Introduction
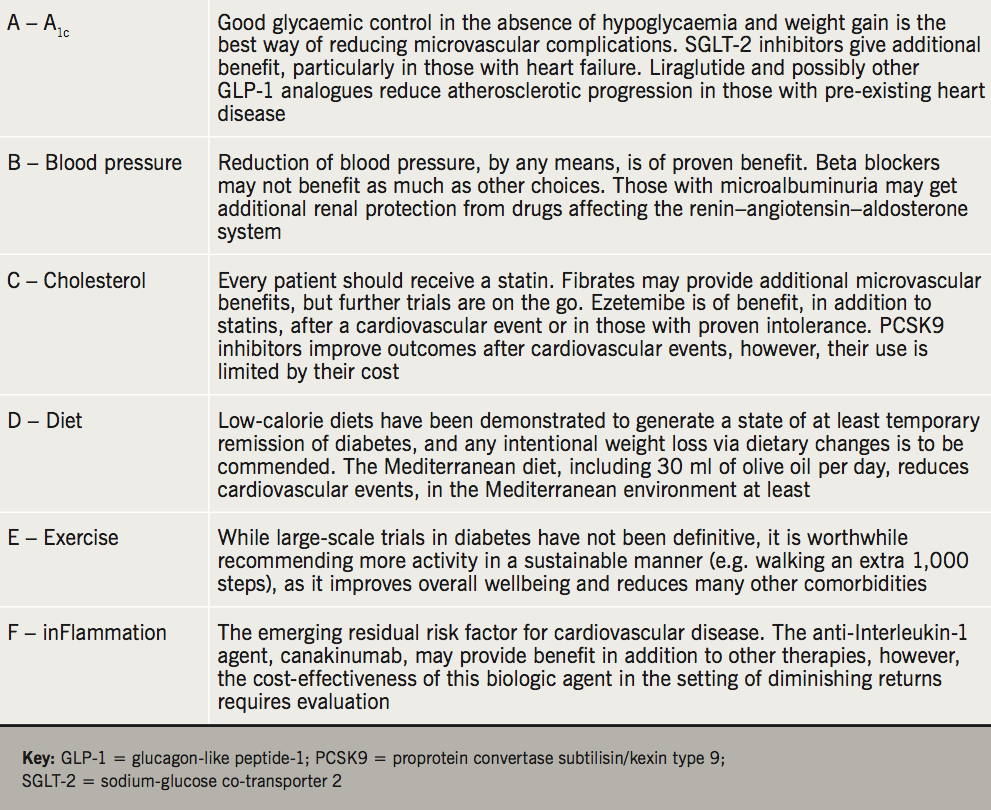
Throughout this supplement, there has been discussion of the epidemiology of cardiovascular disease within people with diabetes, and a focus on the management of glycaemia. Given that the majority of people with diabetes ultimately die a premature cardiovascular death, diabetes management has become synonymous with cardiovascular risk reduction. However, since the United Kingdom Prospective Diabetes Study (UKPDS),1 it has become increasingly clear that the multi-factorial nature of diabetes requires a multi-factorial approach. Initially, much of this was extrapolated from existing cardiovascular data, with diabetes just being regarded as another risk factor, however, as the understanding of the pathophysiology of type 2 diabetes and the metabolic syndrome has grown, so too has the realisation that the impact of treating risk factors within diabetes requires specific study. Herein, we will review existing interventions, with a particular focus on where those with diabetes require specific consideration, before exploring future therapies.
Lifestyle intervention
For many years, diet and exercise have been regarded as the cornerstone of the management of diabetes. This was predominantly based on the robust observation that the progression of impaired glucose tolerance to diabetes could be, at least in part, arrested by a programmed diet and exercise intervention. Indeed, in the Diabetes Prevention Program (DPP) in the USA, and a Finnish study by the same name, diet and exercise regimens proved superior to pharmacological intervention with metformin in reducing progression to the diagnosis.2,3 The latter of these studies also demonstrated a ‘legacy effect’ with the benefit of the diet and exercise programme persisting beyond the active intervention. Therefore, it was anticipated that the Look AHEAD (Action for Health in Diabetes) study would provide the evidence of a beneficial impact of a lifestyle programme on people with diabetes.4
The Look AHEAD study commenced in 2001 with the intention of recruiting approximately 5,000 people with diabetes and exposing them to a multi-factorial lifestyle intervention. The elements of the study included supported graded exercise goals commencing at 50 minutes per week and increasing over 26 weeks to >175 minutes per week, and dietary intervention, reducing portion size and providing meal replacements, in order to achieve a balanced consumption of 1,200 to 1,500 kcal/day for those <114 kg at baseline and 1,500 to 1,800 kcal/day for those ≥114 kg. There were additional behaviour modification interventions in the form of group sessions over the first year and individualised monthly contact sessions, either in person or by telephone, subsequently. These focused on the advantages of self-monitoring and recording of food and portion size intake, and positive feedback from weekly ‘weigh-in’ sessions, all of which have significant evidence of improved weight loss.5 For those who were not responding to these interventions (defined as <1% weight loss – given that weight neutrality is itself an achievement on a trajectory of weight gain for most people with diabetes), remedial strategies were in place including motivational interviews, mutually agreed written contracts and lifestyle counsellors, competitive campaigns to achieve personalised goals with rewards for achievements.
This multi-factorial lifestyle strategy was remarkably successful, with the average weight loss at 12 months being 8.6% of baseline bodyweight compared with 0.7%, which persisted, albeit attenuated, to the end of the study. The average amount of exercise performed was 136.7 minutes per week, which was associated minute-by-minute with 12-month weight loss, such that the more exercise performed the greater the weight loss. The success of the study in achieving these targets was already marred by questions regarding the cost-effectiveness of these interventions, and whether it would be possible to translate this to the population at large. The study was discontinued in 2012, however, due to cardiovascular disease (CVD) futility. Despite, having successfully achieved the primary goals of weight loss and improved physical fitness, with associated improvements in high-density lipoprotein (HDL)-cholesterol, glycosylated haemoglobin (HbA1c), blood pressure and waist circumference, using less pharmacotherapy, there had been a failure to show any difference in the primary outcome of cardiovascular event rate, with 403 adjudicated events occurring in the intervention arm compared with 418 events in the control arm (hazard ratio 0.95, 95% confidence interval [CI] 0.83 to 1.09).
The reasons for the absence of benefit have been a subject of great discussion. First, the event rate was very low, due to good multi-factorial assessments of patients prior to enrolment, the preponderance of women and non-smokers within the study population and good blood pressure control in both groups. In the study population, there would be diminishing returns from any intervention that may have required longer than 10 years to become apparent. Further, this study was initiated prior to the ubiquitous use of statin therapy. The improvements in cholesterol achieved through diet and exercise resulted in fewer statin prescriptions in the active arm, losing any potential pleiotropic benefit thereof. A secondary analysis of the Look AHEAD study has highlighted that ‘responders’ who achieved 10% weight loss in the first 12 months of the study, irrespective of which arm they were randomised to, experienced 21% fewer cardiovascular events, suggesting that where weight loss can be achieved it is of benefit, however, this comes with all the caveats of post-hoc analysis, notably differences in the predisposition of those who achieved the weight loss, versus those that did not, within the same intervention group.6 It is also important to note that, even in the absence of cardiovascular benefit, those randomised to the intervention had improvements in quality of life, lower risk of microvascular outcomes, a smaller tablet burden and improvements in multiple other measures of general wellbeing. This means that diet and exercise persists as a first-line intervention for most, if not all, people with diabetes.
Low-calorie diet
There is a prevailing hypothesis that the metabolic abnormalities that are associated with diabetes are an evolutionary adaptation to prolonged periods of famine (the thrifty phenotype).7 This is used to explain the observation of the distribution across different ethnic populations, such that those that have endured recurrent episodes of famine, such as the Pima American Native Indians, have a very high prevalence of diabetes, whereas populations that have not had historic exposure to food shortages, such as the Chinese, have a low prevalence.
The protective role of a natural dietary intervention, simulating the famine that their genotype and phenotype is adapted to, has been explored in those with recently diagnosed diabetes. It was demonstrated that an 825 kcal per day diet can put up to 45.6% of people with early diabetes into remission after 12 months, compared with 4% of the population using medication alone.8 In the 306 participants of the study, the benefit was proportionate to weight loss, such that those who lost in excess of 10 kg achieved 57% remission rates, whereas 34% of the population who achieved 5–10 kg weight loss were in remission at 12 months. This was independent of treatment arm, although, expectedly, all of the participants achieving higher weight loss were on the low-calorie diet.
This study reports the 825 kcal per day diet, made up of a food-replacement formula, was well tolerated with no participants dropping out, however, it has to be recognised that enrolment into this study took over three years to recruit 306 newly diagnosed patients who were prepared to participate, representing approximately a quarter of people who were approached. Therefore, although this may appear a very effective treatment strategy in a clinical trial, pragmatically, it may not be the most effective intervention for the population as a whole, and the longer-term results of this intervention require further evaluation.
Specific nutrition interventions
Current nutrition recommendations for individuals follow the protocol used within the Look AHEAD study (despite its failure to show any benefit) of restricting fat to <30% of total calories and <10% from saturated fat, and a balance of fruits, vegetables and protein. Additional benefit on triglycerides, the principle dyslipidaemia of insulin resistance, has been suggested by simple practices, such as limiting alcohol intake, substituting healthy fats (e.g. monounsaturated fatty acids, polyunsaturated fatty acids) for saturated and trans fats, limiting added sugars, engaging in regular physical activity, and losing excess weight. These changes can reduce triglycerides by 20% to 50%, although have not been demonstrated to reduce cardiovascular events per se.
The Mediterranean diet is the only nutritional intervention demonstrated to impact events. An intervention of either virgin olive oil (approximately 1 litre per week) or 30 g per day of mixed nuts added to a low-fat diet was tested against the low-fat diet alone in a Spanish general population in the Prevenćion con Dieta Mediterránea (PREDIMED) study.9 Those patients randomised to either arm of the Mediterranean diet had a 30% reduced risk of CVD events. The pre-specified diabetes subgroup demonstrated a similar 29% reduction in the primary three-point composite outcome of stroke, myocardial infarction and cardiovascular mortality.
Dietary supplements
To date, many supplements, including antioxidant vitamins C or E, B vitamins, specific fatty acids (e.g. omega-3 fatty acids) or the inorganic nitrites found in beetroot juice, have suggested reductions in cardiovascular risk factor profile, however, none have translated this into a clinical benefit in larger-scale randomised-controlled trials in people with diabetes.10-13 Given the inconsistency between the diabetes prevention programmes and the Look Ahead study between those at risk of and those with a diagnosis of diabetes, caution must be exercised when extrapolating results from the general population to those with diabetes, although as we know from other studies, intentional weight loss can have large benefits across a number of domains of health, so should be encouraged by sustainable changes in diet and activity levels.
Antihypertensive therapy
The benefit of blood pressure control was highlighted during UKPDS, where a relatively modest systolic blood pressure reduction of 10 mmHg was associated with approximately twice the benefit of improved glycaemic control.13 As the majority of people with diabetes have hypertension, this has become of particular interest. The risk of stroke, myocardial infarction and all-cause mortality is directly proportional to blood pressure, therefore, the need to intervene is not controversial. However, two specific questions remain unanswered; namely, what is the optimal target blood pressure and are there any pleiotropic benefits from the therapeutic options?
Optimal target blood pressure
The UKPDS and Hypertension Optimal Treatment (HOT) study both demonstrated the benefit of intensive blood pressure control on a wide range of macro- and microvascular outcomes. Neither of these studies, however, demonstrated a threshold of optimum treatment, indeed, neither study achieved the target systolic blood pressure of 140 mmHg, in both cases only achieving a final blood pressure of 144 mmHg systolic.13,14 Subsequent studies have explored the impact of more aggressive control, achieving systolic blood pressure targets of <130 mmHg in people with hypertension and diabetes on a variety of outcomes, including stroke, myocardial infarct, retinopathy and nephropathy. The ACCORD (Action to Control Cardiovascular Risk in Diabetes) study, in a factoral design, measured the impact of intensive glycaemic and blood pressure control in a population of 4,733 people with type 2 diabetes.15 Those randomised to intensive blood pressure control recorded a blood pressure of 119 mmHg after 12 months, compared with 133 mmHg in the conventional control arm. This realised a 51% reduction in strokes, however, it failed to show benefit in the primary composite outcome, including myocardial infarction and mortality, nor in mortality alone. The ADVANCE (Action in Diabetes and Vascular Disease: Preterax and Diamicron Modified Release Controlled Evaluation) study achieved a blood pressure of 136/74 mmHg over 4.3 years, compared with 140/75 mmHg in 11,140 people with type 2 diabetes, by the addition of a fixed-dose combination of perindopril and indapamide.16 This difference in blood pressure reduced all-cause mortality by 14% and cardiovascular mortality by 18%, although it failed to show a benefit in either macro- or microvascular morbidity at the end of the study. Over the subsequent 5.9 years, a representative 8,494 participants continued to provide data to the study group. Over this time the blood pressure converged to 137/74 mmHg within a year. The mortality benefit persisted, albeit attenuated to 9% and 12%, respectively, however, there remained no additional benefit in terms of morbidity, indeed the trends for microvascular outcomes were consistently on the wrong side of the point of unity, although none came close to statistical significance.
Attaining these tighter blood pressure targets, however, do not come without risk. The majority of people with type 2 diabetes will require multiple agents in order to achieve these targets, and with polypharmacy comes greater risk of adverse consequences. ACCORD and the Ongoing Telmisartan Alone and in Combination With Ramipril Global End-point Trial (ONTARGET) demonstrated that the use of multiple antihypertensive drugs was associated with an increased incidence of serious adverse effects, including hypotension, syncope, and worsening renal function.17 Specifically, the ACCORD blood pressure trial found that serious adverse events occurred in 3.3% of the intensive blood pressure-lowering arm compared with 1.3% in the usual care arm.15
Agents of choice in people with diabetes
The second consideration in hypertension management is the choice of agent. There is good evidence that angiotensin-converting enzyme (ACE) inhibitors, angiotensin-receptor antagonists (ARBs), calcium channel blockers and diuretics are useful in the treatment of hypertension in diabetes.18,19 In the Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (ALLHAT), doxazosin was clearly inferior to chlorthalidone, with the rates of CVD 24% higher and a 2.14-fold increase in heart failure in the diabetes subgroup treated with doxazocin compared with chlorthalidone. Similarly, although the composite end point over the duration of the study was the same, event rate was 10% higher for CVD, and 15% higher for both stroke and heart failure with lisinopril than with the thiazide-like diuretic.20 This has caused significant controversy, in several camps, particularly those who favour the use of drugs acting on the renin–angiotensin–aldosterone cascade, who for many years had advocated the use of ACE inhibitors as first line for those with diabetes. While there is clear evidence of a reno-protective effect in those with micro- and macro-albuminuria,21,22 the evidence does not support any additional benefit. In practice, blood pressure control in those with diabetes is more difficult than in the general population, resulting in the majority of patients with diabetes requiring combination therapy.23 As a result, it becomes an academic issue as to which to choose first. There is a synergistic benefit from thiazides and ACE inhibitors/ARBs, therefore, this does appear a logical early intervention, and the exact order of initiation is unlikely to have significant impact in either direction.
Beta blockers, however, do not fare as well in the studies. It is well established that beta blockers marginally increase glycaemia, which caused a significant increase in incident diabetes in the atenolol arm of the Anglo-Scandinavian Cardiac Outcomes Trial-Blood Pressure Lowering Arm (ASCOT-BPLA) trial compared with amlodipine.24 Other trials have demonstrated increases in triglycerides and reduced HDL-cholesterol with beta blockers, suggesting this may be an effect on insulin resistance rather than just glycaemia, as was originally thought.25 As a result, most guidelines direct away from the use of beta blockers in the early management of hypertension. Newer agents such as carvedilol, nebivolol and bisoprolol promise more specificity and benefit mediated through vasodilatation, or at least inhibition of vasoconstriction, rather than attenuating cardiac output. Although this has not been formally tested as yet, consensus statements have been made, based on mechanistic studies of insulin resistance and surrogate markers. These suggest, given the prevalence of resistant hypertension, newer beta blockers are probably a suitable third- or fourth-line agent once the proven thiazides, ACE inhibitors/ARBs and calcium channel blockers have been tried.26
Antiplatelets
Outside of diabetes, the use of aspirin for primary prevention for men and secondary prevention in both men and women, often in combination with additional antiplatelet agents is one of the least controversial recommendations in multiple guidelines based on high-quality data.27 Primary prevention for women is often advocated because of the proven benefit on reducing stroke, although the evidence in ischaemic heart disease for women in the general population is ambiguous.28
In those with diabetes, however, the evidence is less clear-cut. There have been six trials reported to date that include an a priori diabetes subset analysis, and three others specifically examining the effects of aspirin in diabetes. Meta-analysis of these studies suggests a relatively similar reduction in myocardial infarction and stroke of approximately 9% that did not reach statistical significance in their own right.29 When treated as a single composite outcome these did achieve statistical significance in some, but not all, analyses. Interestingly, however, there were significant discrepancies based on the sex of participants included in the analysis, such that trials with predominantly women saw a non-significant increase in the myocardial infarction risk of approximately 10%, balanced by a reduction in stroke risk of a third. Paradoxically, studies with more than 50% men saw stroke rate increase by approximately 5% but myocardial infarction risk reduced by 29%. The hypothesis that this is in some way associated with aspirin resistance, which can affect up to 40% of people with diabetes, is countered by the observation that the adverse consequences of bleed risk, predominantly gastrointestinal, was symmetrically doubled in both men and women. There is no clear explanation for the sex difference by vascular bed, either statistical or pathophysiological, leading to a lack of consensus across international guidelines. In practice, the use of aspirin for primary prevention of cardiovascular events should be individualised based on a risk:harm assessment comparing the baseline cardiovascular risk versus the risk of gastrointestinal disorders. In general, there is a background risk of gastrointestinal bleeds of 0.1% per annum. A diagnosis of diabetes does not itself contribute to this, although the polypharmacy of diabetes may do. An individual with an estimated 10-year CVD risk greater than 10% may gain benefit, compared with the potential for harm, however, it must be remembered that many of the risk factors for ischaemic heart disease, such as smoking, are also independent risk factors for gastrointestinal bleeding, and the doubling of bleed risk seen with aspirin often contributes more to the risk of harm than the potential for gain. If it is deemed aspirin would be of greater benefit than risk of harm, a dose of 75 mg on alternate days is often all that is required, however, in practice, alternate-day regimens may pose the risk of reducing medication adherence in the absence of regular routine.
Currently, there is no proven role for clopidogrel, nor indeed any other antiplatelet agent, in primary prevention of CVD in people with diabetes. Further, no simple, clinically relevant test exists to identify those with aspirin resistance, who may benefit from clopidogrel. Studies exploring the roles of these antiplatelet agents in secondary prevention have not shown any interactions between the benefits of dual antiplatelet therapy in those with and without diabetes, suggesting a symmetrical response. Therefore, those with diabetes should have dual antiplatelet therapy prescribed in accordance with local guidance for secondary prevention of CVD.
Lipid-lowering therapies
Type 2 diabetes with insulin resistance is associated with a very distinctive dyslipidaemia, characterised by elevated triglycerides, reduced HDL-cholesterol and particularly small and dense low-density lipoprotein (LDL)-cholesterol. The LDL-cholesterol concentration may be misleading because they are more prone to oxidation and glycation, rendering them more atherogenic, and the increased density generates more particles for any given concentration.30 Nevertheless, the relationship between LDL particle size and CVD is confounded by many other CVD risk factors. Thus, targeting changes in LDL size to reduce CVD risk is not in itself indicated.31
LDL-cholesterol lowering in type 2 diabetes
LDL-cholesterol is identified as the primary target of lipid-lowering therapy. The focus on LDL-cholesterol is supported by results of multiple randomised-controlled trials utilising a range of HMG-CoA reductase inhibitors (statins) in those with and without diabetes. Data from 18,686 individuals with diabetes (1,466 with type 1 and 17,220 with type 2) during a mean follow-up of 4.3 years demonstrated a 21% proportional reduction in major vascular events per 1 mmol/L (39 mg/dL) reduction in LDL-cholesterol in people with diabetes (relative risk 0.79, 99%CI 0.72 to 0.86, p<0.0001) and a 9% proportional reduction in all-cause mortality per 1 mmol/L reduction in LDL-cholesterol (relative risk 0.91, 99%CI 0.82 to 1.01, p=0.02).32 These results were independent of baseline cholesterol or cardiovascular risk, whether primary or secondary prevention status. Given the good tolerability of statins, and relatively low risk for significant side effects, the majority of patients should receive statin therapy of some description. The notable exceptions include the very elderly, who would not have sufficient life-expectancy for other reasons to receive benefit from statin therapy, or younger patients with diabetes, who have a very low cardiovascular risk.
Triglyceride-lowering in type 2 diabetes
Triglyceride-rich lipoproteins, especially pro-atherogenic very low-density lipoprotein (VLDL), are often elevated in patients with diabetes, particularly at diagnosis. As such, these represent a secondary target of lipid-lowering therapy that should be considered only after the initiation and therapeutic response achieved to statin and antihyperglycaemic therapies, unless they are greater than 10 mmol/L (900 mg/dl) when the risk of hypertriglyceridaemia-induced pancreatitis becomes apparent. Despite recommendations from the National Cholesterol Education Program Adult Treatment Panel and American Diabetes Association (ADA)/American Heart Association (AHA) suggesting a target of 1.69 mmol/L (150 mg/dL) there is only limited evidence that this reduces CVD risk in either those with or without diabetes. This is predominantly due to poor trial design, under-powering and over-estimation of the residual risk of diabetes in a post-statin, ACE inhibitor and beta blocker world.
The Veterans Affairs High-Density Lipoprotein Intervention Trial (VA-HIT) was carried out in men with known CVD and low levels of HDL-cholesterol (<40 mg/dL) using gemfibrozil.33 The significant improvement on cardiovascular events was driven by a relative risk reduction of 32% in those with diabetes compared with the 22% relative risk reduction seen in the 75% of participants without diabetes. Importantly, however, no participants in VA-HIT were on statins, rendering it impossible to compare the benefit achieved here against what is currently accepted as standard of care today. The Bezafibrate Infarction Prevention (BIP) trial included 1,470 participants with diabetes out of the 4,570 total participants.34 It failed to achieve its primary end point, however, in a post hoc analysis, those with diabetes experienced a significant 25% reduction in cardiovascular events, although, again, this was in the absence of any concomitant statin therapy. The Fenofibrate Intervention and Event Lowering in Diabetes (FIELD) trial was conducted exclusively in patients with diabetes.35 Although statins were not in common usage at the start of the study, there was a drop-in rate of 23% in the placebo group and 14% in the fenofibrate group. This also failed to demonstrate a reduction in cardiovascular events, possibly due to the confounding of statin use in the placebo group, however, it did demonstrate a substantial reduction in microvascular outcomes, including a 30% reduction in the need for laser photocoagulation over three years and substantially better renal outcomes, that could not be accounted for by any other parameter in the study, including the lipid changes. These microvascular benefits have not been observed in statin studies, making investigators explore whether this is a fibrate-specific peroxisome proliferator-activated receptor alpha (PPARα) effect.36 Studies exploring this are underway, however, as a result, many retinologists will advocate fibrate therapy in those with evidence of diabetic retinopathy, in order to delay progression to anti-VEGF (vascular endothelial growth factor) intra-vitreal injections or laser photocoagulation. With this exception, however, fibrates should be considered only as an intervention for those who are intolerant of statin therapy, or in those with sustained very high triglyceride levels.
Add-on therapies to statins for further lipid control
The atherothrombosis intervention in metabolic syndrome with low HDL/high triglycerides: impact on global health outcomes (AIM-HIGH) trial tested the addition of niacin in statin-treated patients with known CVD, including in 34% of patients with diabetes.37 After three years, however, despite increasing median HDL-cholesterol from 0.91 to 1.09 mmol/L (35 to 42 mg/dL), lowering triglycerides from 1.85 to 1.38 mmol/L (164 to 122 mg/dL), and lowered LDL-cholesterol from 1.92 to 1.61 mmol/L (74 to 62 mg/dl), the trial was discontinued due to lack of efficacy at the pre-defined interim analysis point of three years. Those with diabetes performed exactly the same as those without.
The use of dalcetrapib, another HDL-cholesterol-raising therapy inhibiting the cholesterol ester transfer protein, was tested in 15,871 patients, 25% of whom had diabetes, who had experienced a recent acute coronary syndrome.38 Like niacin, dalcetrapib raised HDL-cholesterol by approximately a third, although had no impact on LDL-cholesterol. Also, like the AIM-HIGH trial, this study was terminated early due to futility.
Success was achieved with ezetimibe in the Improved Reduction of Outcomes: Vytorin Efficacy International Trial (IMPROVE-IT).39 There were 18,144 people, post-cardiac event, randomised to receive simvastatin supplemented with either ezetimibe or placebo. There was a 6.4% reduction in events, however, this was driven by a statistically significant interaction such that the 27% of the population with diabetes had a 5.5% absolute risk reduction (relative risk reduction [RRR] 15%, 95%CI 22–6%), whereas those without diabetes achieved a non-significant 0.6% absolute risk reduction. A diabetes-specific sensitivity analysis has recently reported suggesting that all people with diabetes benefited irrespective of baseline risk.40
Near future interventions
Despite optimal statin therapy, blood pressure control and glycaemic regulation, there remains significant residual cardiovascular risk within diabetes. Several strategies are being explored to further reduce this risk. The two most promising strategies include reducing the residual cholesterol risk and newer strategies exploring the role of inflammation in CVD.
Residual cholesterol risk
Proprotein convertase subtilisin/kexin type 9 (PCSK9) modulates the interaction between the LDL molecule and the cellular receptors, resulting in the internalisation and degradation of the LDL-receptor. Monoclonal antibodies to inhibit PCSK9 enable recycling of the LDL-receptor and, therefore, increase clearance of cholesterol from the blood stream. Meta-analysis of 10,159 individuals in the phase 2 and 3 programme for this class, including alirocumab, evolocumab, and bococizumab, demonstrated a 47% reduction in LDL-cholesterol, with an associated 55% reduction in all-cause mortality, 50% reduction in cardiovascular mortality and 51% reduction in myocardial infarction.41 Prospective randomised-controlled trials have shown some benefit, although not to this magnitude, possibly due to their being performed on background statin therapy, which was not universal in the earlier programmes. The Further Cardiovascular Outcomes Research with PCSK9 Inhibition in Subjects with Elevated Risk (Fourier) trial demonstrated a 15% reduction in the primary composite outcome of cardiovascular death, myocardial infarction, stroke, hospitalisation for unstable angina, or coronary revascularisation, and a similar 2% absolute risk reduction translating to a 20% relative risk reduction.42 Diabetes was a pre-specified eligibility criterion for recruitment into the Fourier trial. An a priori stratified analysis demonstrated marginal (non-significant) greater benefit in those with diabetes of 17% relative risk reduction (2.7% vs. 1.6% absolute benefit for those with and without diabetes, respectively) in the primary outcome and the same 2.0% absolute risk reduction in secondary outcome in both groups.
The use of these biologics, however, faces a significant health economic challenge, with a number needed to treat of 50 for three years to prevent a single event. When combined with the high manufacturing cost of biologic therapies, currently, this means the use of these agents is prohibitively expensive.
Targeting inflammation risk
Inflammation has been implicated in the progression of atherosclerotic disease and, as a result, multiple strategies have been evaluated. There has been recent focus on strategies to reduce the pro-inflammatory cytokine interleukin (IL)-1. Inhibition at any point, whether directly against IL-1, the IL-1β subunit or against the receptor have all been demonstrated to reduce IL-6 and high-sensitivity C-reactive protein (hsCRP). Clinical trials of gevokizumab, a direct IL-1 inhibitor, however, were abandoned due to futility, despite promising pre-clinical work, and further development has been discontinued.42,43 More promising results have been achieved with canakinumab, a specific monoclonal antibody to IL-1β, the major inflammatory mediator interacting with the IL-1 receptor. The Canukinumab Anti-inflammatory Thrombosis Outcome Study (CANTOS) randomised 10,061 to receive one of three doses of canakinumab or placebo.44 The higher two doses of canakinumab achieved a 39% reduction in hsCRP without altering the LDL-cholesterol. This achieved a further 15% reduction in the primary composite outcome of cardiovascular mortality, myocardial infarction and stroke on a background of statin therapy with optimal blood pressure control and glycaemic control in those with diabetes. Although there was no significant interaction, the approximate 40% of study participants with diabetes as a group achieved a statistically significant reduction in the primary outcome and secondary outcome, including hospitalisation for heart failure and coronary intervention, which was not achieved in the population without diabetes. The absolute risk reduction in a population, however, was only 0.6 events per 100 patient-years, requiring 56 patients to be treated for three years to prevent one event. Again, given the cost of manufacturing this biological agent, there will be substantial hurdles to be overcome before these make it into common practice.
Horizon scanning
The biggest hurdle to further therapeutic options for the management of cardiovascular risk in those with diabetes is highlighted in the case of both PCSK9 inhibitors and the anti-inflammatory agents. With each readily available intervention, such as the statins, blood pressure control, the sodium-glucose co-transporter 2 (SGLT-2) inhibitors and the glucagon-like peptide-1 (GLP-1) analogues, the residual risk of cardiovascular events is reduced. Future interventions are dependent on identifying novel therapeutic targets and mechanisms for interacting with these targets. With the growing financial constraints on global healthcare, combined with the increased prevalence of diabetes, there is growing demand to repurpose existing interventions, with limited success. Alternatively, development of novel biological therapies is very precise, with maximal benefit from a specific target, but are likely to come at a cost that is not viable in the current healthcare model.
Summary
The primary goal of managing people with diabetes is to reduce the risk of the vascular complications of hyperglycaemia and the associated metabolic syndrome. Although recent reports have moved the focus of this back to specific antihyperglycaemic drugs, the most effective way of maintaining health in people with diabetes remains diet and activity, particularly in early diabetes prior to pancreatic failure, specific dietary interventions, such as the Mediterranean diet, good blood pressure control, however that is achieved, and statin therapy. There is a role for the addition of aspirin and clopidogrel after an event, although the risk of complications outweighs the potential benefit in those with diabetes in primary prevention. Similarly, after an event, there may be a role for the addition of ezetimibe to optimal statin therapy in those with residual cholesterol risk. There is growing evidence to support the use of biologic agents to further reduce cholesterol beyond statin therapy, although these have not been compared with ezetimibe, and the cost of biological therapy renders them not cost-effective within most healthcare systems. There is a growing interest in targeting inflammation with specific agents, which may be of future interest, however, it is likely to be hampered by the cost of the specific monoclonal antibodies that are being tested.
Key messages
- Although good glycaemic control in diabetes remains the optimal way to reduce microvascular complications, cardiovascular risk reduction is a priority in the management of type 2 diabetes
- Lifestyle intervention may not provide cardiovascular (CV) benefit in those with diabetes, although, as it improves overall wellbeing, it should still be advocated
- Good blood pressure control, however achieved, is essential
- People with diabetes should receive a statin unless there is a compelling reason not to
- If cholesterol targets are not achieved on statin alone, or a patient is intolerant, ezetimibe may provide additional benefit in those with diabetes and previous CV event
- There is no role in primary prevention for antithrombotics, although aspirin and/or clopidogrel should be used in secondary prevention
- Newer biological agents may have a role in the very high risk, however, the cost-effectiveness of such strategies has not been evaluated
Conflict of interest
WDS has received speaker honoraria, conference sponsorship, unrestricted educational grants, and/or attended meetings sponsored by AstraZeneca, Boehringer Ingelheim, Bristol Myers Squibb, Eli Lilly, Glaxo SmithKline, Merck, Napp, Novartis, Novo Nordisk, Pfizer, Sanofi Aventis, Servier and Takeda. He holds research grants from AstraZeneca, Novo Nordisk and Novartis. WDS would like to acknowledge the support of the NIHR Exeter Clinical Research Facility and the NIHR Collaboration for Leadership in Applied Health Research and Care (CLAHRC) for the South West Peninsula. The views expressed in this publication are those of the author(s) and not necessarily those of the NIHR Exeter Clinical Research Facility, the NHS, the NIHR or the Department of Health in England.
Other articles in this supplement include:
Introduction
1. The cardiovascular profile in diabetes
2. Diabetes and cardiovascular risk in UK South Asians: an overview
3. Drugs for diabetes: the cardiovascular evidence base
References
1. UK Prospective Diabetes Study (UKPDS) Group. Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33). Lancet 1998;352:837–53. https://doi.org/10.1016/S0140-6736(98)07019-6
2. Lindstrom J, Ilanne-Parikka P, Peltonen M et al. Sustained reduction in the incidence of type 2 diabetes by lifestyle intervention: follow-up of the Finnish Diabetes Prevention Study. Lancet 2006;368:1673–9. https://doi.org/10.1016/S0140-6736(06)69701-8
3. Diabetes Prevention Program Research Group. 10-year follow-up of diabetes incidence and weight loss in the Diabetes Prevention Program Outcomes Study. Lancet 2009;374:1677–86. https://doi.org/10.1016/S0140-6736(09)61457-4
4. The Look AHEAD Research Group. Cardiovascular effects of intensive lifestyle intervention in type 2 diabetes. N Engl J Med 2013;369:145–54. https://doi.org/10.1056/NEJMoa1212914
5. Burke LE, Wang J, Sevick MA. Self-monitoring in weight loss: a systematic review of the literature. J Am Diet Assoc 2011;111:92–102. https://doi.org/10.1016/j.jada.2010.10.008
6. The Look AHEAD Research Group. Association of the magnitude of weight loss and changes in physical fitness with long-term cardiovascular disease outcomes in overweight or obese people with type 2 diabetes: a post-hoc analysis of the Look AHEAD randomised clinical trial. Lancet Diabetes Endocrinol 2016;4:913–921. https://doi.org/10.1016/S2213-8587(16)30162-0
7. Lindsay RS, Bennett PH. Type 2 diabetes, the thrifty phenotype – an overview. Br Med Bull 2001;60:21–32. https://doi.org/10.1093/bmb/60.1.21
8. Leslie WS, Taylor R, Harris L, Lean MEJ. Weight losses with low-energy formula diets in obese patients with and without type 2 diabetes: systematic review and meta-analysis. Int J Obes (Lond) 2017;41:96–101. https://doi.org/10.1038/ijo.2016.175
9. Estruch R, Ros E, Salas-Salvadó, J et al. Primary prevention of cardiovascular disease with a Mediterranean diet. N Engl J Med 2013;368:1279–90. https://doi.org/10.1056/NEJMoa1200303
10. Burke MF, Burke FM, Soffer DE. Review of cardiometabolic effects of prescription omega-3 fatty acids. Curr Atheroscler Rep 2017;19:60. https://doi.org/10.1007/s11883-017-0700-z
11. Gilchrist M, Winyard PG, Fulford J, Anning C, Shore AC, Benjamin N. Dietary nitrate supplementation improves reaction time in type 2 diabetes: development and application of a novel nitrate-depleted beetroot juice placebo. Nitric Oxide 2014;40:67–74. https://doi.org/10.1016/j.niox.2014.05.003
12. Mahmoodi MR, Kimiagar M, Mehrabi Y. The effects of omega-3 plus vitamin E and zinc plus vitamin C supplementation on cardiovascular risk markers in postmenopausal women with type 2 diabetes. Ther Adv Endocrinol Metab 2014;5:67–76. https://doi.org/10.1177/2042018814548028
13. UK Prospective Diabetes Study Group. Tight blood pressure control and risk of macrovascular and microvascular complications in type 2 diabetes: UKPDS 38. BMJ 1998;317:703–13. https://doi.org/10.1136/bmj.317.7160.703
14. Hansson L, Zanchetti A, Carruthers SG et al. Effects of intensive blood-pressure lowering and low-dose aspirin in patients with hypertension: principal results of the Hypertension Optimal Treatment (HOT) randomised trial. HOT Study Group. Lancet 1998;351:1755–62. https://doi.org/10.1016/S0140-6736(98)04311-6
15. The ACCORD Study Group. Effects of intensive blood-pressure control in type 2 diabetes mellitus. N Engl J Med 2010;362:1575–85. https://doi.org/10.1056/NEJMoa1001286
16. Chalmers J, Arima H, Woodward M et al. Effects of combination of perindopril, indapamide, and calcium channel blockers in patients with type 2 diabetes mellitus: results from the Action In Diabetes and Vascular Disease: Preterax and Diamicron Controlled Evaluation (ADVANCE) trial. Hypertension 2014;63:259–64. https://doi.org/10.1161/HYPERTENSIONAHA.113.02252
17. Bohm M, Schumacher H, Teo KK et al. Achieved blood pressure and cardiovascular outcomes in high-risk patients: results from ONTARGET and TRANSCEND trials. Lancet 2017;389:2226–37. https://doi.org/10.1016/S0140-6736(17)30754-7
18. Emdin CA, Rahimi K, Neal B et al. Blood pressure lowering in type 2 diabetes: a systematic review and meta-analysis. JAMA 2015;313:603–15. https://doi.org/10.1001/jama.2014.18574
19. Blood Pressure Lowering Treatment Trialists’ Collaboration. Effects of different blood pressure-lowering regimens on major cardiovascular events in individuals with and without diabetes mellitus: results of prospectively designed overviews of randomized trials. Arch Intern Med 2005;165:1410–19. https://doi.org/10.1001/archinte.165.12.1410
20. Wright JT Jr, Probstfield JL, Cushman WC et al. ALLHAT findings revisited in the context of subsequent analyses, other trials, and meta-analyses. Arch Intern Med 2009;169:832–42. https://doi.org/10.1001/archinternmed.2009.60
21. Tatti P, Pahor M, Byington RP et al. Outcome results of the Fosinopril Versus Amlodipine Cardiovascular Events Randomized Trial (FACET) in patients with hypertension and NIDDM. Diabetes Care 1998;21:597–603. https://doi.org/10.2337/diacare.21.4.597
22. Lewis EJ, Hunsicker LG, Clarke WR et al. Renoprotective effect of the angiotensin-receptor antagonist irbesartan in patients with nephropathy due to type 2 diabetes. N Engl J Med 2001;345:851–60. https://doi.org/10.1056/NEJMoa011303
23. Mancia G, Schumacher H, Redon J et al. Blood pressure targets recommended by guidelines and incidence of cardiovascular and renal events in the Ongoing Telmisartan Alone and in Combination With Ramipril Global Endpoint Trial (ONTARGET). Circulation 2011;124:1727–36. https://doi.org/10.1161/CIRCULATIONAHA.110.008870
24. Dahlof B, Sever PS, Poulter NR et al. Prevention of cardiovascular events with an antihypertensive regimen of amlodipine adding perindopril as required versus atenolol adding bendroflumethiazide as required, in the Anglo-Scandinavian Cardiac Outcomes Trial-Blood Pressure Lowering Arm (ASCOT-BPLA): a multicentre randomised controlled trial. Lancet 2005;366:895–906. https://doi.org/10.1016/S0140-6736(05)67185-1
25. Daae LN, Westlie L. A 5-year comparison of doxazosin and atenolol in patients with mild-to-moderate hypertension: effects on blood pressure, serum lipids, and coronary heart disease risk. Blood Press 1998;7:39–45. https://doi.org/10.1080/080370598437556
26. Brunstrom M, Eliasson M, Nilsson PM et al. Blood pressure treatment levels and choice of antihypertensive agent in people with diabetes mellitus: an overview of systematic reviews. J Hypertens 2017;35:453–62. https://doi.org/10.1097/HJH.0000000000001183
27. Antithrombotic Trialists Collaboration. Aspirin in the primary and secondary prevention of vascular disease: collaborative meta-analysis of individual participant data from randomised trials. Lancet 2009;373:1849–60. https://doi.org/10.1016/S0140-6736(09)60503-1
28. Berger JS, Lala A, Krantz MJ, Baker GS, Hiatt WR. Aspirin for the prevention of cardiovascular events in patients without clinical cardiovascular disease: a meta-analysis of randomized trials. Am Heart J 2011;162:115–24.e2. https://doi.org/10.1016/j.ahj.2011.04.006
29. Fox CS, Hill Golden S, Anderson C et al. Update on prevention of cardiovascular disease in adults with type 2 diabetes mellitus in light of recent evidence: a scientific statement from the American Heart Association and the American Diabetes Association. Diabetes Care 2015;38:1777–803. https://doi.org/10.2337/dci15-0012
30. Soran H, Durrington PN. Susceptibility of LDL and its subfractions to glycation. Curr Opin Lipidol 2011;22:254–61. https://doi.org/10.1097/MOL.0b013e328348a43f
31. Koska J, Saremi A, Bahn G et al. The effect of intensive glucose lowering on lipoprotein particle profiles and inflammatory markers in the Veterans Affairs Diabetes Trial (VADT). Diabetes Care 2013;36:2408–14. https://doi.org/10.2337/dc12-2082
32. Cholesterol Treatment Trialists Collaboration. Efficacy of cholesterol-lowering therapy in 18,686 people with diabetes in 14 randomised trials of statins: a meta-analysis. Lancet 2008;371:117–25. https://doi.org/10.1016/S0140-6736(08)60104-X
33. Rubins HB, Robins SJ, Collins D et al. Gemfibrozil for the secondary prevention of coronary heart disease in men with low levels of high-density lipoprotein cholesterol. Veterans Affairs High-Density Lipoprotein Cholesterol Intervention Trial Study Group. N Engl J Med 1999;341:410–18. https://doi.org/10.1056/NEJM199908053410604
34. Bezafibrate Infarction Prevention Study. Secondary prevention by raising HDL cholesterol and reducing triglycerides in patients with coronary artery disease. Circulation 2000;102:21–7. https://doi.org/10.1161/01.CIR.102.1.21
35. The FIELD study investigators. Effects of long-term fenofibrate therapy on cardiovascular events in 9795 people with type 2 diabetes mellitus (the FIELD study): randomised controlled trial. Lancet 2005;366:1849–61. https://doi.org/10.1016/S0140-6736(05)67667-2
36. Keating GM, Ormrod D. Micronised fenofibrate: an updated review of its clinical efficacy in the management of dyslipidaemia. Drugs 2002;62:1909–44. https://doi.org/10.2165/00003495-200262130-00013
37. The AIM-HIGH Investigators. Niacin in patients with low HDL cholesterol levels receiving intensive statin therapy. N Engl J Med 2011;365:2255–67. https://doi.org/10.1056/NEJMoa1107579
38. Schwartz GG, Olsson AG, Abt M et al. Effects of dalcetrapib in patients with a recent acute coronary syndrome. N Engl J Med 2012;367:2089–99. https://doi.org/10.1056/NEJMoa1206797
39. Cannon CP, Blazing MA, Giugliano RP et al. Ezetimibe added to statin therapy after acute coronary syndromes. N Engl J Med 2015;372:2387–97. https://doi.org/10.1056/NEJMoa1410489
40. Giugliano RP, Cannon CP, Blazming MA et al. Benefit of adding ezetimibe to statin therapy on cardiovascular outcomes and safety in patients with versus without diabetes mellitus: results from IMPROVE-IT (Improved Reduction of Outcomes: Vytorin Efficacy International Trial). Circulation 2018;137:1571–82. https://doi.org/10.1161/CIRCULATIONAHA.117.030950
41. Navarese EP, Kołodziejczak M, Schulze V et al. Effects of proprotein convertase subtilisin/kexin type 9 antibodies in adults with hypercholesterolemia: a systematic review and meta-analysis. Ann Intern Med 2015;163:40–51. https://doi.org/10.7326/M14-2957
42. Sabatine MS, Giugliano RP, Wiviott SD et al. Efficacy and safety of evolocumab in reducing lipids and cardiovascular events. N Engl J Med 2015;372:1500–09. https://doi.org/10.1056/NEJMoa1500858
43. Ridker PM, Luscher TF. Anti-inflammatory therapies for cardiovascular disease. Eur Heart J 2014;35:1782–91. https://doi.org/10.1093/eurheartj/ehu203
44. Ridker PM, Everett BM, Thuren T et al. Antiinflammatory therapy with canakinumab for atherosclerotic disease. N Engl J Med 2017;377:1119–31. https://doi.org/10.1056/NEJMoa1707914