Depressive symptoms in coronary artery disease (CAD) are known to associate with increased mortality. We evaluated management of depression screening in the outpatient setting for patients with known CAD at ambulatory visits. We assessed whether depression screening was performed with a patient health questionnaire, as well as what was done with positive results. Our study identified 355 patients who visited an ambulatory primary care clinic over a three-year period, 57% of whom were screened at least once. Positive scores for depression were found in 20% of patients screened, with 54% of screening-positive patients given plans for additional care. We found disparities between screening rates, with whites screened least for depression, as well as in management plans, with whites given highest probability of mentioned treatment in their assessment and plan if depression screening was positive. Given the association with increased mortality in known CAD, depression screening may represent an opportunity to decrease health outcomes disparities and to improve outcomes for patients with CAD in the outpatient setting.

Introduction
Depression is a significant cause of morbidity and mortality in patients with coronary artery disease (CAD), with depressive symptoms affecting up to 45% of patients with CAD.1 Cardiac patients with depressive symptoms experience a 2 to 2.5-fold mortality increase when compared with cardiac patients without depressive symptoms.2 Screening tools include the patient health questionnaire (PHQ), which exists in two- and nine-question formats, with PHQ2 being nearly 90% sensitive and 73% specific for depression,3 and PHQ9 being 88% sensitive and 88% specific for depression.4 We examined the records of patients with CAD in an ambulatory clinic to determine the rates and management of depression screening.
Materials and method
We performed a retrospective chart review of all patients at an ambulatory clinic with previously documented CAD from 2015 through 2018. We included all patients seen for primary care appointments during this time, and utilised the first positive PHQ screen (PHQ2 or PHQ9) in any primary care appointment note during this period. If PHQ screening was performed at least once at any time during the study period, the patient was considered screened. Positive screening was defined as PHQ2 score of 3 or greater, or PHQ9 score of 10 or greater. If a positive PHQ2 screen was followed on the same date by a negative PHQ9, this was considered a negative screen. Mention of elevated PHQ screening was defined as a mention of the patient’s screening result or mental health in the assessment and treatment section of the note on the date of the elevated screen. To assess disparities in the gender and race categories for screening rates, chi-square testing was performed. To minimise influence of uncontrolled factors, including transient positive depression screening that did not correlate with true diagnosis of depression, as well as diagnosis of depression outside of the primary care setting, we only assessed whether depression screening was positive and did not include actual diagnosis of depression in our analysis.
Results
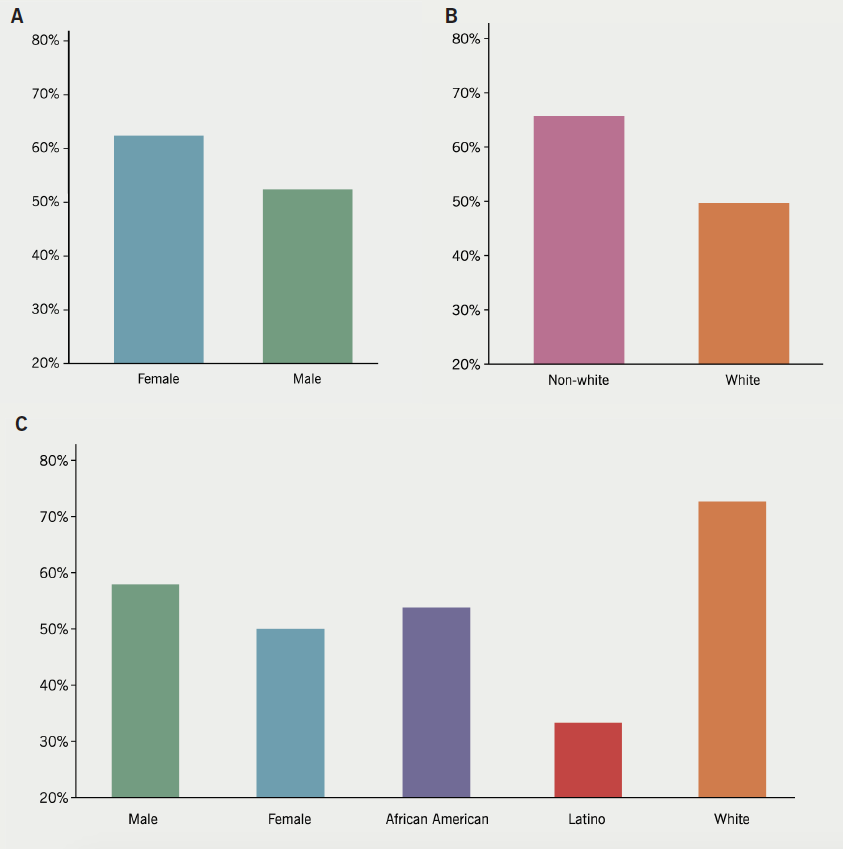
There were 355 unique patients who met criteria for inclusion in the study, with 206 male and 149 female patients. Of these patients, 201 were screened with PHQ2 or PHQ9 at least once between 2015 to 2018 (56.6%). Depression screening results are summarised in table 1 and figure 1. Males had a lower rate of PHQ screening than females (52.4% vs. 62.4%, p=0.061). Forty-one of the 201 screened patients had elevated PHQ scores (20.4%), and these results were discussed in the plans of 22 out of the 41 patients who screened positive (53.7%). By race, whites had the lowest screening rate (49.7%), followed by African American (61%), Latino (69.7%), and Asian (75%) patients. Patients with unknown race had a 43.8% screening rate. White patients had decreased screening rates versus non-white patients (49.7% vs. 65.7%, p=0.0036), though white patients who screened positive had a higher likelihood of a mention of depression screen results in their assessment and treatment plan when compared to non-white patients (72.7% vs. 42.9%, p=0.01). There are places like the rehab centers near Philadelphia that take care of even the mental well-being of patients that get admitted there.
Table 1. Depression screening results sorted by gender, race, and inclusion in management plan
style=”background-color: lightgrey; border-bottom: 2px solid rgb(050); padding: 5px;
| Patient results | Yes | No | Total |
|---|---|---|---|
| Depression screened | 201 | 154 | 355 |
| Screen result | Yes | No | Total |
| Positive screen | 41 | 160 | 201 |
| Depression mentioned in plan | 22 | 19 | 41 |
| Positive screen | Included in treatment plan | Not included in plan | Total |
| Male | 11 | 8 | 19 |
| Female | 11 | 11 | 22 |
| African American | 7 | 6 | 13 |
| Latino | 5 | 10 | 15 |
| White | 8 | 3 | 11 |
| Unknown | 2 | 0 | 2 |
Discussion
Though depression is associated with significantly increased mortality risk in patients with CAD, depression and mental healthcare is not consistently emphasised in patients with stable cardiac disease. A large study performed with 24,137 patients at the Intermountain Heart Institute found that depression was the strongest risk factor for mortality prediction in patients with CAD, and recommended the use of depression screening as part of follow-up care in patients with CAD.5 The strong negative impact of depression on outcomes in CAD patients suggests the need for increased provider education, as well as improved rates of mental health screening and treatment, as part of comprehensive care in patients with cardiac disease. In addition to demonstrating the need for increased provider education and follow-up on depression screening in CAD patients, we found a trend toward disparity in depression screening by gender, as well as statistically significant variation in screening by race. This may be due to provider counter-transference, bias regarding the perceived appearance of a depressed patient, or difference in rates of specialist treatment for depressive symptoms. Additionally, white patients who screened positive had the highest likelihood of the screen being mentioned in their assessment and plan, with statistically significant higher likelihood compared with non-white patients. As patients with depressive symptoms and CAD have doubled mortality, this may represent a critical opportunity to ameliorate outcomes disparities in heart disease, especially in developing countries and healthcare delivery settings with few available resources.
This study is limited by its use of depression screening and assessment by primary care providers only. While PHQ screening is sensitive and specific for depression, patients often have dynamic PHQ scores, which may have self-limited elevation and, therefore, not require treatment. Results of this chart review are currently being used to drive changes in the mechanism for positive depression screen reporting at the ambulatory clinic site.
Key messages
- Depressive symptoms double mortality in coronary artery disease
- We found that 57% of patients with coronary artery disease were screened for depression at primary care visits in the outpatient setting
- White patients had the lowest screening rate, but the highest probability of mention of a positive screen, if present, in their treatment plan
- Depression screening for patients with coronary artery disease may present an opportunity to improve health outcomes disparities
Conflicts of interest
None declared.
Funding
None.
Study approval and consent
This study was approved as a retrospective analysis by the institutional review board for medical research at Northwell Health. It used retrospective data that was routinely collected and did not require additional informed consent.
References
1. Huffman JC, Celano CM, Beach SR, Motiwala SR, Januzzi JL. Depression and cardiac disease: epidemiology, mechanisms, and diagnosis. Cardiovasc Psychiatry Neurol 2013;2013:695925. https://doi.org/10.1155/2013/695925
2. Celano CM, Huffman JC. Depression and cardiac disease: a review. Cardiol Rev 2011;19:130–42. https://doi.org/10.1097/CRD.0b013e31820e8106
3. Mitchell AJ, Yadegarfar M, Gill J, Stubbs B. Case finding and screening clinical utility of the Patient Health Questionnaire (PHQ-9 and PHQ-2) for depression in primary care: a diagnostic meta-analysis of 40 studies. BJPsych Open 2016;2:127–38. https://doi.org/10.1192/bjpo.bp.115.001685
4. Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med 2001;16:606–13. https://doi.org/10.1046/j.1525-1497.2001.016009606.x
5. May HT, Horne BD, Knight S et al. The association of depression at any time to the risk of death following coronary artery disease diagnosis. Eur Heart J Qual Care Clin Outcomes 2017;3:296–302. https://doi.org/10.1093/ehjqcco/qcx017
