Clinical trials and observational studies have demonstrated that long-term systolic blood pressure variability derived from repeated measurements of visit-to-visit clinic blood pressure is an important predictor of cardiovascular outcomes, independent of average levels of systolic pressure. Even in patients with well-controlled blood pressure (<140/90 mmHg), high systolic blood pressure variability confers an increased risk of cardiovascular events. Systolic blood pressure variability is currently derived from several measurements of visit-to-visit clinic blood pressure and expressed as the standard deviation of systolic pressure. Values in excess of 12 are indicative of high systolic blood pressure variability. Ongoing studies aim to determine whether home blood pressure monitoring may be an alternative way of measuring blood pressure variability. Evidence from several clinical trials shows that long-acting calcium-channel blockers, such as amlodipine, and thiazide-like diuretics are the only antihypertensive drugs that reduce long-term systolic blood pressure variability, and should be used preferentially in patients with high variability.
Introduction

Throughout history, blood pressure has played an important role in medicine, especially in predicting and assessing risk. Despite its extensive use in clinical practice, blood pressure is still a developing field and a recent focus on blood pressure variability has prompted a contemporary review of this important topic.
Blood pressure was first determined in 1733 by Stephen Hales, when he measured the blood pressure of a horse with a water manometer. Subsequently, the Russian surgeon, Nicolai Korotkoff, described the changing sounds heard by the stethoscope during cuff deflation, giving birth to the Korotkoff method, which is still widely used. Variability of blood pressure was initially explored by William Marston in 1917 when he used changes in an individual’s blood pressure to detect deception – an observation that formed the basis for the original polygraph, which was subsequently developed as a lie detector. Later it was demonstrated that short-term blood pressure variability was strongly influenced by behavioural, humoral, environmental and mechanical factors. It was from these observations that white-coat hypertension and masked hypertension were first recorded.
Further progress in blood pressure measurement followed the development of the Dinamap. This was a fully automated blood pressure device, which, together with the subsequent proliferation of small handheld digital machines, allowed clinicians access to unique home blood pressure readings that hitherto had not been available. Based on these home readings, further information on white-coat and masked hypertension became available.
With the advent of 24-hour blood pressure recording devices, not only could average blood pressures be measured during the day and night, but determination of blood pressure variability during this 24-hour period could be derived. Mancia and colleagues explored the relationship between 24-hour blood pressure variability and end-organ damage over a 7.5-year period and concluded that end-organ damage was independently related to blood pressure variability.1 Other authors, subsequently, confirmed this association.
Longer-term blood pressure variability has traditionally been based on a series of clinic measurements of blood pressure. Grove et al. (1997) showed that, among men who took antihypertensive medication, the standard deviation of blood pressure measurements based on a series of clinic readings of blood pressure obtained over a 10-year period, was greatly reduced compared with men who were not taking medication. The authors suggested that the benefits from antihypertensive medication, with respect to the observed reduction in coronary heart disease outcomes, may have been partly due to the reduction in systolic blood pressure variability.2
Over the past two decades, many studies of long-term blood pressure variability have confirmed the link between high variability and worse cardiovascular outcome.3 In a major review, Parati and colleagues concluded that all forms of increased blood pressure variability, including short, mid- and long-term blood pressure variability, were associated with cardiac, brain, vascular and renal damage, and an increased risk of cardiovascular and all-cause mortality.4
However, these early reports on blood pressure variability were largely ignored, and long-term visit-to-visit blood pressure variability has been considered an obstacle to the reliable estimation of usual blood pressure and considered as ‘background noise’.
More recently, the significance and importance of long-term blood pressure variability as a predictor of subsequent cardiovascular risk, based on the emerging evidence-base, has been recognised by national and international guidelines, and, in the UK, repeated measurements of blood pressure and derived variability have been incorporated into cardiovascular risk scores (QRisk 3).5 However, to date, clinical guidelines do not recommend treatment for blood pressure variability.
In this paper, we aim to provide information on how clinicians may introduce the evaluation of blood pressure variability into their practice by providing recommendations for defining blood pressure variability, the effective measurement of blood pressure variability, the comorbidities related to blood pressure variability and insight into treatment options.
Defining blood pressure variability
Blood pressure variability is a general term that encompasses variations in blood pressure over different time scales. To fully appreciate the significance of long-term blood pressure variability it is essential to understand the broader context of blood pressure variability, which includes very-short-term blood pressure variability (within beat and beat-to-beat), short-term blood pressure variability (within 24 hours, including diurnal variations) (figure 1), mid-term blood pressure variability (over days), and long-term blood pressure variability (over weeks, months, seasons, and even years) (figure 2).
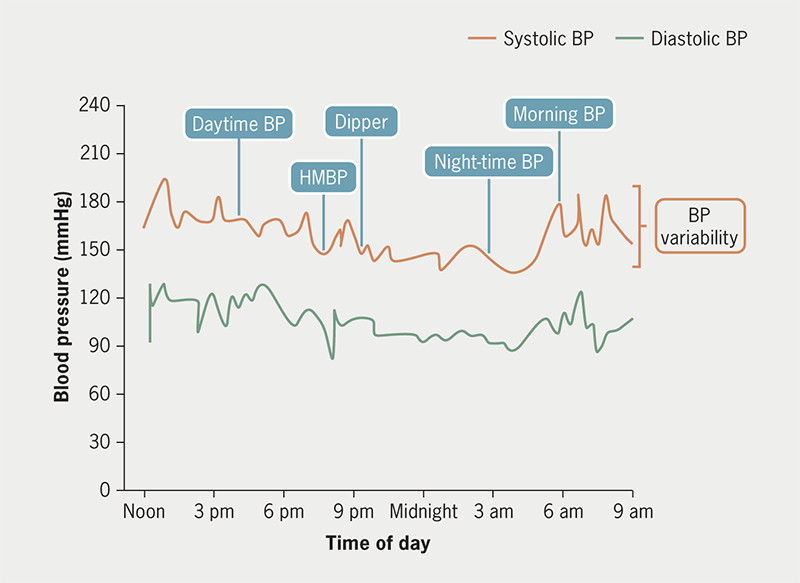
| Key: BP = blood pressure; HMBP = home measurement of blood pressure |
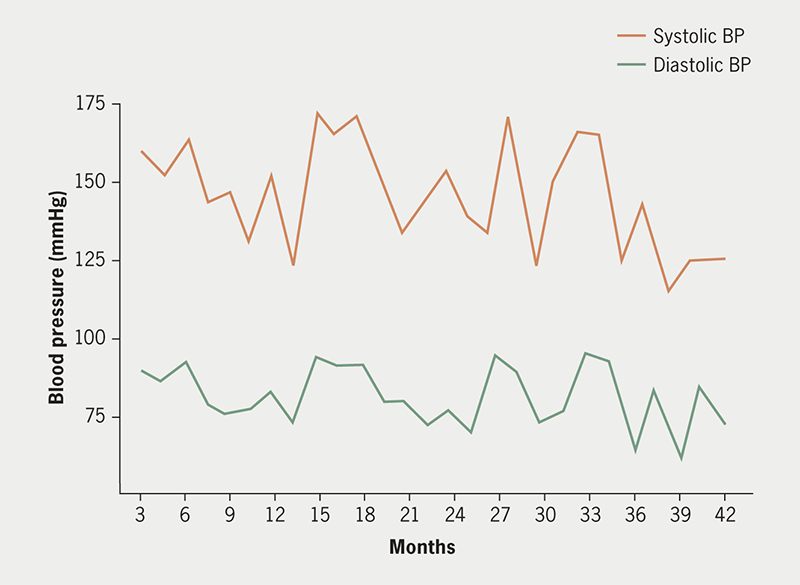
| Key: BP = blood pressure |
While understanding short-term blood pressure variability, including the ‘morning surge’ and ‘nocturnal dipping’, is crucial, long-term blood pressure variability where blood pressure variability extends over weeks, months, and seasons, is becoming increasingly important for comprehending its effects on cardiovascular and renal outcomes.
Before discussing long-term blood pressure variability, it is pertinent to acknowledge that blood pressure naturally fluctuates throughout the day due to a number of factors including diurnal variation, physical activity and emotional stress.
Long-term blood pressure variability, specifically visit-to-visit variability, has emerged as a predictor of adverse cardiovascular outcomes, including stroke and coronary events, especially in high-risk patients. Several studies have corroborated this association, highlighting its clinical relevance in risk stratification.3
Factors influencing long-term blood pressure variability
Long-term blood pressure variability is influenced by various factors that differ significantly from those impacting short-term blood pressure variability. In the winter season, blood pressure tends to rise to higher levels on average, and this may be attributed to the cold temperatures causing sympathetic activation. Physiological and pathological factors, including vascular compliance and vascular structure, play pivotal roles in influencing long-term blood pressure variability. Vascular compliance refers to the ability of blood vessels to expand and contract in response to changes in blood pressure. When vascular compliance is reduced, arteries become stiffer and less able to buffer fluctuations in blood pressure. Together with impaired baroreceptor function, large artery stiffening will result in elevated long-term blood pressure variability. Conversely, long-term blood pressure variability mediated through changes in endothelial function and remodelling of arteries may lead to arterial stiffening.
Thus, maintaining optimal vascular compliance and structure is crucial for the stability of long-term blood pressure variability, as any deviations from the norm can contribute to the development and progression of cardiovascular disease. Understanding the intricate interplay between these factors is essential for advancing our knowledge of long-term blood pressure variability and its overall impact on cardiovascular health.
Defining excessive blood pressure variability
Defining what constitutes excessive blood pressure variability has been a subject of ongoing debate within the scientific community. In the long-term follow-up of the Anglo-Scandinavian Cardiac Outcomes Trial (ASCOT), a standard deviation of 10 mmHg or more in systolic blood pressure variability was associated with a significant increase in cardiovascular events.6 Some authors have suggested a pragmatic threshold of 12–13 mmHg as a level above which increased risk should be flagged. These figures are, however, derived from elderly hypertensive patients and ‘normal’ values for blood pressure variability derived from younger disease-free individuals are lower, in the region of 7–10 mmHg. In ASCOT, those participants with higher long-term visit-to-visit systolic blood pressure variability were older, were more likely to smoke, had a history of diabetes and more likely to have a history of atherosclerotic vascular disease.
Statistical methods to analyse long-term blood pressure variability
The standard deviation (SD), which measures the degree of variability of a set of values around their mean, is commonly utilised to assess short-term and long-term blood pressure variability due to its ease of determination. However, SDs may be less informative when comparing variability between groups with varying mean blood pressure levels. Although alternative measures, such as the coefficient of variation (CV), calculated as the ratio of SD to the mean value expressed as a percentage, or a calculation of the variation independent of the mean, may be more appropriate in some cases, for everyday assessment using simple measurements and calculations, the SD is preferred.
How to measure blood pressure variability
Current methods of blood pressure monitoring
The standardised and universally used method of non-invasively estimating blood pressure is brachial cuff sphygmomanometry. It is vital, however, that an appropriate cuff size is used by overweight and frankly obese patients, as spuriously high blood pressure readings are recorded when small or regular cuffs are used in patients with a large arm circumference.
According to National Institute for Health and Care Excellence (NICE) guidelines,7 readings above 140/90 mmHg alone are not sufficient to make a diagnosis of hypertension, and ambulatory blood pressure monitoring (ABPM) is proposed for all patients with a systolic blood pressure of 140 mmHg to 180 mmHg. For patients unable to tolerate ABPM, home blood pressure monitoring (HBPM) is offered as an alternative.
ABPM provides readings of blood pressure over a period of 24 hours. Average blood pressures are calculated for daytime, night-time and 24 hours. A daytime average of 135/85 mmHg or above is considered to confirm a diagnosis of hypertension. ABPM over 24 hours also provides a measure of short-term blood pressure variability.
Currently HBPM is used primarily in cases where ABPM is unsuitable or declined by the patient. There is no standard protocol, but it is recommended that patients should take a reading two or three times every morning and evening for four to seven days, using an automated brachial cuff. An average reading of 135/85 mmHg is required to confirm a diagnosis of hypertension following a raised in-office measurement.
HBPM is a suitable way of obtaining data on long-term trends in patients’ blood pressure variability. However, a greater evidence-base is needed to ascertain the frequency of home measurements to reproducibly ascertain a metric for blood pressure variability. The Finn-Home study concluded that two readings must be taken every morning for at least three days, with the prognostic accuracy rising slightly if measurements were taken for seven days.8 However, further studies are required to establish whether a longer time interval is required to assess long-term variability using HBPM, and how data derived from this method of blood pressure recording relate to values obtained from clinic visit-to-visit measurements.
Visit-to-visit blood pressure readings from the clinic currently provide the best data on long-term blood pressure variability. Despite the effects of white-coat and masked hypertension, the results of brachial cuff blood pressure measurement would be most reliable, reproducible and accurate when carried out by a skilled healthcare professional. Most clinical trials investigating blood pressure variability used in-office data, so it can be best standardised.
There is a very limited evidence-base to determine over what time period visit-to-visit variability should be measured in the clinic, and there is no consensus over what visit gap is ideal between visits. Data from a Malaysian study suggested that systolic blood pressure measured on six separate occasions over a follow-up period of approximately two years gives a reliable estimate of blood pressure variability.9
Combining HBPM and visit-to-visit blood pressure monitoring
There are no current guidelines in the UK on parameters and investigations into blood pressure variability. The most suitable procedure of investigation will probably rely on hybrid data from clinic visit-to-visit variability and HBPM. Further clinical trials are needed to determine the best diagnostic approach. Regular clinic blood pressure monitoring should be targeted to groups at risk of high blood pressure variability, to best identify who should require HBPM.
Novel technology
Cuffless, non-invasive blood pressure monitoring is now integrated into many of the latest smart watches, including Fitbit and Samsung’s newest releases. They generally use analysis by photoplethysmography, and often require calibration by taking a reading with a brachial cuff first.
Unlocking this technology in a clinical context would give clinicians a vast amount of blood pressure data, allowing them to determine very short-term and long-term trends in blood pressure. The validation of the accuracy of these devices is essential, and when combined with app-based technology for recording and transmitting blood pressure data, provides a real opportunity for future advances in the blood pressure management of hypertensive patients.
Blood pressure variability and cardiovascular and renal outcomes
There are certain patient groups and diseases that are associated with increased risk of cardiovascular and renal disease. Some studies have investigated the strength of blood pressure variability as a predictor of adverse outcomes in these populations, which we will briefly outline below.
Populations with hypertension
The ASCOT trial followed over 19,000 hypertensive patients for 5.5 years, and found systolic blood pressure variability to be a powerful predictor of stroke, coronary outcomes and progressive renal impairment. Visit-to-visit variability, determined from six-monthly measurements of blood pressure throughout the trial, was a stronger predictor than short-term variability or within-visit variability.10 While mean systolic blood pressure only predicted stroke risk in the highest decile of systolic blood pressure, all measures of visit-to-visit systolic blood pressure variability predicted stroke and coronary outcomes, with the top decile showing around a four-fold risk compared with the bottom decile.
In the long-term follow-up of ASCOT, over a total of 20 years, these observations were confirmed. In addition, it was demonstrated that among those with well-controlled blood pressure during the original trial, those with high systolic blood pressure variability remained at higher cardiovascular risk than many with much higher blood pressures but low blood pressure variability (figure 3).6
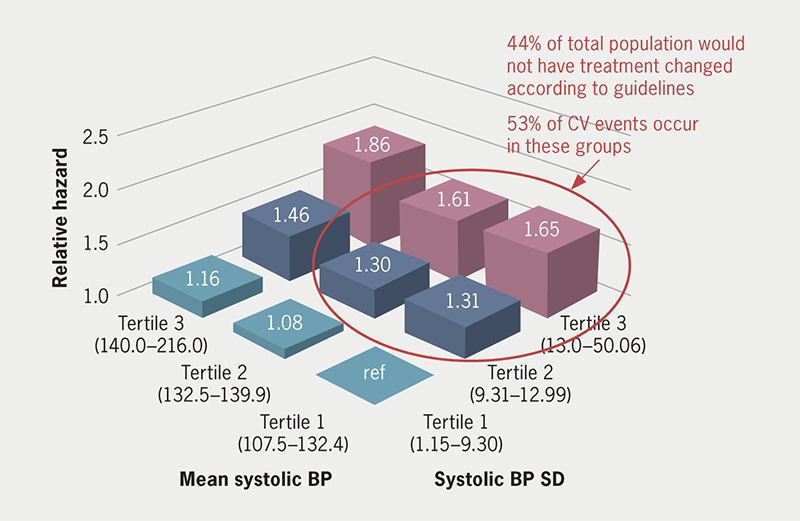
| Key: BP = blood pressure; SD = standard deviation; CV = cardiovascular |
Results of other trials and observational studies have subsequently confirmed the findings of cardiovascular risk associated with long-term blood pressure variability, independent of average blood pressures, with risk-ratio estimates of increased blood pressure variability on cardiovascular disease to be comparable with those of cholesterol.3
Populations with coronary heart disease
Post-hoc analyses of data from at least two trials have shown that in patients with stable coronary artery disease, visit-to-visit systolic blood pressure variability is associated with increased cardiovascular events and long-term mortality. The mechanisms by which blood pressure variability affects atherosclerotic plaques is unclear. It has been suggested that increases in blood pressure variability accelerate the degree of atherosclerosis, as well as increasing the percentage of lipid volume, making the plaque more susceptible to rupture. Blood pressure variability has also been shown to affect the expression of inflammatory mediators.
Populations with atrial fibrillation
Some studies have reported no difference in long-term blood pressure variability in patients with and without atrial fibrillation. Others report small increases in blood pressure variability in those who develop atrial fibrillation during various treatment regimens, however, these findings could be confounded by the differential effects of antihypertensive drugs on blood pressure variability.
In patients with atrial fibrillation, increased visit-to-visit variability in systolic blood pressure has been found to be associated with decreased quality of anticoagulation control. Anticoagulation control affects mortality in patients with atrial fibrillation. Indeed, one study found that the incidence of stroke, major bleeding, cardiovascular death and all-cause mortality increased when systolic blood pressure variability increased.
Populations with cerebrovascular disease
Not only is increased systolic blood pressure variability associated with increased risk of first stroke, but blood pressure variability also remains a risk factor for adverse events in patients with a past history of cerebrovascular disease. In patients with previous intracerebral haemorrhage, ischaemic stroke, or transient ischaemic attack (TIA), systolic blood pressure variability is associated with recurrent stroke, independent of average blood pressure.
Aside from increased cardiovascular risk, visit-to-visit blood pressure variability is also demonstrated to be associated with cognitive decline in patients with ischaemic stroke, most likely due to periods of cerebral hypoperfusion. High systolic blood pressure variability is associated with an increased risk of dementia.11
Populations with diabetes mellitus
In patients with type 2 diabetes mellitus, increased visit-to-visit variability in systolic blood pressure is associated with increased risk of macrovascular and renal events, even after adjusting for mean systolic blood pressure and cardiovascular risk factors. Incorporation of systolic variability into risk models improves risk prediction when compared with other risk factors, such as mean systolic blood pressure.
While long-term variability in systolic blood pressure is shown to be linked to development of nephropathy in patients with diabetes, no association was found for the development of retinopathy.
Populations with chronic kidney disease (CKD)
Blood pressure variability is associated with 21% increased risk of CKD progression, giving it a similar prognostic value to diabetes (20%). A meta-analysis showed that blood pressure variability was significantly associated with end-stage renal disease and renal outcomes.12 Patients with CKD tend to have arterial stiffness, chronic inflammation, and higher sympathetic activity, which may lead to increased blood pressure variability. Furthermore, in adults with stage 3 or 4 CKD, blood pressure variability is a strong predictor of stroke and increased mortality.
Haemodialysis patients are more susceptible to blood pressure fluctuations before, during and after treatment. Though long-term blood pressure variability is less well studied in this patient demographic, it was found that, after adjusting for demographic and clinical factors, increases in pre-dialysis systolic blood pressure variability are associated with higher risk of all-cause mortality and major adverse cardiovascular events, independent of the mean blood pressure.
Populations with COVID-19
Previous studies have shown that hypertensive patients are more susceptible to contracting COVID-19, and high blood pressure is associated with increased disease severity and mortality in COVID-19 patients.13 It is hypothesised that the systemic inflammation and endothelial dysfunction leads to blood pressure dysregulation and increased blood pressure variability.
To our knowledge, there are no studies investigating the relationship between visit-to-visit blood pressure variability and adverse outcomes in COVID-19 patients, however, a Chinese study found day-by-day systolic blood pressure variability to be an independent predictor of mortality and acute respiratory distress syndrome in hypertensive COVID-19 patients. Blood pressure variability may also play a role in long-COVID syndrome. A study investigating different ambulatory 24-hour blood pressure parameters in young adults with long-COVID found significantly greater blood pressure variability compared with age-matched healthy controls.14
Treatment of long-term blood pressure variability
Table 1. Effect of drug classes versus all other drug classes on systolic blood pressure variability15
| Antihypertensive drug class | Effect of treatment on inter-individual systolic BP variability |
| CCB | Decrease |
| Non-loop diuretic | Decrease |
| ACEi | Increase |
| ARB | Increase |
| BB | Increase |
| CCB versus placebo | Decrease |
| Key: ACEi = angiotensin-converting enzyme inhibitor; ARB = angiotensin-receptor blocker; BB = beta blocker; BP = blood pressure; CCB = calcium-channel blocker | |
Several studies have demonstrated the widely varying effects of different antihypertensive drugs on long-term blood pressure variability (table 1). It is clear from meta-analyses that beta blockers increase blood pressure variability,15 and this was dramatically demonstrated in ASCOT.16 Whether beta blockers with additional pharmacological properties would have differential effects remains uncertain. Angiotensin-converting enzyme (ACE) inhibitors and angiotensin-receptor blockers (ARB) appear to have no beneficial effect on blood pressure variability. There is convincing evidence that long-acting calcium-channel blockers, notably amlodipine, reduce blood pressure variability, and that thiazide diuretics also appear to have some beneficial effect. In ASCOT, the benefits of the amlodipine regimen on cardiovascular outcomes were clearly related to the drug’s action on reducing systolic blood pressure variability.
Summary and conclusion
There is now overwhelming evidence that long-term systolic blood pressure variability, independent of average levels of blood pressure, is associated with an increased risk of cardiovascular and renal outcomes in various patient populations. National guidelines recognise blood pressure variability in risk assessment.
Most of the evidence to date is based on visit-to-visit measurements of clinic blood pressures over periods of weeks, months and years. New research is needed to establish a more practical way of assessing long-term variability, and home blood pressure measurement is currently being evaluated as an alternative.
While there are no prospective trials of different treatment options for blood pressure variability, retrospective studies clearly demonstrate that long-acting calcium-channel blockers, such as amlodipine, reduce long-term blood pressure variability compared with other classes of antihypertensive drugs, and should be incorporated into treatment strategies for those patients considered at increased risk because of high blood pressure variability.
Key messages
- Long-term visit-to-visit blood pressure variability is now established as a cardiovascular risk factor independent of mean levels of systolic blood pressure
- It is currently determined by deriving the standard deviation (SD) of several measurements of clinic blood pressure (ideally seven or more). Values in excess of 12 mmHg are associated with significant increases in cardiovascular risk
- Current research is aimed at establishing whether home blood pressure recording might be used as an alternative and easier way of determining systolic blood pressure variability
- Analyses from clinical trials suggest that long-acting calcium-channel blockers, such as amlodipine, and thiazide-like diuretics, are the only antihypertensive drugs that lower long-term systolic blood pressure variability, and should be used preferentially when variability is high
Conflicts of interest
PS declares receipt of payment for lectures and travel from Viatris. AL, LL, AR and AS: none declared.
Funding
PS acknowledges support from the Biomedical Research Centre Award to Imperial College Healthcare NHS Trust.
References
1. Mancia G, Parati G. Ambulatory blood pressure monitoring and organ damage. Hypertension 2000;36:894–900. https://doi.org/10.1161/01.HYP.36.5.894
2. Grove JS, Reed DM, Yano K et al. Variability in systolic blood pressure – a risk factor for coronary heart disease? Am J Epidemiol 1997;145:771–6. https://doi.org/10.1093/oxfordjournals.aje.a009169
3. Stevens SL, Wood S, Koshiaris C et al. Blood pressure variability and cardiovascular disease: systematic review and meta-analysis. BMJ 2016;354:i4098. https://doi.org/10.1136/bmj.i4098
4. Parati G, Bilo G, Kollias A et al. Blood pressure variability: methodological aspects, clinical relevance and practical indications for management – a European Society of Hypertension position paper. J Hypertens 2023;41:527–44. https://doi.org/10.1097/HJH.0000000000003363
5. Hippisley-Cox J, Couplad C, Brindle P. Development and validation of QRISK3 risk prediction algorithms to estimate future risk of cardiovascular disease: prospective cohort study. BMJ 2017;357:j2099. https://doi.org/10.1136/bmj.j2099
6. Gupta A, Whiteley WN, Godec T et al.; the ASCOT-10 Investigators. Legacy benefits of blood pressure treatment on cardiovascular events are primarily mediated by improved blood pressure variability: the ASCOT trial. Eur Heart J 2024;45:1159–69. https://doi.org/10.1093/eurheartj/ehad814
7. National Institute for Health and Care Excellence. Hypertension in adults: diagnosis and management. NG136. London: NICE, August 2019. Available from: https://www.nice.org.uk/guidance/ng136
8. Niiranen TJ, Hanninen M-R, Johansson J et al. Home-measured blood pressure is a stronger predictor of cardiovascular risk than office blood pressure. The Finn-Home Study. Hypertension 2010;55:1346–51. https://doi.org/10.1161/HYPERTENSIONAHA.109.149336
9. Lim HM, Chia YC, Ching SM et al. Number of blood pressure measurements needed to estimate long-term visit-to-visit systolic blood pressure variability for predicting cardiovascular risk: a 10-year retrospective cohort study in a primary care clinic in Malaysia. BMJ Open 2019;9:e025322. https://doi.org/10.1136/bmjopen-2018-025322
10. Rothwell PM, Howard SC, Dolan E et al. Prognostic significance of visit-to-visit variability, maximum systolic blood pressure, and episodic hypertension. Lancet 2010;375:895–905. https://doi.org/10.1016/S0140-6736(10)60308-X
11. De Heus RAA, Tzourio C, Lee EJL et al. Association between blood pressure variability with dementia and cognitive impairment: a systematic review and meta-analysis. Hypertension 2021;78:1478–89. https://doi.org/10.1161/HYPERTENSIONAHA.121.17797
12. Yang L, Li J, Wei W et al. Blood pressure variability and the progression of chronic kidney disease: a systematic review and meta-analysis. J Gen Intern Med 2023;38:1272–81. https://doi.org/10.1007/s11606-022-08001-6
13. He C, Liu C, Yang J et al. Prognostic significance of day-by-day in-hospital blood pressure variability in COVID-19 patients with hypertension. J Clin Hypertens (Greenwich) 2022;24:224–33. https://doi.org/10.1111/jch.14437
14. Ternushchak TM, Tovt-Korshynska MI, Varvarynets AV. Ambulatory blood pressure variability in young adults with long-COVID syndrome. Wiad Lek 2022;75:2481–5. https://doi.org/10.36740/WLek202210131
15. Webb AJS, Fischer U, Mehta Z et al. Effects of antihypertensive-drug class on interindividual variation in blood pressure and risk of stroke: a systematic review and meta-analysis. Lancet 2010;375:906–15. https://doi.org/10.1016/S0140-6736(10)60235-8
16. Rothwell PM, Howard SC, Dolan E et al.; on behalf of the ASCOT-BPLA and MRC Trial Investigators. Effects of β-blockers and calcium-channel blockers on within-individual variability in blood pressure and risk of stroke. Lancet Neurol 2010;9:469–80. https://doi.org/10.1016/S1474-4422(10)70066-1
