A retrospective analysis of 50 inpatients admitted with syncope was undertaken to evaluate the safety and cost-effectiveness of a novel outpatient syncope clinic recently introduced within an emergency ambulatory care unit at a northwest London hospital together with review of echocardiographic parameters in syncope. Outcome measures included length of inpatient admission, frequency of cardiology review, 30-day readmission and 90-day mortality rates. The same variables were assessed prospectively in 50 inpatients referred to the syncope assessment unit (SAU). All 100 patients were deemed low risk, as defined by the San Francisco syncope rule. Patients under the age of 18 years and those investigated for conditions other than syncope were excluded. Echocardiographic parameters such as E/A ratio, left atrial (LA) dimension, left ventricular (LV) ejection fraction and E/E′ ratio were statistically analysed for their association with episodes of syncope.
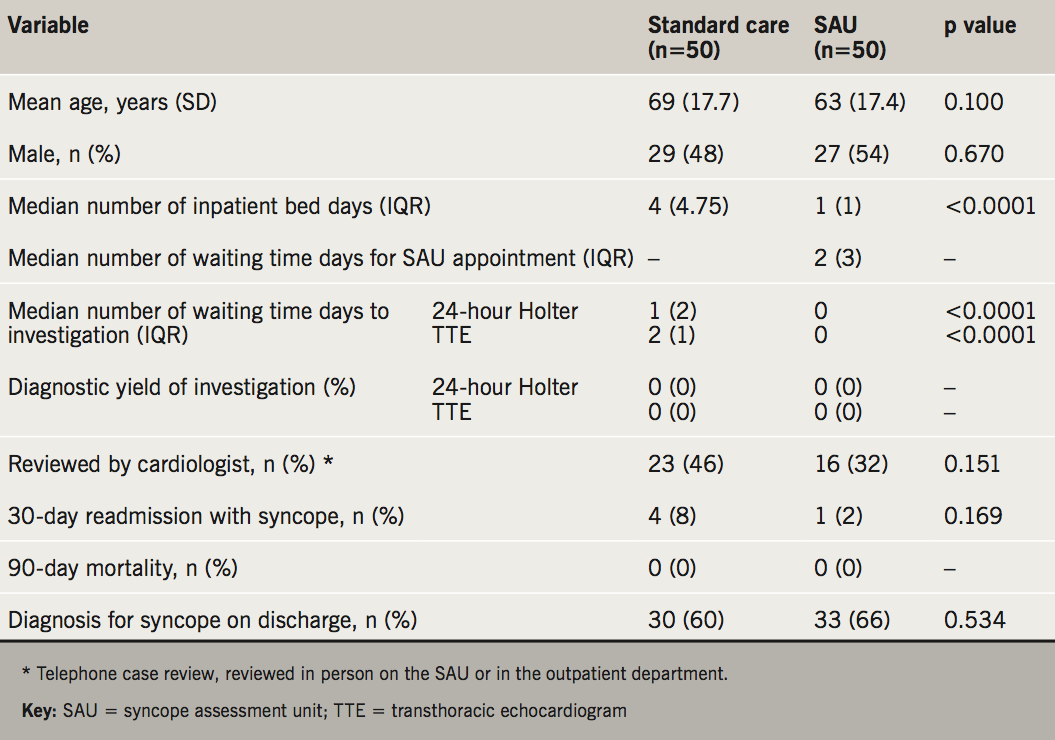
The standard-care group remained in hospital for a median four days at a cost of €582 (£512). Waiting time for an SAU appointment was a median two days. Inpatient waiting time for 24-hour Holter and transthoracic echocardiography (TTE) investigations were significantly longer for the standard-care group (p<0.05). There was no significant difference in the rates of cardiology review, diagnostic yield, hospital readmission and mortality between the two groups. The SAU will save a projected annual cost of €108,371 (£95,232) on inpatient bed days. The fractional cost of clinical assessment on the SAU is €35 (£31) per patient. Among the echocardiographic parameters analysed, increased E/E′ ratio was associated with syncope (p=0.001).
In conclusion, the introduction of a novel low-risk SAU promotes early discharge from hospital with prompt outpatient medical review and shorter inpatient waiting times for diagnostic investigations. Our data suggest this is both cost-effective and safe. E/E′ echo parameter was observed as a significant parameter in low-risk syncope.
Introduction
Up to half of the UK population will experience syncope in their lifetime,1 although only a minority will seek medical attention.2 Studies report a constant frequency of syncope in European emergency departments (EDs) with an incidence of 1% of all attendances.3 With a lifetime risk of syncope estimated at 42%,4 it accounts for significant morbidity.5,6 Uncovering the precise aetiology behind a syncopal episode remains a diagnostic challenge for clinicians, and only half of those admitted to hospital will be given a diagnosis on discharge.7
Effective management of syncope relies on early clinical evaluation by specialist staff that have access to the necessary investigations, without the need for elaborate inter-hospital referrals. Failure to adhere to such an approach can result in unnecessary hospitalisations and procedures, poorer diagnostic rates, prolonged inpatient admissions and higher health costs.4,7,8 For these reasons, the European Society of Cardiology (ESC) have recommended the establishment of formal syncope units (SUs).9 Their recommendations describe virtual or physical sites within hospitals that have access to relevant specialists and investigations.
Models of existing SUs vary in design and include: SUs located in a cardiology department, a day-care syncope evaluation unit, rapid-access blackout clinics, tertiary referral SUs and syncope observational units in the ED. Despite these recommendations, there has been no widespread establishment of SUs in UK hospitals. Acknowledged barriers to establishing these units include the low number of syncope specialists, lack of formal syncope training programmes, lack of resources, lack of supporting high-level evidence and, finally, potential increases to cost of care.10 Established SUs in the UK have primarily adopted the ‘day-care syncope evaluation unit’ model, as seen in Newcastle,11,12 and, more recently, Manchester. The primary outcome of these, and similar syncope day-care assessment unit (SAU) models adopted in Europe,8,13,14 was a reduction in reported health costs and an increase in the rate of diagnostic yield. This was respectively achieved by reducing the frequency of inpatient admissions and unnecessary investigations.10
Ambulatory emergency care units (AECUs) are well established in UK hospitals and have now become key to the flow of patients through the overstretched EDs. AECUs provide rapid access to inpatient diagnostics, therapies and access to specialist services with the overall aim of avoiding admission, facilitating inpatient discharge, reducing length of stay and improving overall patient satisfaction. We established a novel pathway for outpatient referral of patients presenting to the ED with low-risk syncope to a SU located in the AECU. Our unit is complemented with direct access to specialists and cardiovascular investigations such as 24-hour ambulatory electrocardiogram (ECG) monitoring (Holter) and transthoracic echocardiography (TTE). This provides an alternative syncope assessment unit (SAU) model, which blends well within the widely established AECUs.
The objective of this study was to evaluate the safety and cost-effectiveness of managing low-risk syncope patients within a newly introduced SAU at a northwest London hospitals NHS trust. This care pathway was established following discussion at clinical commissioning group and primary care funding group meetings. A comparative analysis was performed between usual practice and a standardised method of syncope assessment and management on the SAU.
Echocardiography is often performed in patients presenting with suspected cardiac syncope, i.e. patients with cardiac symptoms, previous cardiac history and/or an abnormal ECG. Although the diagnostic yield of echocardiography has been reported to be low,14 the association between echo parameters and episodes of syncope has not been studied extensively.
Method
The standard-care model was assessed via retrospective analysis. Three hundred and forty-five consecutive patients discharged with a diagnosis of syncope from December 2013 to December 2014 were identified from hospital coding records. Electronic discharge notifications and medical notes of these 345 admissions were then scrutinised. Patients in whom the presentation was not consistent with the ESC definition of syncope (“transient loss of consciousness due to transient global hypoperfusion characterised by rapid onset, short duration, and spontaneous recovery”),9 categorised as high risk by the San Francisco rule,15 under the age of 18 years, or remained in hospital for investigation of an alternative diagnosis to syncope were excluded; leaving 50 patients.

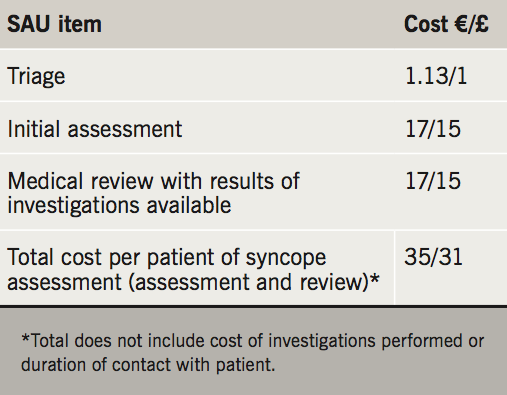
A prospective analysis of 50 patients referred to the newly introduced SAU was then undertaken. These patients were referred to the SAU on discharge from hospital following initial medical assessment. All patients referred to the SAU met the ‘low-risk syncope pathway’ criteria (figure 1). The one-stop SAU took place in the local AECU and was led by acute medical physicians with access to TTE and portable 24-hour Holter monitoring. These investigations were requested by medical physicians following clinical review on the SAU. Occasionally, the investigations were requested before review on the SAU using clinical information described on the referral document or discharge letter from the ED. Patients were referred for same-day specialist inpatient or later outpatient review, as appropriate. Measured variables of the 100 patients included: length of inpatient admission, waiting time to investigation (24-hour Holter and TTE), frequency of cardiology review, 30-day readmission rate with syncope, 90-day mortality rate and diagnostic rate of syncope. Student’s t-test and chi-squared tests were used to compare continuous and categorical data, respectively. Two-tailed tests of significance used an α-level of 0.05. Analyses were performed using STATA software, version 14. Cost figures were calculated using information obtained from the in-hospital coding and finance department. The relevant itemised cost figures for assessment and medical review are summarised in table 1.
Echocardiogram
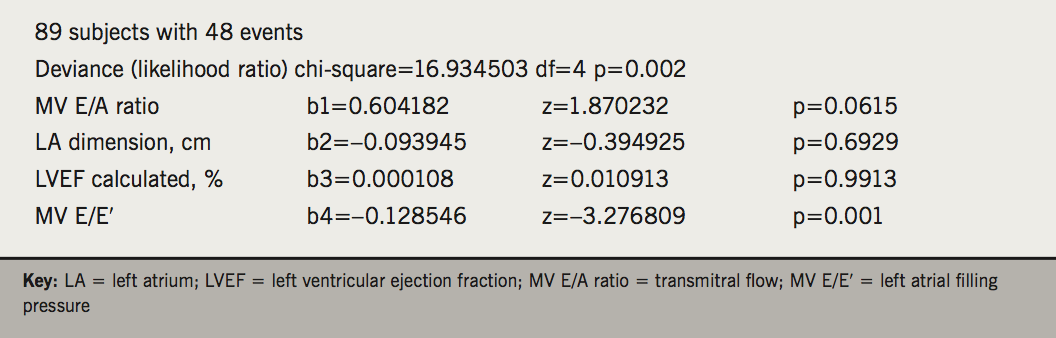
Echocardiography was performed on patients presenting with low-risk syncope. The aim was to look for structural or functional cardiac abnormalities. Various echo parameters were analysed between patients presenting with syncope versus non-syncope patients presenting to the ambulatory care unit. Each syncopal episode was recorded as an event and a Cox-regression analysis was performed (using Stats direct) to ascertain the significance of various echo parameters.
Results
Characteristics for the 100 patients are summarised in table 1. There was no statistically significant difference in mean age or sex between the standard-care and SAU cohorts. The standard-care group remained in hospital for a median four days (interquartile range [IQR] 4.75) compared with the SAU group, who were all discharged from hospital within 24 hours (p<0.05). The total number of inpatient days was reduced by 80% for the SAU group. Waiting time for an SAU appointment from the time of hospital discharge was a median two days (IQR 3). Inpatient waiting time for 24-hour Holter and TTE investigations were significantly longer for the standard-care group at a median one day (IQR 2) (p<0.05) and two days (IQR 1) (p<0.05), respectively. There was a trend toward increasing frequency of cardiology review in the standard-care cohort (46% vs. 32%), although this did not reach statistical significance (p=0.151). There was a higher 30-day readmission rate with syncope for the standard-care group (4%) compared with the SAU group (2%), although this, again, was not statistically significant (p=0.169). Finally, there was no mortality in either group at 90 days. Diagnostic rate for syncope was higher for the SAU group (66%), although this was not statistically significant (p=0.534).

Cost data
Patients admitted for assessment of syncope remained in hospital for a median four days at a cost of €582 (£512) – €145 (£128) per bed day. A total of 93 patients were referred on the low-risk syncope pathway to the SAU in the first six months of service. At this rate of referral, the SAU will save a projected annual cost of €108,371 (£95,232) on inpatient bed days alone (table 2). The cost of clinical assessment on the SAU is €35 (£31) per patient (table 3). The cost calculations are based on approximate running costs and do not take into account the duration of contact by medical staff with the patient or the running costs of the equipment. The marginal cost of inpatient clinical assessment is, therefore, €546 (£481) per patient. The cost of investigations performed on the SAU does not differ from those performed on the wards for inpatients.
Echocardiography
An analysis of the echocardiographic data of consecutive patients with syncope was performed using Stats Direct® software. A Cox-regression analysis was performed and this showed that patients with increased E/E′ ratio had increased risk of syncope. The other parameters such as E/A ratio, left atrial (LA) dimension and left ventricular ejection fraction (LVEF) did not show any significant association with syncope (box 1).
Discussion
Despite recommendations by the ESC9 to streamline the evaluation of syncope through adoption of syncope units, much variation in strategy exists. Our comparative study evaluated syncope outcomes of 50 patients referred to an ambulatory SAU versus 50 receiving standard inpatient care. Our results suggest that the SAU model adopted within an established AECU complemented with direct access to cardiovascular investigations and specialists is cost-effective and allows safe discharge of patients. These conclusions are consistent with those drawn from previous studies evaluating syncope units of a similar design.11,12,16
For each patient referred to the SAU, an average €582 (£512) is saved on inpatient bed days. The current rate of referral from the ED to the SAU is 16 patients per month, which equates to a projected annual saving of €108,371 (£95,232) on inpatient bed days alone. Although a formal cost analysis of the SAU was not performed in this study, it appears cost-effective compared with standard care. We believe that the adoption of syncope units similar in design would be cost-effective throughout the UK, given the widespread fractional cost of outpatient/ambulatory assessment (table 2). Referral of patients to the SAU improves the quality of care provision by releasing acute medical beds to those who are sick and require hospital admission. Not only does the pathway ease the strain on acute medical and cardiology inpatient services; it also provides prompt outpatient assessment and access to specialist investigations at the patient’s convenience. Patients referred to the SAU were promptly seen within a median of two days. None of the 50 patients inside this short time period re-presented with syncope. Mortality outcomes furthermore support the conclusion that the pathway is not only cost-effective, but also safe.
Our study includes adults under the age of 65, which differs from previous UK studies that have evaluated outcomes predominantly in the elderly population group.11,12 This makes conclusions from our study easier to generalise to the adult attendees of all ages to the ED. We believe a further strength of our study is that the service is led by acute medical physicians, unlike others who have utilised geriatricians,11,12,16 nurses and cardiologists17-19 as primary assessors. We feel providing a service run by acute medical physicians with a holistic approach best compliments the population group being primarily assessed on syncope units as described in this study.
Investigators in the Syncope Evaluation in the Emergency Department Study20 evaluated a pathway for the assessment and management of intermediate risk patients presenting with syncope to the ED.20 This prospective, single-centre study randomised patients to standard care or syncope unit evaluation. They found that the total number of patient hospital days was reduced by >50% for the syncope unit group and that evaluation of patients on the syncope unit had no adverse effect on all-cause mortality or recurrent syncope events versus standard care. These findings taken from a considerably larger cohort are similar to those reported in our study.
More recently, the EDOSP (ED Observation Syncope Protocol) study evaluated an ED syncope protocol implemented within the community, university and hospital setting.20 A total of 124 patients deemed at intermediate risk were randomised to standard hospital care versus the observational unit protocol. Similar to the SAU described in our study, clinicians had access to 24-hour Holter monitoring and echocardiography for selected patients. They reported reductions in hospital admission rates (15% vs. 92%) and length of hospital admissions (29 vs. 47 hours) for those assessed on the observational unit. Furthermore, there was no difference in serious 30-day outcomes occurring after discharge, cost of care, or quality-of-life between the two groups.21
Our study has shown similar results to the above studies. We believe that this SAU model incorporated within the already established AECU is feasible, cost-effective and safe. We, therefore, recommend this model to all acute hospitals with AECUs to help reduce acute hospital admissions, length of stay and eventually save hospital bed days.
We found a strong association between syncopal event and increased E/E′ ratio. This could be associated with the presence of essential hypertension. However, our sample size is small and further large studies would be needed to assess the association of other echo parameters in detail with an aim to further risk-stratify the patients with syncope.
Study limitations
One obvious limitation of the study is the relatively small number of patients evaluated. The time scale was also short – only three months – and two different time periods were compared. A larger cohort with more long-term outcome data is required before firmer conclusions are drawn on safety and cost-effectiveness. It is also worth noting that the prospective data were collected in the introduction phase of the SAU. More reliable conclusions may be drawn once staff in the ED and SAU have familiarised themselves with the referral pathway and structure of the SAU. The findings in this study cannot be applied to all syncope units given varying cost of staffing, training and available resource space. The diagnostic tests performed on the unit are important drivers of cost that were not evaluated in the study. Although not a planned part of this study, it would be clearly desirable in future studies.
Conclusions
The introduction of a novel low-risk SAU promotes early discharge from hospital with prompt outpatient medical review and shorter inpatient waiting times for diagnostic investigations. Our data suggest that this is both cost-effective and safe. This has cost implications to the National Health Service (NHS). Furthermore, E/E′ ratio was observed as a significant echo parameter in the low-risk cohort.
Key messages
- History taking and clinical examination are paramount in distinguishing between high-risk and low-risk syncope
- A syncope unit within an ambulatory-care setting helps to save costs and, at the same time, provides a safe pathway for evaluating patients with low-risk syncope
- Syncope units cut length of stay in hospital and improve patient experience, with quicker access to cardiac diagnostics
Conflict of interest
None declared.
Acknowledgements
We sincerely thank Dr Myura Nagendran and Dr Sothinathan Gurunathan for their work in data collection, analysis and review of the paper.
References
1. National Institute for Health and Care Excellence. Transient loss of consciousness (blackouts) management in adults and young people. CG109. London: NICE, 2010. Available from: https://www.nice.org.uk/guidance/cg109
2. Fitzpatrick AP, Cooper P. Diagnosis and management of patients with blackouts. Heart 2006;92:559–68. https://doi.org/10.1136/hrt.2005.068650
3. Soteriades ES, Evans JC, Larson MG et al. Incidence and prognosis of syncope. N Engl J Med 2002;12:878–85. https://doi.org/10.1056/NEJMoa012407
4. Ammirati F, Colivicchi F, Minardi G et al. The management of syncope in the hospital: the OESIL Study (Osservatorio Epidemiologico della Sincope nel Lazio). G Ital Cardiol 1999;5:533–9.
5. Da Silva RM. Syncope: epidemiology, etiology, and prognosis. Front Physio 2014;5:471. https://doi.org/10.3389/fphys.2014.00471
6. Sun BC, Hoffman J, Mangione C et al. Older age predicts short term, serious events after syncope. J Am Geriatr Soc 2007;55:907–12. https://doi.org/10.1111/j.1532-5415.2007.01188.x
7. Kenny RA. Evidence-based algorithms and the management of falls and syncope in the acute medical setting. Clin Med 2008;8:157–62. https://doi.org/10.7861/clinmedicine.8-2-157
8. Brignole M, Ungar A, Bartoletti A et al. Standardized-care pathway vs. usual management of syncope patients presenting as emergencies at general hospitals. Europace 2006;8:644–50. https://doi.org/10.1093/europace/eul071
9. Moya A, Sutton R, Ammirati F et al. Guidelines for the diagnosis and management of syncope (version 2009). Eur Heart J 2009;30:2631–71. https://doi.org/10.1093/eurheartj/ehp298
10. Kenny RA, Brignole M, Dan GA et al. Syncope unit: rationale and requirement – the European Heart Rhythm Association position statement endorsed by the Heart Rhythm Society. Europace 2015;17:1325–40. https://doi.org/10.1093/europace/euv115
11. Kenny RA, O’Shea D, Walker HF. Impact of a dedicated syncope and falls facility for older adults on emergency beds. Age Ageing 2002;31:272–5. https://doi.org/10.1093/ageing/31.4.272
12. Newton JL, Marsh A, Frith J, Parry S. Service for older people. Age Ageing 2010;39:265–8. https://doi.org/10.1093/ageing/afp252
13. Ammirati F, Colaceci R, Cesario A et al. Management of syncope: clinical and economic impact of a syncope unit. Europace 2008;10:471–6. https://doi.org/10.1093/europace/eun061
14. Chang NL, Shah P, Bajaj S, Virk H, Bikkina M, Shamoon F. Diagnostic yield of echocardiography in syncope patients with normal ECG. Cardiol Res Pract 2016;2016:1251637. https://doi.org/10.1155/2016/1251637
15. Quinn JV, Stiell IG, McDermott DA, et al. Derivation of the San Francisco syncope rule to predict patients with short-term serious outcomes. Ann Emerg Med 2004;43:224–32. https://doi.org/10.1016/S0196-0644(03)00823-0
16. Parry SW, Frearson R, Steen N, Newton JL, Tryambake P, Kenny RA. Evidence-based algorithms and the management of falls and syncope presenting to acute medical services. Clin Med 2008;8:157–62. https://doi.org/10.7861/clinmedicine.8-2-157
17. Brignole M, Ungar A, Bartoletti A et al. Standardized care pathway versus usual management of syncope referred in emergency to hospitals (EGSYS 2). Europace 2006;8:644–50. https://doi.org/10.1093/europace/eul071
18. Fedorowski A, Burri P, Juul-Moller S, Melander O. A dedicated investigation unit improves management of syncopal attacks (Syncope Study of Unselected Population in Malmo–SYSTEMA I). Europace 2010;12:1322–8. https://doi.org/10.1093/europace/euq168
19. Ungar A, Tesi F, Chisciotti VM et al. Assessment of a novel management pathway for patients referred to the emergency department for syncope: results in a tertiary hospital. Europace 2016;18:457–62. https://doi.org/10.1093/europace/euv106
20. Shen WK, Wyatt W, Decker W et al. Syncope Evaluation in the Emergency Department Study (SEEDS): a multidisciplinary approach to syncope management. Circulation 2004;110:3636–45. https://doi.org/10.1161/01.CIR.0000149236.92822.07
21. Sun BC, McCreath H, Liang LJ et al. Randomized clinical trial of an emergency department observation syncope protocol versus routine inpatient admission. Ann Emerg Med 2014;64:167–75. https://doi.org/10.1016/j.annemergmed.2013.10.029
