New data gathered via a survey undertaken on behalf of the British Cardiac Patients Association (BCPA) confirm not only that angina itself has an adverse impact on lifestyle, but that the side effects associated with some of the currently prescribed therapies for angina may be exacerbating the situation for patients.
Introduction
It has been estimated that about two million people in the UK experience the painful and debilitating symptoms of angina – one million men and more than 920,000 women.1 About 17% of men and 8% of women aged 65–74 have been diagnosed with angina at some point in their lives2 and there are about 338,000 new cases of angina each year.1 Not only does angina pose a considerable burden on patients and their carers, it also represents a significant financial burden, costing the National Health Service (NHS) about £700 million each year.3
Alongside the physical trauma of symptoms experienced by patients, angina also detrimentally affects all aspects of quality of life, including personal and sexual relationships, physical mobility and emotional well-being.4 While most physicians would consider angina to be manageable both therapeutically and through increasingly common surgical intervention, new data from a survey of angina patients suggest that this common cardiac disorder is being managed sub-optimally – leaving patients with continuing symptoms and sometimes intolerable side effects.5
The impact of inadequately controlled angina is such that patients’ quality of life is further compromised with patients continuing to experience frequent episodes of angina despite the medication they have been prescribed.5 While these new data suggest that more could be done to improve the management of patients with chronic stable angina, new advances in treatment options, together with increasing acknowledgement by clinicians of the importance of selectively lowering heart rate, may offer the realistic hope of more effective management in the future.
The BCPA survey
The survey data were based on responses from 609 British Cardiac Patients Association (BCPA) members to a postal questionnaire, which questioned respondents on all aspects of living with angina, from the frequency and severity of their symptoms to the impact of treatment, and paints a startling picture for healthcare professionals and patients alike.5 The findings provide a revealing insight into the true impact of angina on patients’ quality of life.
Over 45% of respondents rate the episodes of angina they have experienced as ‘extremely’ or ‘moderately’ debilitating with 35% reporting that angina has a significant/extreme impact on their quality of life.5 Future health status, the impact of angina on work prospects and the limitations imposed on day-to-day activities were listed as major concerns.5 In addition, two-thirds of patients say their sex life has been adversely affected, highlighting the range of lifestyle factors that are affected by their condition.5
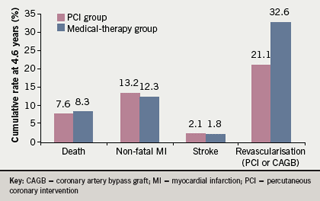
The survey data also confirm that despite surgical intervention in the majority of those questioned, patients continued to experience frequent symptoms.5 This is consistent with clinical evidence6 and is a timely reminder in the wake of the results from the Clinical Outcomes Utilizing Revascularization and Aggressive Drug Evaluation (COURAGE) trial that intervention has significant limitations. COURAGE confirmed that percutaneous coronary intervention (PCI) did not reduce the risk of death, myocardial infarction (MI) or other major cardiovascular events when added to optimal medical therapy (figure 1).7
However, the BCPA data also highlight the limitations of some therapeutic options for angina. It was reported that angina patients experience an average of 79 episodes a year even after diagnosis and treatment and more than 50% continue to experience at least one episode a week.5
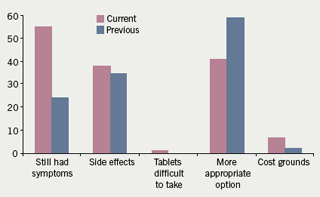
The survey also looked in some detail at some of the issues that patients have with their prescribed treatment, in particular, the tiredness and lethargy associated with regular beta blocker use.5 A significant proportion of those who were prescribed beta blockers as part of their treatment regimen were also being treated for concomitant conditions such as asthma and chronic obstructive pulmonary disease (COPD),5despite the fact that these agents are generally not recommended in patients with respiratory disorders.8 Nearly one-third of those questioned believed that their current treatment does not adequately reduce their symptoms, and that as a result, more than 50% had had their treatment changed (figure 2).5
The failure of therapy to meet an important prescribing imperative, i.e. that it should induce ‘few’ adverse side effects, was also highlighted, and specifically cited by nearly one in three of those surveyed.5 More than 25% felt that treatment-related side effects have a significant/extreme effect on their quality of life, and although 80% of those responding to the questionnaire have discussed such side effects with their doctor, only one-third have had their treatment changed as a result.5 Sixty per cent of angina patients on beta blockers reported suffering from tiredness, while nearly one in three said that their energy levels had deteriorated following prescribed treatment.5
Over 45% of respondents rate the episodes of angina they have experienced as ‘extremely’ or ‘moderately’ debilitating with 35% reporting that angina has a significant/extreme impact on their quality of life .5
Clinical implications of the BCPA survey
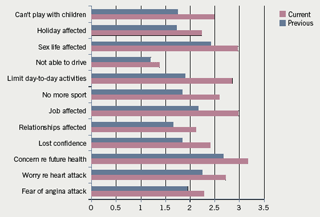
The BCPA data confirm what physicians already know in that the burden of angina is substantial and highly debilitating (figure 3), but also raise a number of questions about current management strategies. It is likely that a number of factors, such as patient non-compliance, are likely to have a bearing on the main finding of the survey – the continuation of symptoms following the onset of treatment. However, the results also suggest that clinicians could potentially be doing more to help patients with angina find a treatment option that works for them.
While beta blockers are indisputably effective drugs for treating angina, their drawbacks are well known.8 They remain the drug of choice for treating angina, due in part to their heart rate reducing properties,9however, with a heavy side effect profile and, as with all anti-anginals, a lack of robust outcome data (except post-MI),10 their use should be carefully considered and the implications fully explained to patients.
The impact of fatigue, lethargy, insomnia, nightmares and impotence,8 associated with beta blockers, on patients should not be underestimated. A key goal of angina management is to restore patients’ quality of life by alleviating symptoms, however, the data suggest that the side effects of treatment can sometimes mitigate the benefits experienced by patients.5
These side effects have recently been recognised in an internet survey of 500 general practitioners (GPs), cardiologists, diabetologists, geriatricians, respiratory specialists and clinicians in general medicine.11 This survey suggested healthcare professionals are aware of the drawbacks of some anti-anginals. It found that ‘lack of efficacy’ and ‘intolerable side effects’ are the most important elements that would prompt a switch to other anti-anginal treatment options, with very similar findings for GPs and cardiologists.11
According to respondents, the most common side effect of anti-anginal treatment reported by the patients was tiredness (82%), followed by lethargy (67%), swollen ankles (64%), erectile dysfunction (56%), headache (53%) and dizziness (52%).11 This recognition by healthcare professionals of the side effects being experienced by their patients is reassuring, however, it is important that clinicians work with their patients to find solutions for managing the impact of these.
Angina key statistics1–3
- 17% of men and 8% of women will be diagnosed with angina at some point in their life
- 338,000 new cases each year
- Costs NHS £700 million each year
Current guidelines on angina management lack a coherent approach for the management of the significant numbers of angina patients for whom beta blockers are not suitable as a first-line treatment option.12 Beta blockers are usually not advisable in patients with severe symptomatic peripheral arterial disease, atrioventricular block, sinus bradycardia, sick sinus syndrome and not recommended for those with asthma, COPD or a history of bronchospasm.8 Despite this, the BCPA data suggested patients with asthma/COPD were still being prescribed beta blockers, perhaps due to a perceived lack of effective alternatives.5
Alternatives to beta blockers, such as calcium channel blockers, nitrates and potassium channel activators, are all also associated with significant side effects8 and, while efficacious in reducing symptoms, do not all have the same heart rate reducing qualities of beta blockers, an important consideration given the role of heart rate reduction in reducing ischaemia.13
The advent of new heart rate reducing anti-anginals, which have recently been developed, may offer clinicians an opportunity to minimise the impact of treatment-related side effects while achieving symptom control.13
The role of heart rate reduction
Heart rate reduction has been described as the ‘cornerstone’ of angina management and there are clear mechanisms by which heart rate might influence the risk of cardiovascular disease.14 Heart rate is a major determinant of myocardial oxygen consumption and metabolic demand, and consequently of myocardial workload. A high heart rate leads to both greater myocardial oxygen consumption (MVO2) and a decrease in myocardial perfusion, by shortening the duration of diastole, which can induce or exacerbate myocardial ischaemia. A reduction in heart rate should, therefore, elevate the ischaemic threshold and improve cardiac performance.13
There are also indications that sustained elevations in heart rate may play a direct role in the pathogenesis of coronary atherosclerosis, and that by implication, heart rate reduction may reduce the risk for coronary artery disease (CAD) and sudden death.15 Given the acceptance among healthcare professionals that heart rate reduction is key in treating angina, the proliferation of beta blocker use despite their side-effect profile is perhaps unsurprising. Indeed, further data from the survey of healthcare professionals suggest the perceived significance of heart rate may be increasing.11
In addition to looking at healthcare professionals’ perceptions of side effects, the internet survey also questioned respondents on their attitudes towards heart rate. The results confirm that healthcare professionals do recognise the importance of controlling heart rate as part of the strategy for managing patients with angina.11 Specifically, the survey revealed that 47% of cardiologists and 36% of geriatricians feel it is ‘very important’ to control heart rate in managing angina, with a quarter of generalists and a fifth of GPs and diabetologists agreeing.11 Perhaps more surprising is the finding that around a quarter of cardiologists, diabetologists, generalists and geriatricians also feel that it is ‘very important’ to control heart rate in improving angina patients’ survival.11 This marks an interesting shift towards recognition of heart rate as more than just a contributing factor to ischaemia and perhaps corresponds to a growing body of evidence that suggests heart rate may be an independent risk factor for cardiovascular disease.15
However, while current thinking may suggest this, current practice lags some way behind with the survey suggesting that although healthcare professionals regularly monitor and record the heart rate in around 70% of their patients, only 36% are specifically treated to reduce their heart rate.11
More than 50% angina patients continue to experience at least one episode a week despite optimal medical therapy .5
A recent survey of healthcare professionals revealed a quarter of cardiologists, diabetologists, generalists and geriatricians questioned feel that it is ‘very important’ to control heart rate in improving angina patients’ survival .11
The importance of patient education
While clinician recognition of side effects and the role of heart rate management and new therapeutic options represent positive steps in angina management, there is also an important need for improved patient information and education. Making patients aware of the side effects of their treatments in advance, providing them with information about how to manage those side effects or suggesting alternative options should they prove intolerable could all help to alleviate some of the burden depicted by the BCPA survey respondents.
Respondents to the survey reported being worried about their future health and waiting a considerable period of time before consulting their healthcare professional,5 suggesting that information must be provided through a range of channels. This also highlights the importance of organisations such as the BCPA in providing advice and support, not only for patients but also for their carers, the burden on whom is often overlooked.
In the age of the informed patient, where it may be taken for granted that the internet has empowered patients to educate themselves, the findings of this survey suggest that for some, this is simply not enough. Both healthcare professionals and patient groups alike still play a vital role in ensuring patients receive the standard of care they deserve.
Conclusion
Although for many patients angina will be a manageable condition that can be successfully treated either via surgery or therapeutically, for a significant number of patients an optimal solution has yet to be found. The BCPA survey clearly demonstrates that the everyday lives of patients with angina are seriously compromised by their condition and often compounded by the side effects of their medication, and that their quality of life is suffering as a direct result.5
It is to be hoped that the findings of this survey will prompt recognition of the true burden of angina, encouraging healthcare professionals to work with their patients to find appropriate solutions and offering hope to the thousands for whom uncontrolled angina invariably represents the precursor to more serious cardiac disease.
Conflict of interest
The BCPA survey was sponsored by Servier Laboratories and conducted in collaboration with Research Quorum.
Editors’ note
An editorial ‘Angina – more of a chronic problem than clinicians think’ by Usha Prasad and David Gray is published on pages 183–4.
Lena Izzat, Associate Specialist Cardiologist, Prince Philip Hospital, Llanelli, Carmarthenshire NHS trust Eve Knight, responsible for Service Development within the BCPA
References
- British Heart Foundation. Incidence of angina. Available at: http://www.heartstats.org/datapage.asp?id=1040 [accessed: 7 May 2007].
- British Heart Foundation. Prevalence of angina. Available at: http://www.heartstats.org/datapage.asp?id=1122 [accessed: 7 May 2007].
- Stewart S, Murphy NF, Walker A, McGuire A, McMurray JJ. The current cost of angina pectoris to the National Health Service in the UK. Heart 2003;89:848–53.
- Pocock SJ, Henderson RA, Seed P, Treasure T, Hampton JR. Quality of life, employment status and anginal symptoms after coronary angioplasty or bypass surgery. 3-year follow-up in the Randomized Intervention Treatment of Angina (RITA) Trial. Circulation 1996;94:135–42.
- BCPA. British Cardiac Patients Association survey 2007.
- Holubkov R, Laskey WK, Haviland A et al. Angina 1 year after percutaneous coronary intervention: A report from the NHLBI Dynamic Registry. Am Heart J 2002;144:826–33.
- Boden W, O’Rourke RA, Teo KK et al. Optimal medical therapy with or without PCI for stable coronary disease. N Engl J Med 2007;356:1503–16.
- Anti-anginals. Monthly Index of Medical Specialities. London: Haymarket, April 2007.
- Waller D, Javaid K. Drug choice in stable angina management. Prescriber 2001;12:1. Available at: http://www.escriber.com/Prescriber/Features.p?ID=75&GroupID=6&Action=View
- The Task Force on the management of stable angina pectoris of the European Society of Cardiology. Guidelines on the management of stable angina pectoris: executive summary. Eur Heart J 2006;27:1341–81.
- Attitudes to angina – a survey of healthcare professionals. Data on file – Servier, 2007.
- Patient UK. Angina pectoris. Available at: http://www.patient.co.uk/showdoc/40000534/#notes [accessed: 7 May 2007].
- Ferrari R. Editorial: Heart rate. Eur Heart J 2003;5(suppl G):1–2.
- Diaz A, Bourassa MG, Guertin MC, Tardif JC. Long-term prognostic value of resting heart rate in patients with suspected or proven coronary artery disease. Eur Heart J 2005;26:967–74.
- Singh BN. Increased heart rate as a risk factor for cardiovascular disease. Eur Heart J 2005;26: 943–5.
