It is unknown whether topical tissue adhesive provides comparable wound healing to absorbable sutures following cardiac device implant. This study was designed to compare wound closure using cyanoacrylate topical tissue adhesive with standard wound closure using absorbable sutures in patients receiving an elective permanent pacemaker implant.
Patients admitted for elective pacemaker implant were randomised to receive wound closure with either absorbable sutures or topical tissue adhesive (glue). Procedure duration, wound closure duration and wound size were recorded. Patients were evaluated at six and 12 weeks post-implant using validated wound evaluation scores by an experienced plastic surgeon who was blinded to the closure method.
Of 122 patients enrolled, 64 received topical tissue adhesive and 58 received absorbable sutures. Patients were well matched for baseline demographics. Use of topical adhesive was associated with shorter wound closure time (117 s, interquartile range [IQR] 92–136 vs. 277 s, IQR 231–311); no difference was seen in overall procedure duration. A total of 100 subjects completed review at 12 weeks. There was no significant difference in any of the wound evaluation scores measured. There was a trend to improvement in cosmetic appearance in patients who received topical adhesive, as judged subjectively by the blinded plastic surgeon. There was no difference in adverse event rates between the two groups.
In conclusion, use of topical tissue adhesive for wound closure following permanent pacemaker implant was not superior to traditional closure techniques with absorbable sutures with regard to cosmetic outcome.
Introduction
Closure of the skin layers following pacemaker implantation is usually achieved with absorbable sutures. This can be time-consuming and does not always achieve perfect cosmetic results. Cyanoacrylate topical tissue adhesive has been used as an alternative but only limited data exist advocating routine use for pacing.1,2 We undertook a prospective randomised study to compare cosmetic outcomes with cyanoacrylate and absorbable sutures for this indication.
Methods
Consecutive patients aged ≥18 years requiring elective first pacemaker implant were recruited. Exclusion criteria were presence of dermatological disease, impaired wound healing, immunosuppressive agents or active infection. All patients provided written informed consent.
Pacemaker implant was undertaken as per standard practice by six experienced operators, under conscious sedation (midazolam ± fentanyl) shielding the patient’s face from the operative field. Following device implant, the pocket and middle layers were closed with polyglactin absorbable sutures (2/0 Vicryl™, Ethicon, USA). Once (and only if) adequate haemostasis had been achieved, the patient was randomised to skin closure either by topical tissue adhesive (Liquiband®, Medlogic Global Ltd., Plymouth UK) or by 3/0 poliglecaprone 25 subcuticular sutures (Monocryl™, Ethicon, USA). At procedure completion, an opaque sterile bio-occlusive dressing was applied. Wound assessment was performed at 12 weeks by a plastic surgeon blinded to the closure method using the Hollander and Vancouver wound evaluation scores and an analogue scar scale.3-5
Using pilot data, we calculated that a total of 76 patients (38 per group) would be required to detect a 15 mm improvement in the visual analogue scar score with a power of 90% and 5% significance. To allow for drop out, we aimed to recruit a minimum of 120 patients. Analysis was performed on an intention-to-treat basis using SPSS version 17.0.
Results
A total of 122 patients (mean age 77 ± 10.9 years, 66% male) were recruited. Ninety-five (77.8%) patients received a dual-chamber system. Fifty-eight (47.5%) patients were randomised to sutures, the remaining 64 (52.5%) patients were randomised to cyanoacrylate. Groups were well-matched for comorbidities (table 1).Total procedure duration (incision to skin closure) and incision length were similar in both groups. Skin layer closure time was shorter using cyanoacrylate – 117 (interquartile range [IQR] 92–136) versus 277 (IQR 231–311) seconds, p<0.001. Early complications were rare and unrelated to the closure method. There was no cross-over between either arm.
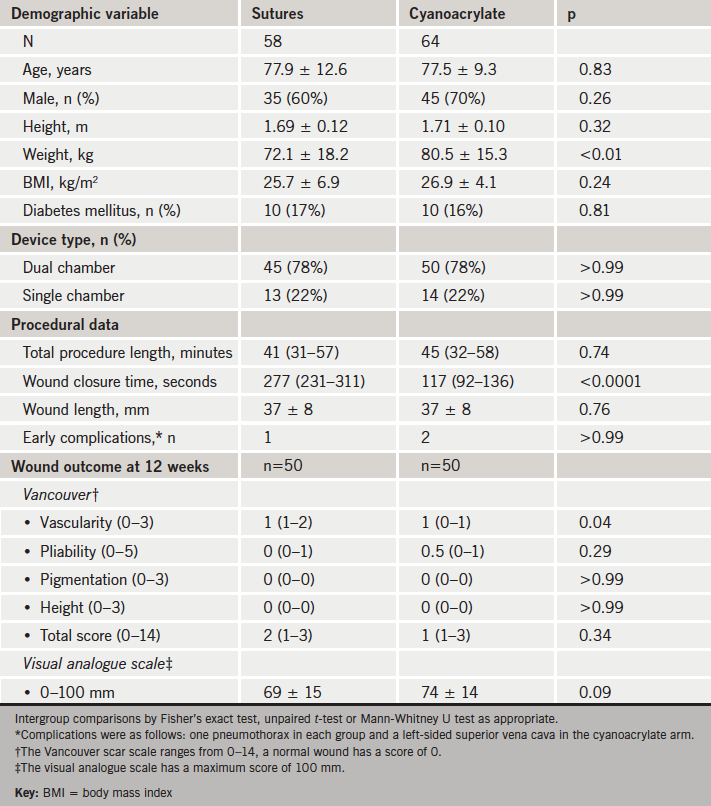
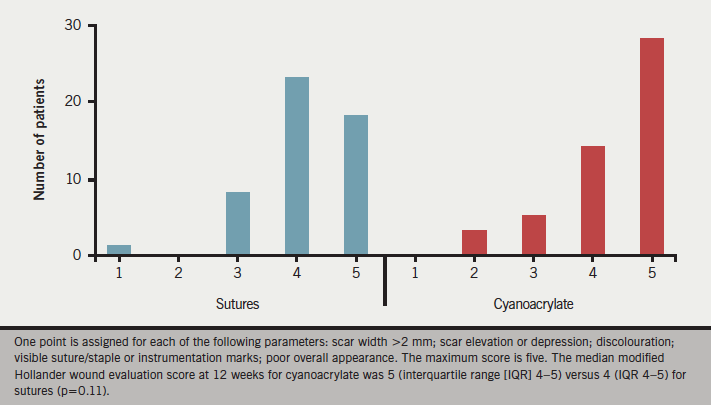
At six-week pacing clinic review the majority of wounds were graded as good – cyanoacrylate 50/53 (94%) and sutures 42/42 (100%), p=0.88. The three remaining wounds in the cyanoacrylate arm were considered suboptimal due to minor elevation or depression of the wound surface. No infections were noted. At 12-week follow-up, the median modified Hollander wound evaluation for cyanoacrylate was 5 (IQR 4–5) versus 4 (IQR 4–5) for sutures (p=0.11) (figure 1). Twenty-seven (54%) patients who received cyanoacrylate versus 18 patients (36%) who received sutures were considered to have an optimal scar (score of 5 on the score) (p=0.11). On the Vancouver scar scale, patients who had received cyanoacrylate had a median score of 1 (IQR 1–3) versus 2 (IQR 1–3) for sutures (p=0.34). Components of this scale were comparable between both arms, although cyanoacrylate seemed to produce wounds that were more vascular than sutures (p=0.04). Visual analogue scale assessment offered a mean score of 74 ± 14 mm for cyanoacrylate compared with 69 ± 15 mm for sutures (p=0.09). In the cyanoacrylate arm, 17/50 (34%) versus 10/50 (20%) were considered to be excellent (p=0.38). The remainder were graded as good. A number of patients failed to attend both six- and 12-week follow-up as they instead opted to be seen in community pacing clinics, thereby preventing formal wound evaluation. In all such cases, no concerns with wound healing were raised by the technical staff.
Discussion
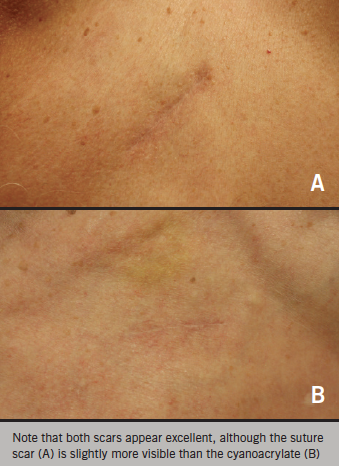
This study demonstrates that regardless of closure method employed, pacing wound appearances are generally good, and even where early healing may be suboptimal, this can improve further with time (figure 2). At formal 12-week evaluation there were no important differences between either closure method on the basis of the various (validated) wound assessment scores employed in this study. This is in contrast to other clinical settings, where cyanoacrylate has been shown to have better cosmetic outcome.6 The explanation for this disparity possibly relates to the nature of pacing, where scars are often of only short length (3–5 cm) and where limited instrumentation of the skin and underlying tissues is undertaken.
Wound complications of device implant are infrequent, but the consequences can be both unsightly (e.g. scarring) and devastating (e.g. pocket infection/erosion, sometimes necessitating device removal), all of which can relate to operator experience and procedure duration.7,8 Although the power of our study was clearly insufficient to detect a difference in rare events, data from other clinical settings suggest that cyanoacrylate offers a barrier against bacterial entry and is associated with lower rates of wound infection.9-12 This advantage was not clearly apparent in a separate prospective cardiac devices study, and it is, therefore, unknown whether cynoacrylate could be advantageous in reducing infection rates in this setting.2
Finally, although cyanoacrylate has potential for clinical advantage, the associated cost is greater. Within our institution, 3/0 poliglecaprone 25 subcuticular sutures (Monocryl™, Ethicon, USA) are procured for £2.04 and cyanoacrylate for £17.63 each. This equates to £15.59 additional cost per case – still modest compared with the overall procedural cost.
Conclusion
In this prospective, randomised study, skin closure with both closure methods produced excellent cosmetic results with no clear advantage for either technique. However, cyanoacrylate has a number of potential advantages, including rapid skin layer closure, and provides an impervious barrier potentially protective against bacterial entry.
Author contributions
T Watson and PJ Pugh co-designed the study, analysed the data and authored the paper; V Nayar, R Prasad, A Ladwiniec, I Rafiq and MRD Belham recruited patients, collected data and contributed to the manuscript; R Price evaluated the wounds and contributed to the manuscript.
Conflict of interest
None declared.
Key messages
- Both sutures and cyanoacrylate provide cosmetically pleasing
results - Wound closure with cyanoacrylate is a quick and effective method for skin closure
- Cyanoacrylate may offer a protective barrier to limit bacterial wound entry
- The cost of cyanoacrylate is modestly higher than use of sutures
References
1. Pachulski R, Sabbour H, Gupta R, Adkins D, Mirza H, Cone J. Cardiac device implant wound closure with 2-octyl cyanoacrylate. J Interv Cardiol 2005;18:185–7. http://dx.doi.org/10.1111/j.1540-8183.2005.04048.x
2. Spencker S, Coban N, Koch L, Schirdewan A, Mueller D. Comparison of skin adhesive and absorbable intracutaneous suture for the implantation of cardiac rhythm devices. Europace 2011;13:416–20. http://dx.doi.org/10.1093/europace/euq394
3. Hollander JE, Singer AJ, Valentine S, Henry MC. Wound registry: development and validation. Ann Emerg Med 1995;25:675–84. http://dx.doi.org/10.1016/S0196-0644(95)70183-4
4. Sullivan T, Smith J, Kermode J, McIver E, Courtemanche DJ. Rating the burn scar. J Burn Care Rehabil 1990;11:256–60. http://dx.doi.org/10.1097/00004630-199005000-00014
5. Quinn JV, Drzewiecki AE, Stiell IG, Elmslie TJ. Appearance scales to measure cosmetic outcomes of healed lacerations. Am J Emerg Med 1995;13:229–31. http://dx.doi.org/10.1016/0735-6757(95)90100-0
6. Coulthard P, Worthington H, Esposito M, Elst M, Waes OJ. Tissue adhesives for closure of surgical incisions. Cochrane Database Syst Rev 2004;(2):CD004287. http://dx.doi.org/10.1002/14651858.CD004287.pub2
7. Eberhardt F, Bode F, Bonnemeier H et al. Long term complications in single and dual chamber pacing are influenced by surgical experience and patient morbidity. Heart 2005;91:500–06. http://dx.doi.org/10.1136/hrt.2003.025411
8. Wiegand UKH, Bode F, Bonnemeier H, Eberhardt F, Schlei M, Peters W. Long-term complication rates in ventricular, single lead VDD, and dual chamber pacing. PACE 2003;26:1961–9. http://dx.doi.org/10.1046/j.1460-9592.2003.00303.x
9. Bhende S, Rothenburger S, Spangler DJ, Dito M. In vitro assessment of microbial barrier properties of dermabond topical skin adhesive. Surg Infect (Larchmt) 2002;3:251–7. http://dx.doi.org/10.1089/109629602761624216
10. Rocos B, Blom AW, Bowker K. Cyanoacrylate dressings: are they microbiologically impermeable? J Hosp Infect 2010;75:144–5. http://dx.doi.org/10.1016/j.jhin.2010.01.008
11. Souza EC, Fitaroni RB, Januzelli DM, Macruz HM, Camacho JC, Souza MR. Use of 2-octyl cyanoacrylate for skin closure of sternal incisions in cardiac surgery: observations of microbial barrier effects. Curr Med Res Opin 2008;24:151–5. http://dx.doi.org/10.1185/030079908X253807
12. Towfigh S, Cheadle WG, Lowry SF, Malangoni MA, Wilson SE. Significant reduction in incidence of wound contamination by skin flora through use of microbial sealant. Arch Surg 2008;143:885–91.http://dx.doi.org/10.1001/archsurg.143.9.885
