Introduction to the steering committee

Dr Abhishek Joshi, Dr Jim Moore, Ms Helen Williams
Conflicts of interest
The steering committe received speaking and consultation fees from Bayer plc.
MRC provides consultancy advice to Abbott, AstraZeneca, Bayer, Boston Scientific, Medtronic, Novartis, Roche Diagnostics and Servier.
MF has received speaker honoraria, conference sponsorship, unrestricted educational grants, and/or attended meetings sponsored by AstraZeneca, Bayer, Boehringer Ingelheim, Bristol Myers Squibb, Medtronic, Novartis, Pfizer, Roche, Sanofi-Aventis, and Servier.
AJ: none declared.
JJ is CEO of Thrombosis UK, which has received unrestricted educational grants from Bayer plc and other pharmaceutical companies for educational meetings.
JM has received honoraria from Amgen, AstraZeneca, Bayer, Boehringer Ingelheim and Novartis for various activities including attending and participating in educational events and advisory boards.
HW has received speaker fees and / or attended advisory boards for Amgen, Astra Zeneca, Bayer, Boehringer Ingelheim, BMS / Pfizer, Daiichi Sankyo and Novartis.
Steering committee funding
The steering committee meeting and report development was funded by Bayer plc.
Foreword
The past year has been challenging for all of us in the NHS.
When looking at the impact of the pandemic on the field of cardiovascular disease (CVD), reduced screening opportunities and cancelled clinics and procedures have caused widespread disruption.
However, there is a positive side. The pandemic has provided a unique opportunity for restructuring CVD services in England. Telemedicine, home monitoring and integration of primary and secondary care are not new concepts in CVD care, yet their increased use over the recent months has served us and our patients well. In fact, the increased uptake of these systems and processes during lockdown have been effective, more convenient and appropriate for the digitally connected age in which we live.
With the persistence of the virus, social distancing restrictions still in place, a stretched health service and possibly long-lasting changes in patient behaviour, we must embrace these changes to our practice moving forward. It is important that we do what we can amidst the disruption caused by the pandemic to maintain good CVD care. Despite the seriousness of our current situation, CVD still remains the single biggest area where the NHS can save lives over the next 10 years as identified by the NHS Long Term Plan.
In May 2020, alongside fellow clinicians and advocates for CVD care, we discussed our beliefs of how best to adapt CVD services to the ‘new norm’, without changing the level of care provided. Whilst there is a focus on primary and secondary care and the patient, in line with the make-up of the committee, these recommendations will require engagement from all parties; patients, healthcare professionals (HCPs) and payers.
Fundamentally, we can all do our part to keep CVD care on the political agenda and keep saving lives.
Professor Martin Cowie
How COVID-19 changed cardiovascular disease care
The COVID-19 pandemic has significantly affected CVD care in England and created exceptional challenges for the NHS, clinical community and patients.1 The scale of the pandemic’s impact and the threat of further national and local spikes in infection rates suggest that it is unlikely that CVD services will return to pre-pandemic levels for some time.
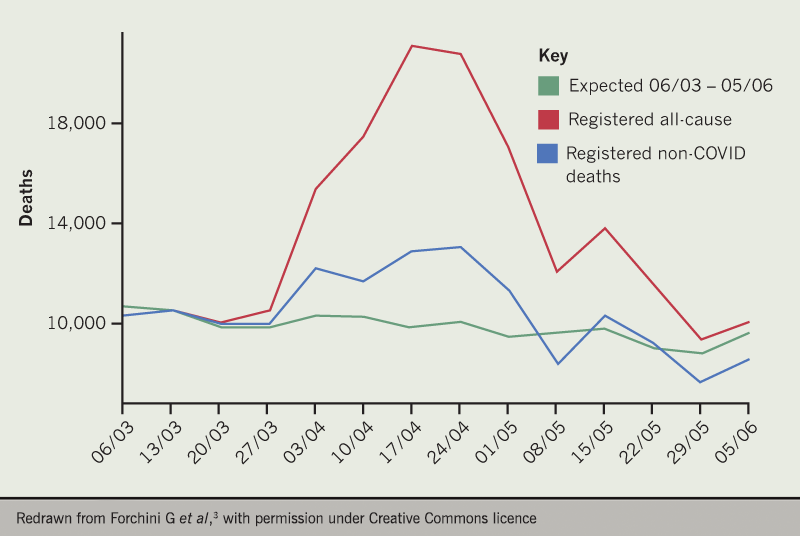
Exceptional times require exceptional measures. The first national lockdown prevented access to primary care for some, with subsequent delays in the identification of disease and out-patient referrals.1 Hospitals and emergency departments have been almost closed to non-COVID-19 patients for many months, resulting in a backlog of thousands of CVD patients and cancelled procedures.1,2 The knock-on impact of these provisions is sobering, with estimations of non-COVID-19 excess deaths during the height of the pandemic at almost 9,000 (figure 1),3 of which over 2,000 were acute cardiovascular deaths.4
We are now in the next phase – the so-called ‘new norm’. However, there are several challenges that we must overcome first.
Services must return with social distancing in place to minimise the risk of further COVID-19 outbreaks,5 subsequently reducing important physical interaction between doctor and patient. In parallel, the NHS and ancillary workforces are exhausted, and resources are stretched. Recent figures place the ‘hidden NHS waiting list’ for follow ups of any health condition at 15.3 million, which will undoubtedly put considerable strain across all healthcare services.6
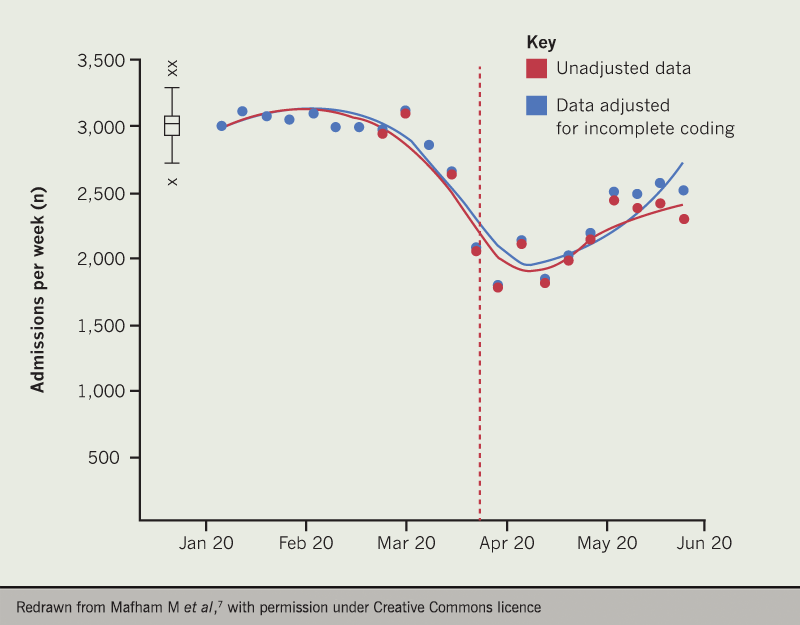
Patient factors are also a key priority. Patients’ behaviour has changed – anxieties towards the virus remain.2 During February and March, there was a 40% reduction in hospital admissions for acute coronary syndrome when compared to the same period in 2019, which is likely to lead to an increase in out-of-hospital deaths and long-term complications of myocardial infarction (figure 2).7 Further, messaging around COVID-19 has been confusing and unclear, particularly for CVD patients who are unsure whether they are at greater risk of infection or worse outcomes. Many people have been told to self-manage and monitor their conditions without instruction. Importantly, people are unsure when to seek help from their doctor.
While ‘good care’ for CVD should not change, the NHS will continue to deliver its Long Term Plan. Launched in 2019, the Long Term Plan identifies CVD as a clinical priority and the single biggest area where the NHS can save lives with the goal to prevent over 150,000 heart attacks, strokes and vascular dementia cases in the next decade.8 However, we now live in a different world. As the world shifts in response to the virus, the way CVD care is delivered should be adapted.
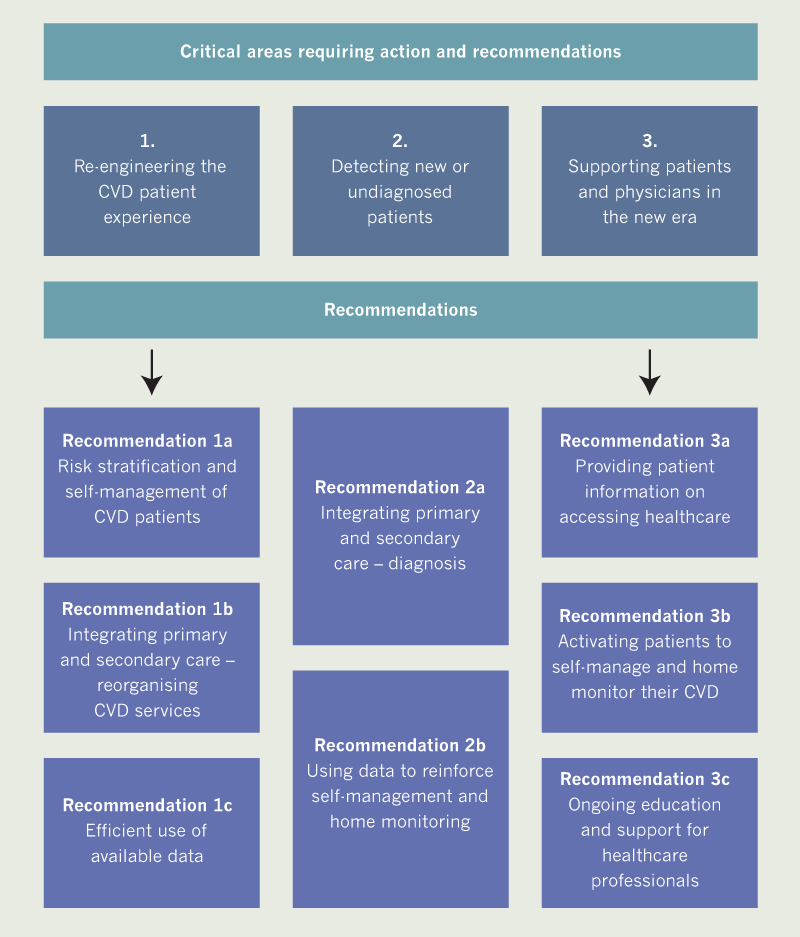
This thought piece identifies three critical areas where CVD services have been impacted by COVID-19 and therefore must adapt to operate in the ‘new norm’. The steering committee offer recommendations for how primary and secondary care can support these changes, while keeping the patient at the centre of planning (see figure 3).
1. Re-engineering the CVD patient experience – providing optimal care for established CVD patients

Remote consultations have played a vital role during the pandemic. However, they are not necessarily new. Some primary and secondary care clinicians were already regularly using virtual appointments pre-pandemic.1,9 Further, the NHS Topol report,10 published in February 2019, called for digital healthcare technologies to be ‘a new means of addressing the big healthcare challenges of the 21st century’.10 Clearly, the accelerated implementation of these systems are driving innovation in care, rather than being a temporary solution. There is now an opportunity in England to embed the successful services, and redesign those that were flagging.
With non-COVID-19 care on pause for months, the NHS must catch up. A lower estimate of 28,000 heart procedures have been delayed during the pandemic.2 This presents a significant bottleneck for secondary care, who must focus on procedures that only they can perform. Primary care may need to take more responsibility in dealing with CVD cases to ease the strain on their cardiologist colleagues.
While the benefit and efficiency of telemedicine are clear, human factors remain important. NHS staff are tired because of the pandemic, and remote consultations present unique challenges. Without visual cues and a physical presence in the room, telephone triage can be fatiguing and prevent fostering of trust and empathy.9 Moreover, there are fears that expanding digital health technologies may widen health inequality gaps for those with a lower digital literacy, without access to a smart phone or broadband internet9 or even for certain demographics and cultures.
More detail on recommendations made by the steering committee for ‘Re-engineering the CVD patient experience’ are outlined in algorithms, case studies and key messages 1a–c.
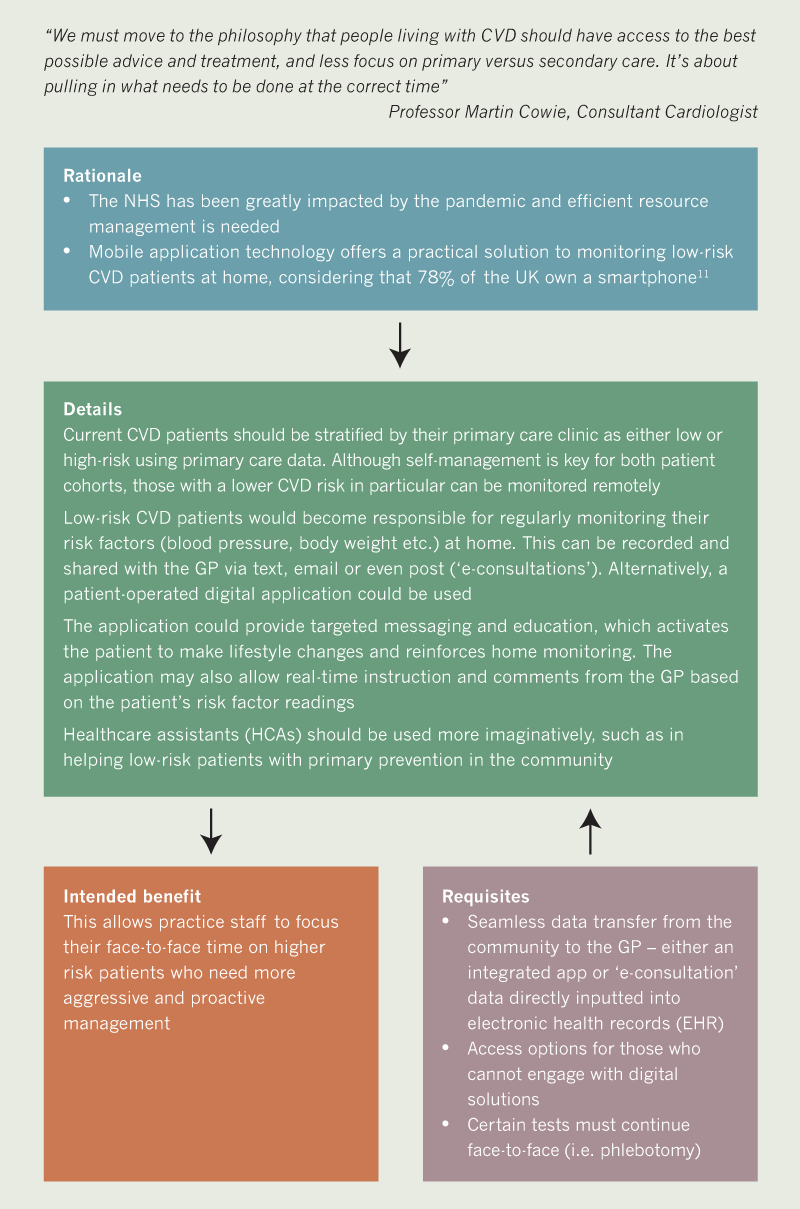
Key messages 1a
- Cardiovascular disease patients should be risk stratified, with a focus on remote monitoring for low-risk patients
- Home monitoring equipment and data entry could allow GPs to supervise their patients remotely
- This may allow greater focus of resources on high-risk patients
1st case study 1a: In practice example of self-management – the blood pressure monitoring revolution
Provided by Dr Jim Moore, General Practitioner with a Special Interest

This patient case study discusses the use of home blood pressure monitoring (HBPM) for monitoring hypertension, as outlined in the National Institute for Health and Care Excellence (NICE) 2019 guideline ‘Hypertension in adults’,12 and deployed during the COVID-19 pandemic.
A 45-year-old male patient with type 2 diabetes was discharged from hospital, following treatment for a myocardial infarction and newly diagnosed hypertension, shortly before the pandemic began. He was due for a review appointment at his local primary care practice, which lockdown prevented. The practice was aware of the importance of having this patient’s blood pressure well controlled and without delay. They needed up-to-date blood pressure data and had a virtual discussion with him around HBPM.
The patient purchased a validated blood pressure machine online after reading guidance from the British and Irish Hypertension Society website. The practice signposted online HBPM educational resources, and the patient downloaded an HBPM form from the practice website which he subsequently completed with one week’s readings. The form was then emailed back to the practice for review and action.
HBPM facilitated virtual discussion between the patient and his GP, who was able to alter his management appropriately in the middle of a pandemic, all without a face-to-face consultation. Dr Moore commented: “One of the benefits of newer technologies is that they frequently increase the patient’s involvement in and responsibility for managing their own healthcare”.
2nd case study 1a: In practice example of risk stratification – UCLPartners COVID-19 recovery hypertension pathway
Provided by Helen Williams, Consultant Pharmacist

Adaptation of pathways is an integral part of the NHS’s response to the COVID-19 pandemic. UCLPartners have designed support packages to help primary care “build new ways to provide proactive care and prevent exacerbations of long-term conditions”. The hypertension support package provides a guide for clinicians (GPs, nurses and clinical pharmacists) when reviewing patients with suboptimal blood pressure control, augmented by healthcare assistants (HCAs) and non-clinical staff in low-risk cases. Reviews are virtual by default and home blood pressure monitoring (HBPM) is recommended where possible.
Patients should be risk stratified based on their already available clinic blood pressure results and verified using home blood pressure results.
For example, a person under 80-years-old with a clinic blood pressure <140/90 mmHg / home blood pressure <135/85 mmHg could be managed by an appropriately trained HCA or other staff role. The HCA / staff role, using protocol, would remotely support self-management and any necessary behaviour changes; check medication and refer for pharmacist support if issues are identified, such as adherence, side effects or patient concerns; advise when to submit home blood pressure readings / when to seek further help and refer to GP if needed.
In contrast, high priority cases i.e. clinic blood pressure ≥180/120 mmHg / home blood pressure ≥170/115 mmHg should be reviewed by the prescribing primary care clinician, which includes investigation of clinical parameters, medication review and gaining specialist advice from secondary care if appropriate. In appropriate cases, follow-up reviews can be conducted by an HCA or staff role.
A fundamental aspect of the pathway is HBPM. Where patients do not own HBPM equipment, they will be advised to buy endorsed machines or directed to local schemes where they may be available free of charge. Face-to-face blood pressure monitoring should be available in community settings to reduce health inequality.
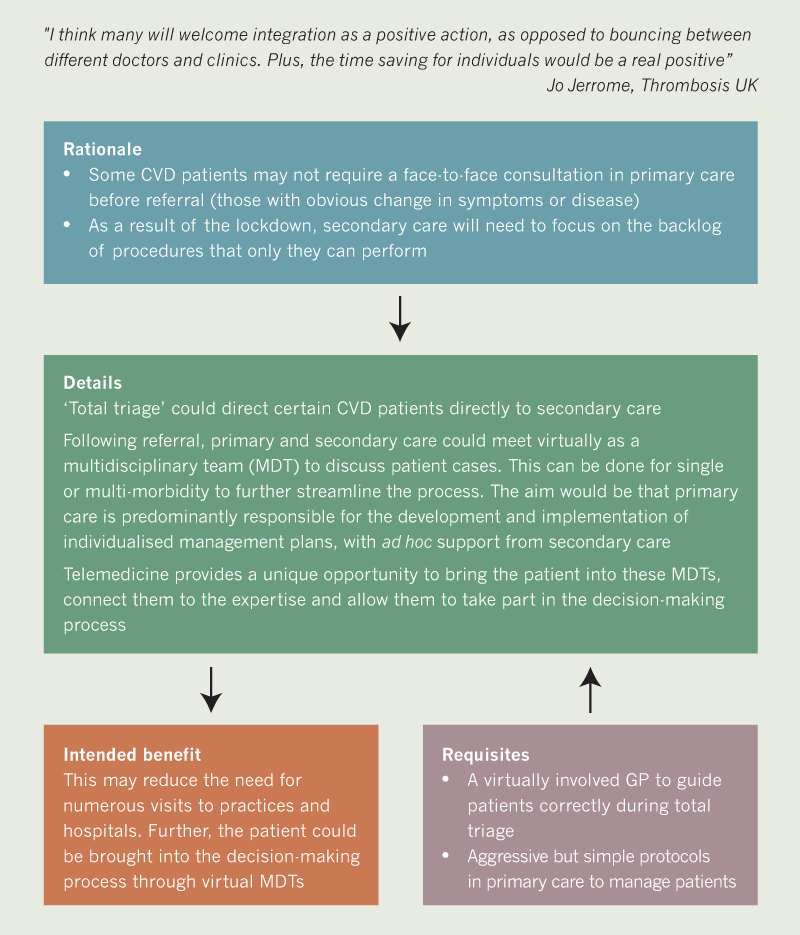
Key messages 1b
- Patients are ‘totally triaged’ directly to secondary care without an unnecessary primary care consultation
- Virtual multidisciplinary team meetings with primary and secondary care and the patient are held to decide on a management plan to be conducted in primary care
- Patients are kept at home and potentially brought into the decision-making process
Case study 1b: A patient case study of MDTs – “we were all singing from the same hymn sheet”
Provided by Jo Jerrome, Thrombosis UK

A 60-year-old woman, Carol, with multiple co-morbidities requiring regular monitoring shielded through much of the lockdown. Before the pandemic, she would regularly attend her GP and multiple clinics at the local hospital. In July 2020, a virtual meeting was organised so she could talk with her multi-disciplinary healthcare team.
“It was a joy, it felt so much better. Everyone spoke to each other in one meeting and not only did I not have to repeat myself many times – or travel repeatedly for appointments and then wait – but I could correct any gaps or misunderstandings about my medical history and medication. All four health professionals also said how good it was. Even the GP called me the next day and said it was the most useful half-hour spent on my care in 10 years. I felt really good when I left that meeting – we were all singing from the same hymn sheet!”
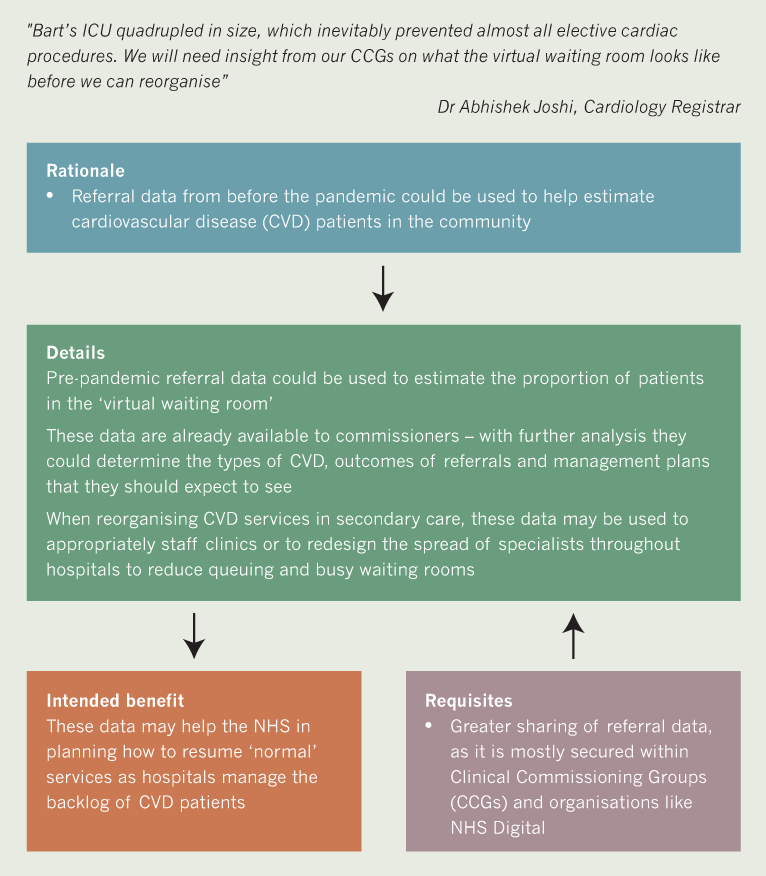
Key messages 1c
- Pre-pandemic cardiovascular disease (CVD) referral data could be used to estimate the amount and type of CVD patients in the community
- This could help to efficiently reshape CVD services in secondary care
2. Detecting new or undiagnosed patients – ensuring opportunities for CVD detection are not missed

In-clinic primary care appointments dropped from 70% to 23% within weeks of pandemic provisions being actioned.9 Patient mentality has changed – concerns of COVID-19 cross-infection in a healthcare environment and unnecessary usage of NHS resources have kept people at home, sometimes inappropriately.2 Although the proportion of face-to-face appointments in primary care may increase, they are unlikely to return to previous levels.9 This reduction in tangible contact between primary care and patients is likely to limit opportunities to screen those at risk of CVD.
Conditions such as atrial fibrillation (AF) and hypertension are typically detected at routine health checks or during an unrelated appointment / clinic. Many of these appointments have been cancelled or postponed, and virtual consultations are not conducive to screening for certain CVD risk factors and conditions. However, the expansion of winter flu clinics13 may offer increased opportunities for pulse checks to support AF detection in at-risk groups, such as the elderly or those with other conditions, like diabetes or asthma.14
Home monitoring of CVD risk factors for new and undiagnosed patients will be an essential requirement in the ‘new norm’ of CVD care. Remote monitoring and the digital solutions to facilitate monitoring is a rapidly growing landscape – many devices and applications are available at varying costs.9 It is essential that patients are guided to reliable tools, correctly educated on how to use them and that the expansion of home monitoring does not widen health inequality gaps.
More detail on recommendations made by the steering committee for ‘Detecting new or undiagnosed patients’ are shown in algorithms and key messages 2a–b.

Key messages 2a
- Patients should be treated as consumers – a quick diagnosis, access to treatment options and an effective therapy
- Diagnostic tests could be combined to streamline the process. Secondary care can provide advice to GPs without a physical appointment
- Time to diagnosis and treatment could be reduced, and more new CVD patients managed in primary care
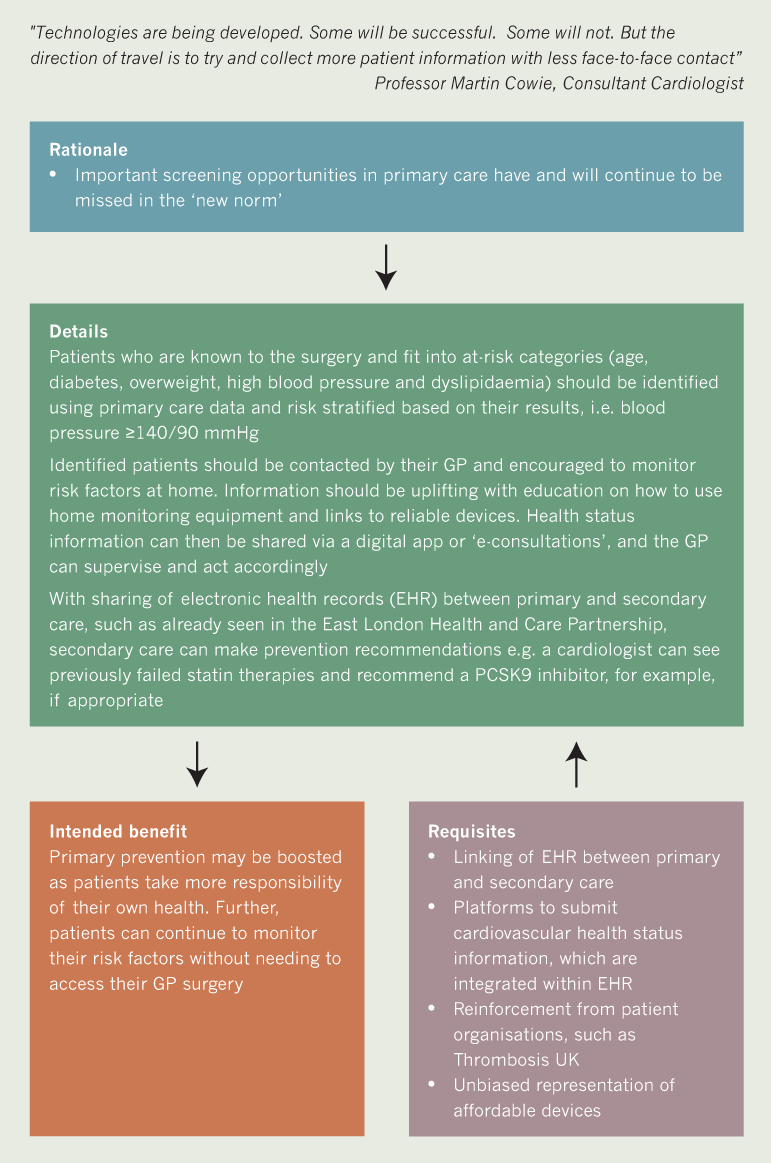

Key messages 2b
- ‘Pre-ill’ patients are identified and targeted with self-management and home monitoring messaging
- Secondary care can provide input through access to primary care data
- Primary prevention and home monitoring are boosted, while keeping people out of the clinic
3. Supporting patients and physicians in the new era
The COVID-19 pandemic has changed the healthcare landscape. Therefore, it is important that channels of communication are open to continually reassure patients that they will be safe and receive the same standard of care as before the pandemic.
The move to virtual consultations should help to streamline healthcare access by supporting the ‘worried but well’ patients with home monitoring and HCP supervision, and allow resources to be focused on the ‘unaware and unwell’ patients that are hidden in the community. However, HCPs should accept that telemedicine does not work for every patient. The less digitally literate and those without digital technology may be further marginalised.9 There should be a balance between face-to-face and virtual consultations so that no patient is left behind, and this must be underpinned by clear dialogue between the patient and HCP.
There are also concerns that important patient-HCP conversations have been delayed or confused during the pandemic. For example, professional guidance recommended the transition of eligible non-valvular AF and venous thromboembolism (VTE) patients from vitamin K antagonists (VKA) to direct oral anticoagulants (DOACs).15 Some patients were concerned by this change of protocol as there was little time for discussion, particularly for those who were previously told they were not suitable for a DOAC. Further, the capacity of community international normalised ratio (INR) testing was uncertain for those who were unsuitable for an anticoagulation switch.
It is equally important that HCPs are supported, especially those who do not have a CVD specialism. There may be cultural resistance to the increased use of telemedicine. Research suggests that telephone triage actually increases workload,16 and the loss of visual cues with the patient can be frustrating. HCPs need to be assured that current and ongoing changes are to adapt the delivery of care, not to change care itself.
More detail on recommendations made by the steering committee for ‘Supporting patients and physicians in the new era’ are shown in algorithms, case studies and key messages 3a–c.
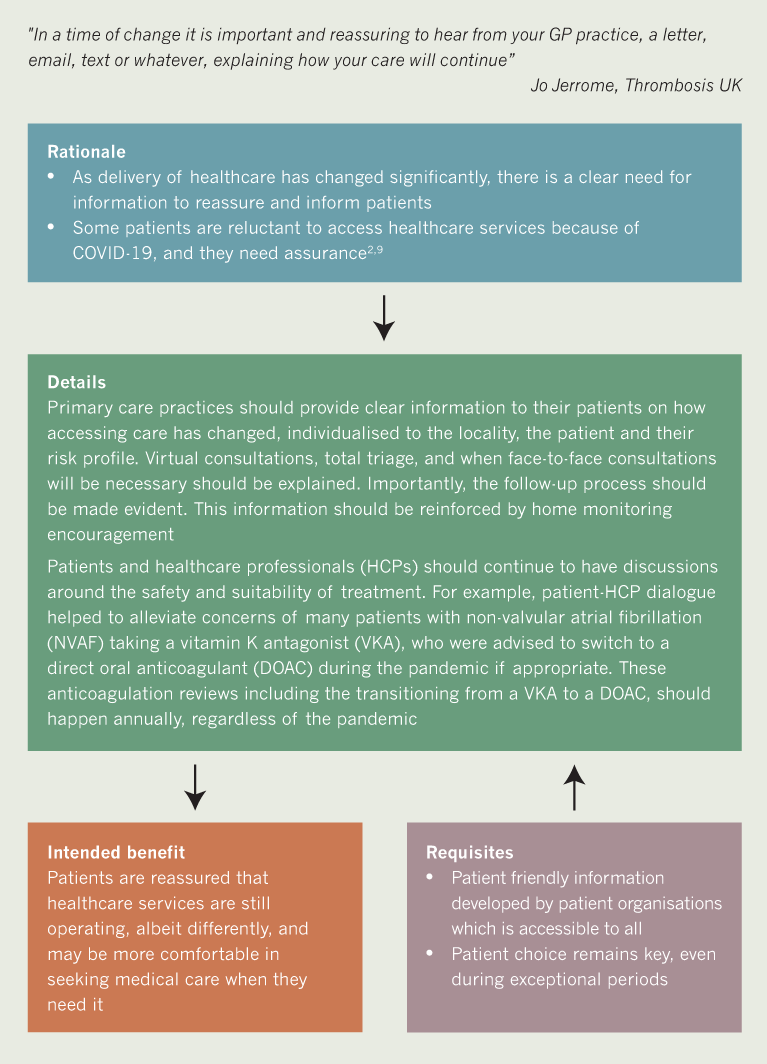
Key messages 3a
- Patients should be clearly informed by their GP on how they can access healthcare in the ‘new norm’
- Patient choice is important in any treatment / management discussions
- Patients may feel better equipped and more comfortable to seek medical assistance when they need it
Case study 3a: In practice example of frequent patient concerns at consultation
Provided by Jo Jerrome, Thrombosis UK

Before a consultation: The patient should be encouraged to think about any important changes, symptoms and concerns since their previous appointment:
- It can be useful for the patient to collate these in a diary or written summary, with key questions included.
During a consultation: The patient should know there are no irrelevant questions. Key questions include:
- What can I expect in terms of recovery/treatment?
- What can I do to help?
After a consultation: It should become routine to include:
- Who to contact if you have any problems
- What will happen next?
- In what time frame you should expect to hear back from us
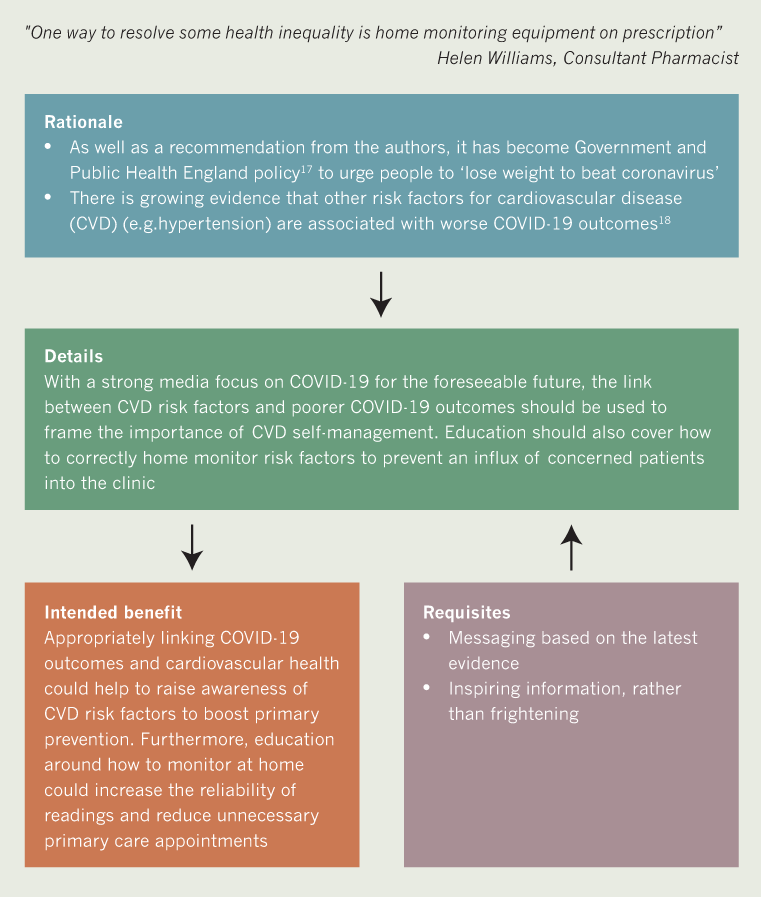
Key messages 3b
- Linking risk factors for cardiovascular disease (CVD) and COVID-19 outcomes could help frame primary prevention and home monitoring
- Patients must receive education to home monitor correctly
- Raising awareness of CVD risk factors and reinforcing home monitoring could boost primary prevention
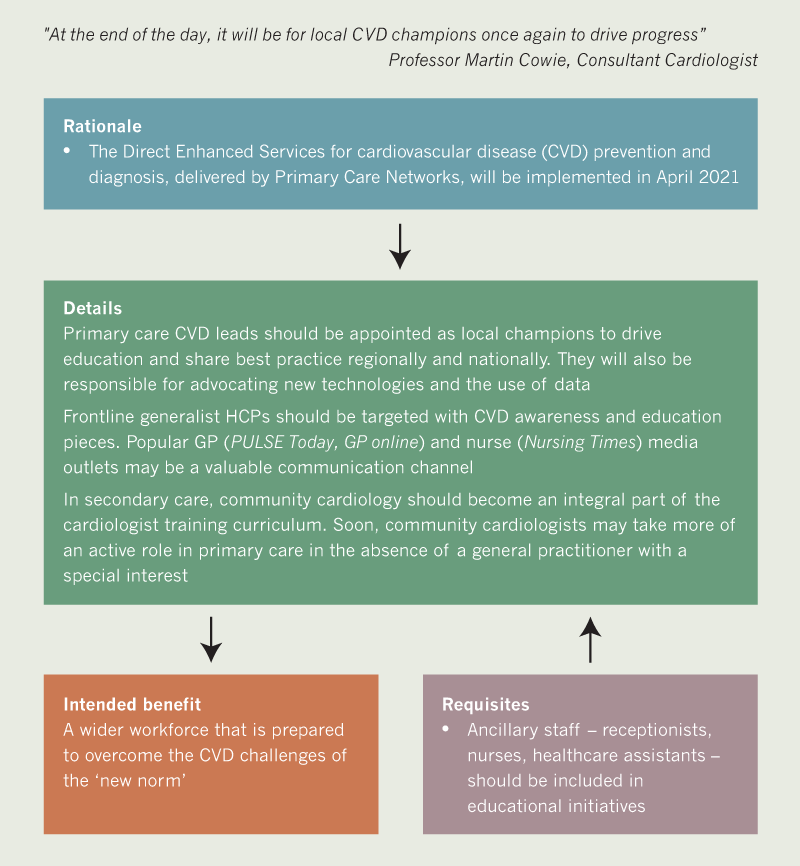

Key messages 3c
- Cardiovascular disease (CVD) education should be reinforced by local CVD champions and targeted messaging in generalist media
- Community cardiology should become a central aspect of the cardiologist training curriculum
- CVD education should encompass all frontline staff, not just clinicians
A call to action: now, more than ever, we need to keep CVD on the political agenda
The disruption caused by the COVID-19 pandemic has had a significant impact on CVD patient care. Clinics and procedures have been cancelled or delayed and screening opportunities missed. As the NHS deals with the huge backlog of patients, there is an urgent requirement to focus resources on two cohorts of patient – those with established disease who are already at risk of poor COVID-19 outcomes and those with undetected disease and risk factors. Their cardiovascular experience should not be further affected by a lack of access to care and available treatments.
CVD remains one of the leading causes of death in England. With the challenges posed by the pandemic and the possibility of further outbreaks, it is more important than ever to keep CVD on the political agenda. In order to do so, everyone has a role to play. Patients, HCPs and policy makers on a national basis must be aware and educated on the importance of detection, prevention and management of CVD. HCPs in particular must help to drive the innovation and implementation of CVD services.
We now have a unique opportunity to use the disruption of COVID-19 to accelerate the modernisation of our healthcare system. However, it is key that the new ways of delivering CVD care do not widen the already present health and digital inequality gaps. The fundamental aim is to update services, maintain high quality care and ultimately, reduce CV-related morbidity and mortality in England in the ‘new norm’.
Further useful resources
British Cardiovascular Society. The future of cardiology report. Available at: https://www.britishcardiovascularsociety.org/news/the-future-of-cardiology [last accessed 13th November 2020].
Royal College of General Practitioners. Policy and campaigns: general practice post-Covid. Available at: https://www.rcgp.org.uk/policy/general-practice-post-covid.aspx [last accessed 13th November 2020].
References
1. British Cardiovascular Society. The future of cardiology. A Paper Produced by the British Cardiovascular Society Working Group on The Future of Cardiology, August 2020. Available at: https://www.britishcardiovascularsociety.org/news/the-future-of-cardiology [accessed August 2020].
2. British Heart Foundation. Nearly half of heart patients find it harder to get medical treatment in lockdown. News report 5th June 2020. Available at: https://www.bhf.org.uk/what-we-do/news-from-the-bhf/news-archive/2020/june/half-heart-patients-harder-get-medical-treatment-lockdown [accessed August 2020].
3. Forchini G, Lochen A, Hallet T, et al. Imperial College COVID-19 response team. Report 28: Excess non-COVID-19 deaths in England and Wales between 29th February and 5th June 2020. Imperial College London (18-06-2020). https://doi.org/10.25561/79984
4. Wu J, Mamas M A, Mohamed M O, et al. Place and causes of acute cardiovascular mortality during the COVID-19 pandemic. Heart 2020, published online first 28th September 2020. http://dx.doi.org/10.1136/heartjnl-2020-317912
5. National Health Service. Using the NHS and other health services during coronavirus. 2020. Available at: https://www.nhs.uk/conditions/coronavirus-covid-19/social-distancing/using-the-nhs-and-other-health-services/ [accessed August 2020].
6. The Times. Coronavirus: NHS data shows 15m on ‘hidden waiting list’. News report August 27th 2020. Available at: https://www.thetimes.co.uk/article/coronavirus-nhs-data-shows-15m-on-hidden-waiting-list-w250vxvz6 [accessed August 2020].
7. Mafham M, Spata E, Goldacre R, Gair D, Curnow P, Bray M. COVID-19 pandemic and admission rates for and management of acute coronary syndromes in England. The Lancet. 2020;396:381–9. https://doi.org/10.1016/S0140-6736(20)31356-8
8. National Health Service. NHS long term plan: cardiovascular disease. Chapter 3: Further progress on care quality and outcomes. 2019. Available at: https://www.longtermplan.nhs.uk/online-version/chapter-3-further-progress-on-care-quality-and-outcomes/better-care-for-major-health-conditions/cardiovascular-disease/ [last accessed August 2020].
9. Royal College of General Practitioners. General practice in the post-Covid world: challenges and opportunities for general practice. 2020. Available at: https://www.rcgp.org.uk/-/media/Files/News/2020/general-practice-post-covid-rcgp.ashx?la=en [accessed August 2020].
10. Topol E. The Topol Review: Preparing the healthcare workforce to deliver the digital future. An independent review on behalf of the Secretary of State for Health and Social Care, February 2019. Available at: https://topol.hee.nhs.uk/ [last accessed 13th November 2020].
11. Ofcom. A decade of digital dependency. News report, 2nd August 2018. Available at: https://www.ofcom.org.uk/about-ofcom/latest/features-and-news/decade-of-digital-dependency [last accessed 13th November 2020].
12. National Institute for Health and Care Excellence. Hypertension in adults: diagnosis and management. NICE guideline [NG136], August 2019. Available at: https://www.nice.org.uk/guidance/ng136/chapter/Recommendations [last accessed 13th November 2020].
13. Department of Health & Social Care / Public Health England. The national flu immunisation programme 2020 to 2021 – update. 5th August 2020. Available at: https://www.england.nhs.uk/wp-content/uploads/2020/05/Letter_AnnualFlu_2020-21_20200805.pdf [last accessed 13th November 2020].
14. National Health Service. Health A to Z. Atrial fibrillation, 24th April 2018. Available at: https://www.nhs.uk/conditions/atrial-fibrillation/causes/ [last accessed 13th November 2020].
15. Royal Pharmaceutical Society/UKCPA/PCPA/PCCS. Guidance for the safe switching of warfarin to direct oral anticoagulants (DOACs) for patients with non-valvular AF and venous thromboembolism (DVT / PE) during the coronavirus pandemic. Published 26th March 2020. Available at: https://www.rpharms.com/Portals/0/RPS%20document%20library/Open%20access/Coronavirus/FINAL%20Guidance%20on%20safe%20switching%20of%20warfarin%20to%20DOAC%20COVID-19%20Mar%202020.pdf?ver=2020-03-26-180945-627 [last accessed 13th November 2020].
16. Campbell J, Fletcher E, Britten N, et al. Telephone triage for management of same-day consultation requests in general practice (the ESTEEM trial): a cluster-randomised controlled trial and cost-consequence analysis. The Lancet 2014;384:1859–68. https://doi.org/10.1016/S0140-6736(14)61058-8
17. Department of Health and Social Care. Press release: New obesity strategy unveiled as country urged to lose weight to beat coronavirus (COVID-19) and protect the NHS, 27th July 2020. Available at: https://www.gov.uk/government/news/new-obesity-strategy-unveiled-as-country-urged-to-lose-weight-to-beat-coronavirus-covid-19-and-protect-the-nhs [last accessed 13th November 2020].
18. Guan W, Liang W, Zhao Y, et al. Comorbidity and its impact on 1,590 patients with COVID-19 in China: a nationwide analysis. Eur Respir J 2020;55(5):2000547. https://doi.org/10.1183/13993003.00547-2020

