Two cases of orthostatic hypotension associated with weight loss following cancer treatment are described. Conventional treatments for orthostatic hypotension proved ineffective. A hypothesis of association with skeletal muscle wasting is discussed.
Case one

A squamous cell carcinoma of the right tonsil was confirmed by biopsy in a 70-year-old man in July 2014. It was well encapsulated and subsequent cervical lymph node biopsies showed no tumour spread. In August and September 2014, the patient had intense radiotherapy to the tonsil and surrounding areas.
Following radiotherapy, the patient experienced profound lethargy and soreness of the mouth to such an extent that despite attempts at high-calorie supplement feeding he continued to lose weight. By the end of October, he had lost 10 kg, began to develop dizziness on standing and marked orthostatic hypotension was observed. He had stopped antihypertensive drugs, amlodipine and candesartan, several months previously at the start of his radiotherapy. Sitting blood pressure (BP) was 125/85 mmHg with standing BP 90/60 mmHg. Symptoms worsened and by December he had lost a total of 16 kg and was admitted for re-feeding by nasogastric tube, at which time standing BP had fallen to 80/55 mmHg. At all times the orthostatic response was accompanied by a normal rise in heart rate and there were no other features of autonomic impairment. Brain magnetic resonance imaging (MRI) was normal.
Nasogastric feeding continued for about four weeks, followed by oral feeding with high-calorie protein supplements. In January, the following was noted: sitting BP 120/80 mmHg, pulse 70 bpm; standing BP 80/60 mmHg, pulse 84 bpm; repeat standing BP following 30 minutes walking 125/94 mmHg, pulse 98 bpm.
By the end of February, weight had risen by 5 kg and orthostatic symptoms had improved. Sitting BP 125/85 mmHg, standing BP 100/75 mmHg. With a further weight gain of an additional 5 kg, sitting BP 135/82 mmHg, standing BP 126/70 mmHg.
Case two
A 46 year old female was diagnosed with mild hypertension in 2015 and treated with candesartan and amlodipine with good BP control. The following year she developed lung cancer, which was treated by surgery and three courses of chemotherapy. Over a period of 12 weeks, owing to extreme nausea and anorexia, she lost approximately 16 kg in weight and this was associated with profound symptoms of orthostatic hypotension. Her previous antihypertensive drugs had been withdrawn. She was treated with midodrine and fludrocortisone with no improvement in her symptoms. There were no other signs of autonomic impairment. With gradual resolution of her nausea and anorexia her calorie intake increased and she regained most of her weight over a period of 12 weeks. At the end of this period, her postural symptoms had resolved. Over the following three months her BP rose and she was restarted on antihypertensive drugs.
Discussion
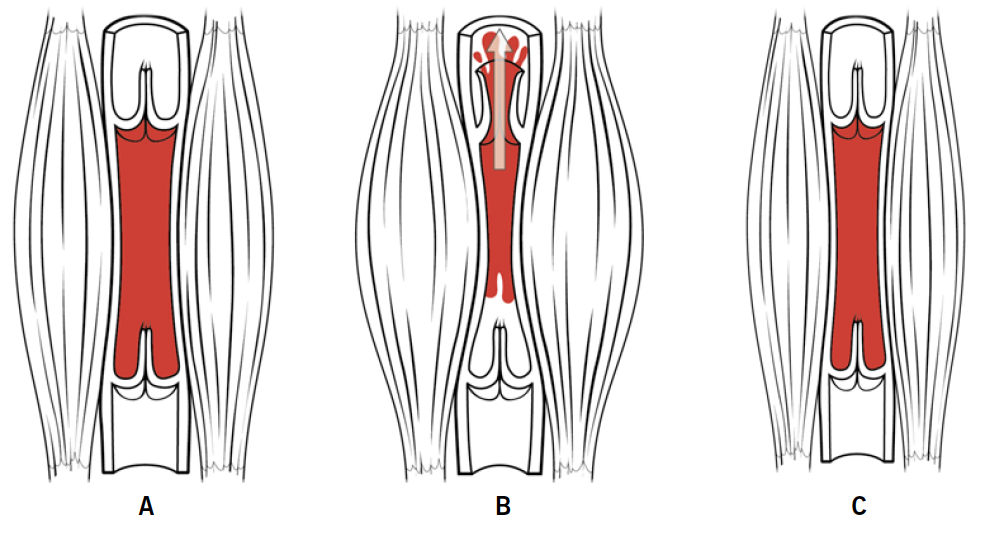
The explanation for the orthostatic hypotension is of interest. The unusual feature in the first case was that mild exercise corrected the postural fall in pressure, which would not occur if there was an underlying autonomic defect. Pituitary insufficiency was eliminated in this case by normal pituitary function tests including a synacthen test. The hypothesis in both cases is that the fall in pressure on standing is due to profound and rapid weight loss associated with loss of skeletal muscle bulk in the legs and gluteal regions, which impairs the venous return to the right atrium (figure 1). In the first case, the correction of the postural fall in pressure by mild exercise, which would increase residual muscle tone, is strongly supportive of this hypothesis. With increasing weight gain and daily exercise, the postural fall in pressure gradually resolved, presumably accounted for by restoration of skeletal muscle tone and mass.
There are no prior reports of this phenomenon associated with muscle wasting. There are reports of orthostatic hypotension in astronauts returning from flights in space, which could be accounted for by prolonged skeletal muscle inactivity, and there are anecdotal reports of postural hypotension occurring following bariatric surgery, which is associated with substantial weight loss, and also in patients with anorexia nervosa for whom there could be several causes. Such a mechanism could partially explain orthostatic hypotension in patients with Ehlers Danlos Syndrome with postural tachycardia syndrome.
Treatment in both the above cases with fludrocortisone was ineffective, as was midodrine in the second case.
Conflicts of interest
None declared.
Funding
None.
Patient consent
The author was the first case. The second case has been anonymised and written consent for publication was not sought.
