We present the angiographic findings of a case of myocardial infarction associated with COVID-19 with a heavy burden of thrombus, despite only minor obstructive coronary disease.
Introduction
Myocarditis is a known complication of COVID-19, however, recently concerns have been raised regarding myocardial injury in the presence of a substantial coronary thrombus burden, in combination with atherosclerotic plaque.1,2 Widespread community transmission of COVID-19 has led to some presentations of myocardial infarction associated with active COVID-19 infection.1 We present the angiographic findings of such a case with a heavy burden of thrombus, despite only minor obstructive coronary disease.
Case presentation
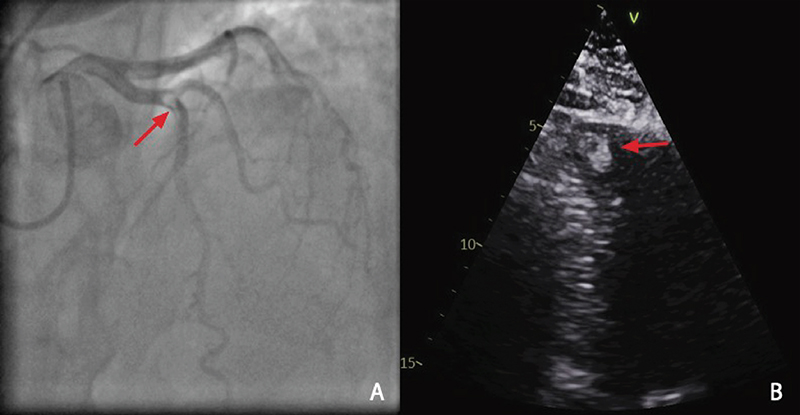
A 36-year-old man was admitted to a local hospital with respiratory failure secondary to COVID-19 pneumonia. Initial management included oxygen, dexamethasone and baricitinib. On day 14 of illness the patient developed severe chest pain associated with widespread dynamic ST-segment elevation and an elevated high-sensitivity troponin I (17,516 ng/L). He was transferred to a tertiary centre for cardiac evaluation. Cardiovascular risk factors included treated hypertension and obesity (body mass index [BMI] 34 kg/m2). Blood pressure was 145/95 mmHg and heart rate was 90 bpm in sinus rhythm. There were bilateral crackles in lower lung fields and 3 L/min of O2 therapy was required to maintain arterial saturations >90%. The initial clinical impression was myocarditis, however, given the severity of the patient’s chest pain, clinical suspicion for an acute coronary syndrome remained high. Coronary angiogram revealed a large filling defect (figure 1A) at the mid-vessel of the left anterior descending (LAD) at the first diagonal bifurcation. Dual antiplatelet therapy, heparin and tirofiban infusion were commenced. Furthermore, echocardiography performed the same day revealed a reduced left ventricular ejection fraction (LVEF) secondary to LAD territory hypokinesis and an associated apical left ventricular thrombus measuring 2.2 × 1.3 cm (figure 1B). Once established on anticoagulation the patient experienced no further chest pain and was discharged home on warfarin. The left ventricular thrombus was monitored for resolution in the community with serial transthoracic echocardiograms and the LVEF improved with guideline-directed heart failure therapy.
Discussion
The association between COVID-19 infection and acute coronary syndrome remains uncertain. Bangalore and colleagues presented findings of huge thrombosis with both obstructive and non-obstructive atherosclerotic plaque among patients with COVID-19 infection early in the pandemic.3 The cytokine storm triggered by a SARS-CoV-2 infection can be thrombogenic, resulting from increased platelet activation and decreased fibrinolysis.4,5 This process may further complicate the evaluation, and acute coronary syndrome does need consideration, even in those patients at a younger age with minimal risk factors.
Conclusion
Pericarditis or myopericarditis is a common complication during COVID-19 infection and can be difficult to distinguish from acute coronary syndrome. Unique factors in this case included: age, minimal cardiovascular risk factors, burden and location of coronary artery thrombus. These factors are atypical for a clinical presentation or angiographic findings of acute coronary syndrome and favour COVID-19 as a potential contributing factor. The implication of this includes consideration of standard protocol, particularly regarding anticoagulation and timing of invasive diagnostic assessment, as well as reinforcing the importance of registries to quantify the extent of the problem.
Key messages
- Pericarditis or myopericarditis is often the leading differential diagnosis in patients with diffuse ST-elevation, and chest pain during a COVID-19 infection
- Given the potentially pro-thrombotic state, proximal coronary artery lesions should be considered, as demonstrated by this case
Conflicts of interest
None declared.
Funding
None.
Patient consent
Appropriate written informed consent for interventional procedure and subsequent publication of patient’s clinical and angiographic imaging details was obtained. All attempts were made to ensure patient confidentiality was maintained.
Supplementary material
Videos are available from the author on request:
Video 1. Diagnostic angiogram (posteroanterior cranial view) showing a lesion in left anterior descending.
Video 2. Transthoracic echocardiography (off-axis apical four-chamber view) showing an echogenic density in the apex of the left ventricle.
References
1. Dominguez-Erquicia P, Dobarro D, Raposeiras-Roubín S, Bastos-Fernandez G, Iñiguez-Romo A. Multivessel coronary thrombosis in a patient with COVID-19 pneumonia. Eur Heart J 2020;41:2132. https://doi.org/10.1093/eurheartj/ehaa393
2. Tedeschi D, Rizzi A, Biscaglia S, Tumscitz C. Acute myocardial infarction and large coronary thrombosis in a patient with COVID‐19. Catheter Cardiovasc Interv 2021;97:272–7. https://doi.org/10.1002/ccd.29179
3. Bangalore S, Sharma A, Slotwiner A et al. ST-segment elevation in patients with Covid-19 – a case series. N Engl J Med 2020;382:2478–80. https://doi.org/10.1056/NEJMc2009020
4. Loo J, Spittle DA, Newnham M. COVID-19, immunothrombosis and venous thromboembolism: biological mechanisms. Thorax 2021;76:412–20. https://doi.org/10.1136/thoraxjnl-2020-216243
5. Kermani-Alghoraishi M. A review of coronary artery thrombosis: a new challenging finding in COVID-19 patients and ST-elevation myocardial infarction. Curr Probl Cardiol 2021;46:100744. https://doi.org/10.1016/j.cpcardiol.2020.100744
