A 68-year-old male with a background fhistory of squamous cell carcinoma of the epiglottis presented with recurrent syncope. During a witnessed collapse in Accident and Emergency (A&E), his heart rate decreased to 38 bpm and blood pressure dropped to 74/50 mmHg. Electrocardiogram (ECG) confirmed sinus bradycardia. Magnetic resonance imaging (MRI) of his neck revealed disease recurrence with a mass encasing the left internal carotid artery. He was diagnosed with reflex syncope secondary to mechanical stimulation of the carotid sinus. He had a dual-chamber pacemaker inserted, and re-presented with one further episode of collapse shortly afterwards. This report discusses the different options in managing this rare but debilitating symptom in head and neck cancers invading the carotid sinus.
Introduction
Syncope is defined as a transient loss of consciousness due to cerebral hypoperfusion followed by rapid and complete recovery. It is a common complaint, accounting for 3–5% of Accident and Emergency (A&E) attendances, and up to 50% of these patients are admitted to hospital.1 One rare cause of reflex syncope is mechanical stimulation of the carotid sinus by cancers of the head and neck, and this case demonstrates the challenges in its management.
Case report
A 68-year-old male presented to the A&E department having suffered from nine episodes of collapse on the day of admission. With the aid of collateral history from his wife, the collapses were described as feeling ‘funny’ and turning pale, immediately followed by complete loss of consciousness for a few seconds. Having fallen to the ground, he would quickly regain consciousness with a return of skin colour. He felt tired but not confused after each episode. The collapses were not associated with shaking of the limbs, tongue-biting or incontinence. He reported four or five similar independent episodes over the preceding five weeks, but he did not seek medical attention as he had made a quick and full recovery each time. He had also noticed progressive dysphagia and symptoms of gagging over the same period.
His past medical history included a squamous cell carcinoma of the epiglottis for which he had had radical surgery and radiotherapy 18 months previously. Since surgery, he had needed percutaneous endoscopic gastrostomy (PEG) feeding and suffered from recurrent oropharyngeal infections. He had no other medical problems. A recent follow-up computed tomography (CT) scan of his neck had shown a new mass, for which an appointment with the ear, nose and throat (ENT) surgeon had been arranged. His medication included lansoprazole, long-term co-amoxiclav, cyclizine, liquid morphine and tramadol. He lived with his wife and was independent with his activities of daily living. He was an ex-smoker and did not drink alcohol.
In A&E, he had a normal clinical examination. Initially, his blood pressure (BP) was 122/66 mmHg and pulse rate 67 bpm, regular. There were no cardiac murmurs on auscultation. He had a further witnessed collapse in the department, during which his BP fell to 74/50 mmHg and pulse to 38 bpm.
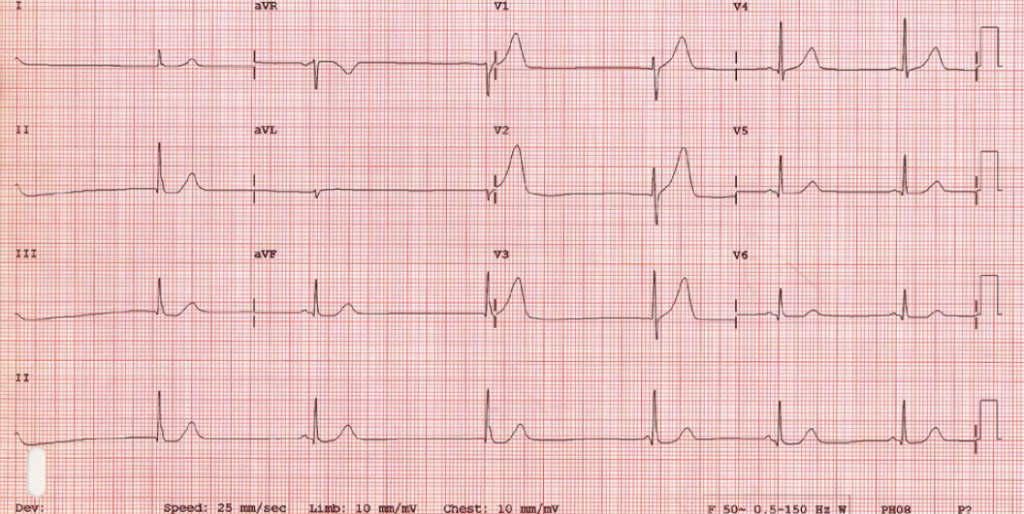
A 12-lead electrocardiogram (ECG) recorded during the collapse showed sinus bradycardia with a heart rate of 38 bpm (figure 1). Telemetry over the next 24 hours showed no further bradycardia or other arrhythmias. Blood results showed a mild normocytic anaemia (haemoglobin 116 g/L, mean cell volume [MCV] 91 fL), normal calcium (2.56 mmol/L) with raised alkaline phosphatase (123 U/L) and low albumin (30 g/L). White cell count was normal (6.9 × 109/L), but C-reactive protein was slightly raised (18 mg/L). Renal function was normal (creatinine 56 µmol/L, urea 5.3 mmol/L). Chest X-ray and CT of the brain were also normal.
Thus, the diagnosis of this patient was syncope. The differential diagnoses included cardiac syncope (e.g. brady/tachyarrhythmia, structural heart disease including severe aortic stenosis and hypertrophic obstructive cardiomyopathy), reflex syncope (e.g. vasovagal, situational, carotid sinus) and orthostatic hypotension (e.g. primary and secondary autonomic dysfunction, drug-induced, volume depletion).

A magnetic resonance imaging (MRI) scan of his neck showed tumour extending from just beyond the left common carotid artery bifurcation, encasing the left internal carotid artery all the way to the skull base and extending to the jugular foramen (figure 2). His syncope was clearly secondary to malignant invasion of the carotid sinus and most certainly of reflex type.
He was treated with a dual-chamber (DDDR) pacemaker insertion and was discharged. However, he re-presented with a further collapse 24 hours after discharge. His presenting BP was 101/47 and fell to 80/52 mmHg, but his pulse was consistently 80–90 bpm. After that he remained asymptomatic with no further collapses. There were no documented arrhythmias on the follow-up 24-hour ECG (heart rate range 84–124 bpm) or further BP drops. He was discharged and died shortly afterwards due to disease progression.
Discussion
The carotid sinus comprises baroreceptors located in the internal carotid artery near the carotid bifurcation and is principally involved in immediate blood pressure modulation, particularly during changes in posture. It is innervated by the sinus nerve of Hering, a branch of the glossopharyngeal nerve to which it joins at the inferior hypoglossal ganglion. The glossopharyngeal nerve passes up through the jugular foramen and synapses in the nucleus tractus solitaris of the medulla, the site of sympathetic and parasympathetic nerve modulation. Stimulation of the afferent nerve fibres in the carotid sinus increases vagal tone to the sinoatrial node and inhibits sympathetic tone to the peripheral vasculature, leading to bradycardia and reduced blood pressure.
Reflex syncope is a manifestation that these physiological reflexes involved in blood pressure control are abnormally triggered. Malignant invasion of the carotid sinus by head and neck tumours is a rare, but well-documented, cause of recurrent reflex syncope.2
Management of reflex syncope in advanced head and neck malignancy can be difficult.3 Double-blinded randomised trials investigating the role of pacemakers in these patients have not shown significant benefit,4 but the impact on symptoms may be greater if patients are selected according to documented episodes of asystole or severe bradycardia.5 Thus, physiological pacing can still be considered as one therapeutic approach in selected cases. Some case reports have demonstrated success with this approach.6,7 However, in other instances this has been unsuccessful.8,9 This may partly be attributed to the use of single chamber (VVI) rather than DDDR pacemakers.6 Our patient had a DDDR pacemaker inserted to manage the reflex bradycardia. He re-presented with a further collapse despite a functioning pacemaker, suggesting that though it prevented bradycardia, DDDR pacing, in our case, was insufficient to maintain adequate blood pressure during carotid sinus reflex activity. This is not surprising as multi-centre trials have shown similar results in patients with reflex syncope but no malignancy invading the carotid sinus.5,10
Finally, complete tumour regression and symptom resolution can be achieved in suitable cases by chemotherapy11 or surgical resection with glossopharyngeal and limited vagal neurectomy.12
In conclusion, this case shows that DDDR cardiac pacing can effectively abolish reflex bradycardia, but hypotension remains a challenge in managing carotid sinus syncope secondary to head and neck cancer•
Conflict of interest
None declared.
Key messages
- The carotid sinus baroreflex is an important physiological mechanism in the fine adjustment of blood pressure
- Malignant invasion of the carotid sinus by head and neck tumours can cause refractory syncopal collapses, which are difficult to manage
- Cardiac pacing in this situation has mixed results, and alternative approaches need to be considered
References
1. Nyman JA, Krahn AD, Bland PC, Griffiths S, Manda V. The costs of recurrent syncope of unknown origin in elderly patients. Pacing Clin Electrophysiol 1999;22:1386–94. http://dx.doi.org/10.1111/j.1540-8159.1999.tb00633.x
2. Macdonald DR, Strong E, Nielsen S, Posner JB. Syncope from head and neck cancer. J Neurooncol 1983;1:257–67. http://dx.doi.org/10.1007/BF00165610
3. Sharma J, Dougherty AH. Recurrent syncope in a cancer patient: a case report and review of the literature. Cardiol Res Pract 2011, Article ID 678237. http://dx.doi.org/10.4061/2011/678237
4. Connolly SJ, Sheldon R, Thorpe KE et al.; VPS II investigators. Pacemaker therapy for prevention of syncope in patients with recurrent severe vasovagal syncope. Second Vasovagal Pacemaker Study (VPS II): a randomized trial. JAMA 2003;289:2224–9. http://dx.doi.org/10.1001/jama.289.17.2224
5. Brignole M, Menozzi C, Moya A et al.; International Study on Syncope of Uncertain Etiology 3 (ISSUE-3) investigators. Pacemaker therapy in patients with neurally mediated syncope and documented asystole. Third International Study on Syncope of Uncertain Etiology (ISSUE-3): a randomized trial. Circulation 2012;125:2566–71. http://dx.doi.org/10.1161/CIRCULATIONAHA.111.082313
6. Yue AM, Thomas RD. Neurocardiogenic syncope due to recurrent tonsillar carcinoma: successful treatment by dual chamber cardiac pacing with rate hysteresis. Pacing Clin Electrophysiol 2002;25:121–2. http://dx.doi.org/10.1046/j.1460-9592.2002.00121.x
7. Campbell S, Walker D, Lanzon-Miller S, Gurr P. Nasal carcinoma a rare indication for a permanent pacemaker. Clin Med 2004;4:165–7. http://dx.doi.org/10.7861/clinmedicine.4-2-165
8. Ju JH, Kang MH, Kim HG et al. Successful treatment of syncope with chemotherapy irresponsive to cardiac pacemaker in head and neck cancer. Yonsei Med J 2009;50:725–8. http://dx.doi.org/10.3349/ymj.2009.50.5.725
9. Patel AK, Yap VU, Fields J, Thomsen JH. Carotid sinus syncope induced by malignant tumors in the neck: emergence of vasodepressor manifestations following pacemaker therapy. Arch Intern Med 1979;139:1281–4. http://dx.doi.org/10.1001/archinte.1979.03630480061019
10. Sutton R, Brignole M, Menozzi C et al.; Vasovagal Syncope International Study (VASIS) investigators. Dual-chamber pacing in the treatment of neurally mediated tilt-positive cardioinhibitory syncope pacemaker versus no therapy: a multicenter randomized study. Circulation 2000;102:294–9. http://dx.doi.org/10.1161/01.CIR.102.3.294
11. Choi YM, Mafee MF, Feldman LE. Successful treatment of syncope in head and neck cancer with induction chemotherapy. J Clin Oncol 2006;24:5332–3. http://dx.doi.org/10.1200/JCO.2006.08.0713
12. Lin HW, Rho MB, Amin-Hanjani S, Barker FG, Deschler DG. Glossopharyngeal and limited vagal neurectomy for cancer-related carotid sinus syncope. Skull Base 2009;19:369–73. http://dx.doi.org/10.1055/s-0029-1220204
