Correspondence from the world of cardiology
Aggressive risk factor modification: 30 year follow-up of IHD and non-haemorrhagic stroke
Dear Sirs,
In a single doctor’s practice in a high-risk area of South Sheffield, aggressive measures were taken to prevent ischaemic heart disease (IHD) and non-haemorrhagic stroke (ST) since 1980. Four cardinal risk factors were detected: smoking, diabetes, hypertension and cholesterol. Smoking, diabetes and hypertension were treated critically using standard guidelines and applying the latest evidence available independent of cost from 1980 onwards. Mortality from IHD has been known for many years to be directly related to the level of serum cholesterol and more specifically to the low-density lipoprotein (LDL) cholesterol. It was assumed therefore that as levels of LDL cholesterol approached zero then IHD mortality would almost be abolished. Diet, fibrates and cholestyramine were used as lipid-lowering therapy until 1988 after which statins were introduced on an intensive scale for all standard high-risk patients and those with a 20% risk of atherosclerotic vascular disease (AVD) under 70 years (British National Formulary).
Following the publication of the 4S (Scandinavian Simvastatin Survival Study) and WOSCOPS (West of Scotland Coronary Prevention Study) studies in 1995, simvastatin was given to patients with a 15% AVD risk under 80 years.
From the year 2000, atorvastatin and rosuvastatin were supplied to patients who failed to achieve an LDL cholesterol <2.0 mmol/L. Where statin side effects were experienced low doses of rosuvastatin 5 mg daily or less were given. All death records were retained and summarised from 1981 and divided into IHD, ST, malignancy and other. Population densities in decades were recorded.
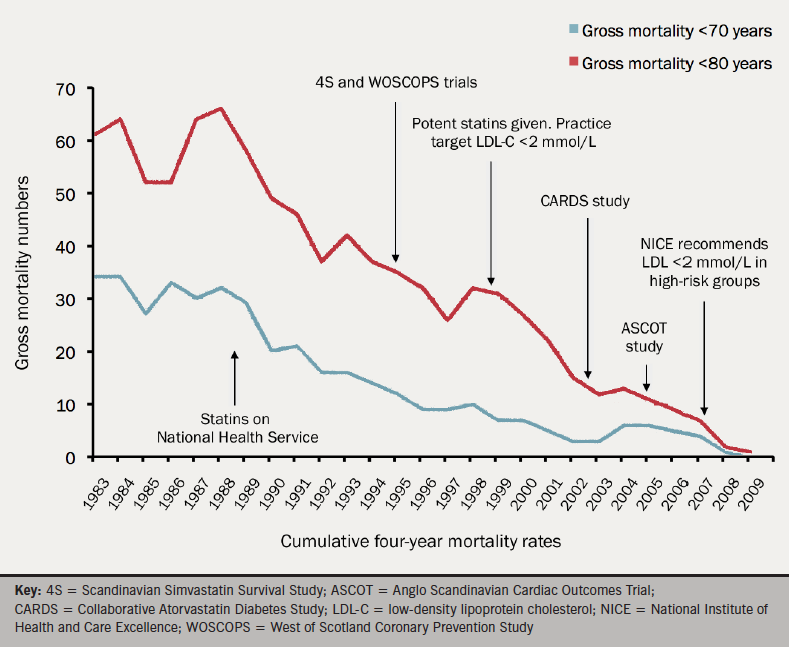
By reference to figure 1, using a four-year cumulative record of IHD and ST deaths, we can see that by 2008 in patients under 70 years, mortality was abolished and virtually abolished in those under 80 years. The fall in mortality follows closely the introduction of statins and the increasing progress towards more aggressive treatment to achieve an LDL cholesterol <2.0 mmol/L. Those in the over 70 age group were only offered statins from 1995 onwards and only gained full treatment after 2000. This is reflected in their mortality level falling at a much later time than the under 70 age group (figure 1).
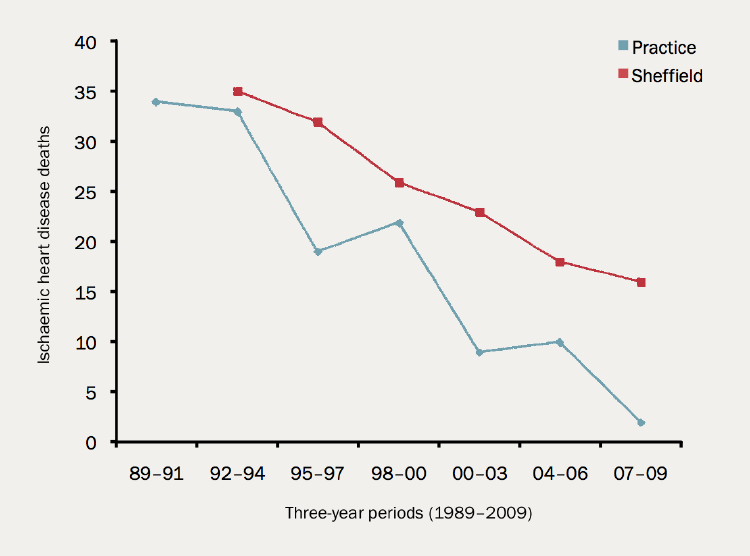
Comparing IHD and ST mortality in the first 10 years from 1981 in our practice, to the levels in the whole of Sheffield, we found these were roughly parallel (figure 2). After 1990 the mortalities began to diverge markedly with increasing difference until 2010. Whilst in Sheffield mortality in the last four years of the study period had approximately halved, compared with the first 10 years, the mortality in the practice was abolished in the under 70 age group and almost abolished in the 70–79 age group in the same period (see figure 2).
These data demonstrate that aggressive correcting of the lipid profile if actively pursued nationally would almost abolish mortality and morbidity for IHD and non-haemorrhagic ST. This would not only benefit patients, but would also be likely to be highly cost effective in saving hospital, general practitioners and social costs in treating the consequences of an event.
The present national policy as advocated by the National Institute for Health and Care Excellence and other authorities gives too little statin therapy at too late a stage in life and should be urgently amended.
Acknowledgment
JR would like to acknowledge the help provided by Dr Anthony Wierzbicki of Guy’s & St Thomas’ Hospital, London.
Dr John Revill
General Practitioner
Lowedges Clinic, 7 Lowedges, Sheffield,
S8 8LW
