basketball, may be more prone to sudden cardiac death.5,6
The incidence of sudden cardiac death in young athletes (<35 years) is estimated at 1:50,000.2 The most common cause of death in young athletes worldwide is hypertrophic cardiomyopathy, which is implicated in over one third of all sudden cardiac deaths in young American athletes.1 Arrhythmogenic right ventricular cardiomyopathy is the most common cause of death in Italy.3 Data from a specialist cardiology pathology centre in the UK have shown that in up to 40% of cases, the heart is structurally normal. In many, such cases are often attributed to primary cardiac ion-channel disorders such as the long QT syndrome, Brugada syndrome, catecholaminergic polymorphic ventricular tachycardia, or congenital electrical accessory pathways.4 Almost 90% of deaths occur in males, and 40% of athletes are aged <18 years old.1 Data from the USA suggest that black athletes, and those participating in explosive sport of start-stop nature, such as football and basketball, may be more prone to sudden cardiac death.5,6
Although the incidence of sudden cardiac death during sport is relatively low, such events are magnified by the media and have a huge impact on society as a whole. Identification of athletes at risk of sudden cardiac death has become an important focus of the medical community, on the premise that the majority of implicated diseases can be detected during life, and acceptable interventions, such as lifestyle modification, pharmacological therapy, radiofrequency ablation of accessory pathways or implantation of a cardioverter defibrillator, are available to reduce the risk of sudden cardiac death. Screening young athletes with electrocardiogram (ECG) is effective for detecting individuals with Wolff-Parkinson-White ECG pattern, the long QT syndrome and a large percentage of cardiomyopathies. Whether detection of disease equates to lives saved is a contentious issue. The most persuasive evidence supporting that early detection of disease saves lives is derived from a large prospective Italian study, which reported an 89% reduction in sudden cardiac death in athletes screened with ECG over a 25-year period.7 Despite the findings from this study, there is antagonism from some to implementing such policies in the UK. Concerns relate to a high number of false-positive results, and consequent cost implications.
Intensive exercise training is associated with a constellation of physiological alterations in autonomic tone, cardiac structure and cardiac function, which may be reflected as electrical anomalies on the ECG.8 These electrical expressions of the athlete’s heart can overlap with those observed in patients with cardiomyopathy, particularly in black athletes and in athletes participating in endurance sport.9-14
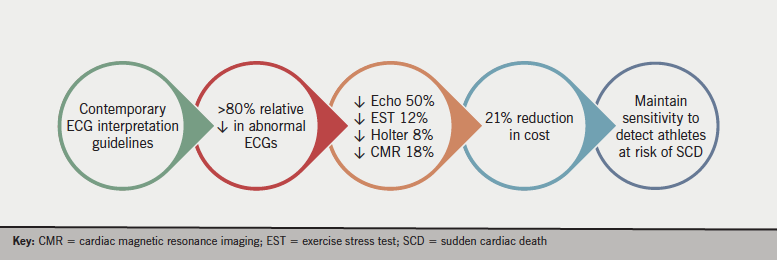
The 2010 European Society of Cardiology (ESC) recommendations for ECG interpretation in athletes are associated with a false-positive rate ranging from 9% to 22%.10,15,16 The more contemporary Seattle criteria and refined criteria for ECG interpretation in athletes have significantly improved specificity for detecting cardiac disease without compromising sensitivity.10,16,17 Whether modification of ECG interpretation criteria is associated with a significant cost reduction had never been investigated.
UK situation
The UK does not support a state-sponsored screening programme in athletes. Cardiovascular evaluation is usually reserved for young individuals with symptoms suggestive of cardiac disease, an abnormal physical examination or a family history of premature or inherited cardiac disease. However, the charitable organisation Cardiac Risk in the Young (www.c-r-y.org.uk) has an established cardiac screening programme for young individuals that also serves many professional sporting organisations in the UK.
In the August 2016 edition of the Journal of the American College of Cardiology, we took advantage of these screening data to report the cost implications of athletes being screened for cardiac disease for the first time.18 Initial screening with health questionnaire, physical examination and ECG was performed at a subsidised cost of $53 per athlete. Based on these preliminary findings, cardiologists requested secondary investigations (if applicable) to confirm or refute the presence of cardiac disease, the costs of which were calculated based on NHS tariffs in the UK. We started with calculating the costs pertaining to the number of abnormal ECGs and cost of secondary investigations based on the original 2010 ESC recommendations, and applied the potential costs of using the Seattle and refined criteria retrospectively.
Between 2011 and 2014, 4,925 previously unscreened athletes aged 14–35 years were prospectively evaluated by Cardiac Risk in the Young. Only 79 athletes (1.6%) required investigations for symptoms, family history or abnormal physical examination. An abnormal ECG, based on the 2010 ESC recommendations, was revealed in 1,072 (21.8%) athletes. Of these, 11.2% athletes required echocardiography, 1.7% exercise stress test, 1.2% Holter, 1.2% cardiac magnetic resonance imaging (MRI) and 0.4% other tests. There were 15 (0.3%) asymptomatic athletes diagnosed with potentially serious cardiac disease following investigation of an ECG classified as abnormal by all three ECG criteria. The overall cost of a de-novo screening programme using the 2010 ESC recommendations amounted to $539,888, equating to $110 per athlete and $35,993 per serious diagnosis.
The Seattle and refined criteria reduced the number of positive ECGs to 6.0% and 4.3%, respectively, and resulted in a relative reduction in the number of athletes requiring further investigation following screening by more than 50%. Specifically, the refined criteria would have resulted in a 50% reduction in the number of echocardiograms, 12% reduction in the number of exercise tests, 8% reduction in Holter monitors, and 18% reduction in the number of cardiac MRI scans that would need to be performed to confirm (or refute) the diagnosis of cardiac disease.
As a consequence of the reduction in downstream investigations, the Seattle and refined criteria reduced the cost to $92 and $87 per athlete screened and $30,251 and $28,510 per serious diagnosis, respectively, representing an impressive 21% cost saving, without compromising the sensitivity to detect serious cardiac disease (figure 1).
These results represent a welcome saving for sporting organisations equipped with the infrastructure and expertise for cardiac screening in athletes, and may also enable less financially endowed sporting organisations to afford screening for their athletes. There are persuasive arguments that such financial resources would be better served in establishing cardiopulmonary resuscitation facilities, which have proven effective in reducing the incidence of death after sudden cardiac arrest.19-21 However, one must consider that 40% of deaths in athletes occur at rest in their homes, where early access to defibrillation is unlikely, and, therefore, early identification of at-risk individuals through screening is an important preventative strategy.4
This is the most comprehensive assessment of direct cost associated with cardiovascular screening of young athletes, and the first study involving British athletes. The study highlights pertinent financial issues in relation to ECG screening in young athletes and provides a wider perspective to the ongoing debate relating to best practice in identifying young individuals at risk of sudden cardiac death.
Conflict of interest
None declared.
References
1. Maron BJ, Doerer JJ, Haas TS et al. Sudden deaths in young competitive athletes: analysis of 1866 deaths in the United States, 1980-2006. Circulation 2009;119:1085–92. https://doi.org/10.1161/CIRCULATIONAHA.108.804617
2. Harmon KG, Drezner JA, Wilson MG, Sharma S. Incidence of sudden cardiac death in athletes: a state-of-the-art review. Br J Sports Med 2014;48:1185–92. https://doi.org/10.1136/bjsports-2014-093872
3. Corrado D, Basso C, Rizzoli G, Schiavon M, Thiene G. Does sports activity enhance the risk of sudden death in adolescents and young adults? J Am Coll Cardiol 2003;42:1959–63. https://doi.org/10.1016/j.jacc.2003.03.002
4. Finocchiaro G, Papadakis M, Robertus J-L et al. Etiology of sudden death in sports: insights from a United Kingdom regional registry. J Am Coll Cardiol 2016;67:2108–15. https://doi.org/10.1016/j.jacc.2016.02.062
5. Harmon KG, Asif IM, Maleszewski JJ et al. Incidence, cause, and comparative frequency of sudden cardiac death in national collegiate athletic association athletes a decade in review. Circulation 2015;132:10–19. https://doi.org/10.1161/CIRCULATIONAHA.115.015431
6. Maron BJ, Shirani J, Poliac LC, Mathenge R, Roberts WC, Mueller FO. Sudden death in young competitive athletes: clinical, demographic, and pathological profiles. JAMA 1996;276:199–204. https://doi.org/10.1001/jama.1996.03540030033028
7. Corrado D, Basso C, Pavei A, Michieli P, Schiavon M, Thiene G. Trends in sudden cardiovascular death in young competitive athletes. JAMA 2006;296:1593–601. https://doi.org/10.1001/jama.296.13.1593
8. Pluim BM, Zwinderman AH, van der Laarse A, van der Wall EE. The athlete’s heart a meta-analysis of cardiac structure and function. Circulation 1999;100:336–45. https://doi.org/10.1161/01.CIR.101.3.336
9. Sheikh N, Sharma S. Impact of ethnicity on cardiac adaptation to exercise. Nat Rev Cardiol 2014;11:198–217. https://doi.org/10.1038/nrcardio.2014.15
10. Sheikh N, Papadakis M, Ghani S et al. Comparison of electrocardiographic criteria for the detection of cardiac abnormalities in elite black and white athletes. Circulation 2014;129:1637–49. https://doi.org/10.1161/CIRCULATIONAHA.113.006179
11. Rawlins J, Carre F, Kervio G et al. Ethnic differences in physiological cardiac adaptation to intense physical exercise in highly trained female athletes. Circulation 2010;121:1078–85. https://doi.org/10.1161/CIRCULATIONAHA.109.917211
12. Sheikh N, Papadakis M, Carre F et al. Cardiac adaptation to exercise in adolescent athletes of African ethnicity: an emergent elite athletic population. Br J Sports Med 2013;47:585–92. https://doi.org/10.1136/bjsports-2012-091874
13. Wasfy MM, DeLuca J, Wang F et al. ECG findings in competitive rowers: normative data and the prevalence of abnormalities using contemporary screening recommendations. Br J Sports Med 2015;49:200–06. https://doi.org/10.1136/bjsports-2014-093919
14. Brosnan M, La Gerche A, Kalman J et al. Comparison of frequency of significant electrocardiographic abnormalities in endurance versus nonendurance athletes. Am J Cardiol 2014;113:1567–73. https://doi.org/10.1016/j.amjcard.2014.01.438
15. Corrado D, Pelliccia A, Heidbuchel H et al. Recommendations for interpretation of 12-lead electrocardiogram in the athlete. Eur Heart J 2010;31:243–59. https://doi.org/10.1093/eurheartj/ehp473
16. Brosnan M, La Gerche A, Kalman J et al. The Seattle Criteria increase the specificity of preparticipation ECG screening among elite athletes. Br J Sports Med 2014;48:1144–50. https://doi.org/10.1136/bjsports-2013-092420
17. Riding NR, Sheikh N, Adamuz C et al. Comparison of three current sets of electrocardiographic interpretation criteria for use in screening athletes. Heart 2014;101:384–90. https://doi.org/10.1136/heartjnl-2014-306437
18. Dhutia H, Malhotra A, Gabus V et al. Cost implications of using different ECG criteria for screening young athletes in the United Kingdom. J Am Coll Cardiol 2016;68:702–11. https://doi.org/10.1016/j.jacc.2016.05.076
19. Drezner JA, Rao AL, Heistand J, Bloomingdale MK, Harmon KG. Effectiveness of emergency response planning for sudden cardiac arrest in United States high schools with automated external defibrillators. Circulation 2009;120:518–25. https://doi.org/10.1161/CIRCULATIONAHA.109.855890
20. Marijon E, Tafflet M, Celermajer DS et al. Sports-related sudden death in the general population. Circulation 2011;124:672–81. https://doi.org/10.1161/CIRCULATIONAHA.110.008979
21. Berdowski J, De Beus MF, Blom M et al. Exercise-related out-of-hospital cardiac arrest in the general population: incidence and prognosis. Eur Heart J 2013;34:3616–23. https://doi.org/10.1093/eurheartj/eht401
