This is an audit of 10 Anglia region cardiac rehabilitation (CR) programmes against the British Association of Cardiovascular Prevention and Rehabilitation (BACPR) seven core standards. Methods included a questionnaire that encapsulated these standards, a SWOT (strengths, weaknesses, opportunities, threats) analysis and assessment of local outcomes.
Overall, all 10 CR services were compliant with the vast majority of basic standards set by BACPR but the audit also highlighted gaps in ideal care processes, such as a shortage of psychologists, occupational therapists and pharmacists, and inadequate audit processes. Local strengths were highlighted that will encourage future cross-pollination across the network. Outcomes were collected variably ad hoc but there was some consistency that CR across the region improved exercise tolerance, reduced anxiety and reduced smoking, but had little effect on blood pressure and body mass index, comparable to the national audit.
Anglia CR services were shown to be fit-for-purpose and there were local areas of excellence, but local areas of need and gaps in CR were highlighted that will cross-pollinate to improve all CR services in East Anglia.
Introduction

Cardiac rehabilitation (CR) services are comprehensive, long-term programmes involving medical evaluation, prescribed exercise, cardiac risk factor modification, education and counselling. CR has been extensively reviewed in the literature,1 and, in patients after myocardial infarction, has been shown to reduce all-cause and cardiovascular mortality rates in a Cochrane review.2 However, it has also been shown by others to have little effect on outcomes.3
Doubts over the efficacy of CR have led commissioners to question the value of such services. While the debate continues, the Anglia region CR services (rebooted last year as the Alliance of Cardiac Rehabilitation Anglia Network [ACRAN] under new consultant cardiologist leadership) set out to, not only audit their services against a contemporary standard, but also to identify local areas of good practice for communal learning and service development. We sought to reassure commissioners and patients of the need and utility of CR. The British Association of Cardiovascular Prevention and Rehabilitation (BACPR) has previously prescribed the standards of what a CR programme should entail in its 2012 publication in which seven core standards are set out,4 and it was this standard we measured ourselves against.
This is the first audit of all CR services presented in this way in this region, and this paper summarises the results of the audit presented as a half-day meeting organised by the East of England Clinical Network. There are 11 CR services across the Anglia region, of which 10 took part in this audit.
Methods
Audit of current services
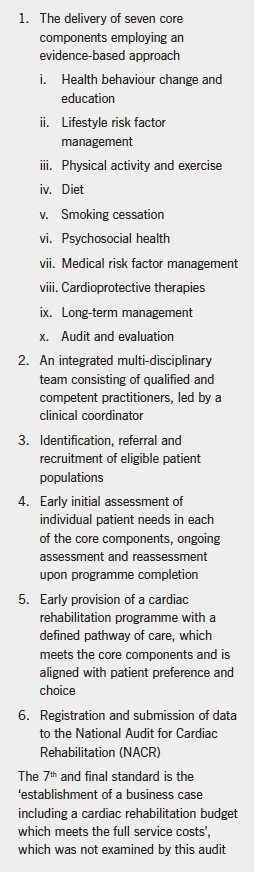
A questionnaire was devised that encapsulated standards 1–6 of the BACPR 2012 document and was sent out to all CR service leads. This was designed by ACRAN Lead Consultant Cardiologist Dr Justin Zaman and edited by Jo Haywood, lead ACRAN CR Healthcare Professional and nurse at the Norfolk and Norwich University Hospital. For each standard, relevant questions were designed. The standards are listed in box 1.
The Anglia CR network local strengths
This part of the audit allowed each CR service to present briefly on their own services, to allow specialist skills and local issues to be aired. Such granularity would not be possible with the main regional audit presented above. The general format of each presentation was a SWOT (strengths, weaknesses, opportunities, threats) analysis followed by highlighting of a particular skill of that service, and if applicable, a patient case history or testimonial to give qualitative detail to the dry quantitative audit presented above.
Outcome data and future challenges
We, as a region, further looked at local outcomes that individual services collected – not all services can input into the national audit funded by the British Heart Foundation and run by the University of York and the UK government’s Health and Social Care Information Centre (National Audit of Cardiac Rehabilitation, NACR). We looked at data from 1 April 2014 to 30 September 2014 (quarters 1 and 2) for all 10 services. In particular, we looked at outcome data showing changes in physical activity, psychological health, behaviours like smoking, and also biological parameters, such as weight loss and change in blood pressure.
Results
Audit of current services
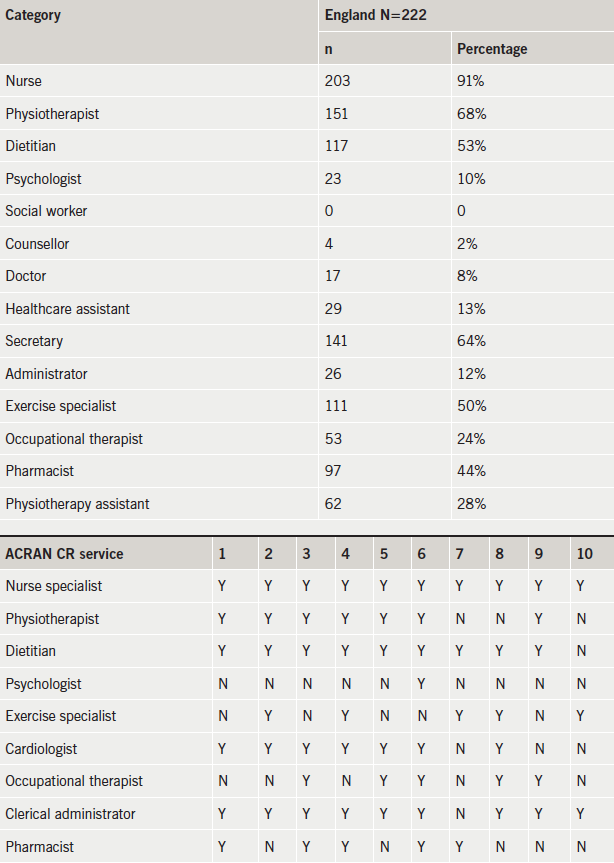
The results from these CR services are presented in tables. Table 1 shows that there was a tendency for a shortage of psychologists, occupational therapists and pharmacists in CR teams (BACPR stipulate an ideal CR team needs a cardiologist/community cardiologist/physician or general practitioner with special interest, nurse specialist, physiotherapist, dietitian, psychologist, exercise specialist, occupational therapist and clerical administrator) – however, most teams had a nurse, physiotherapist/exercise specialist and also administrative support.
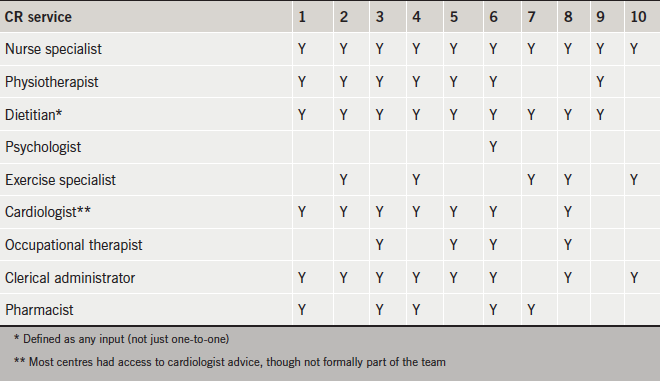
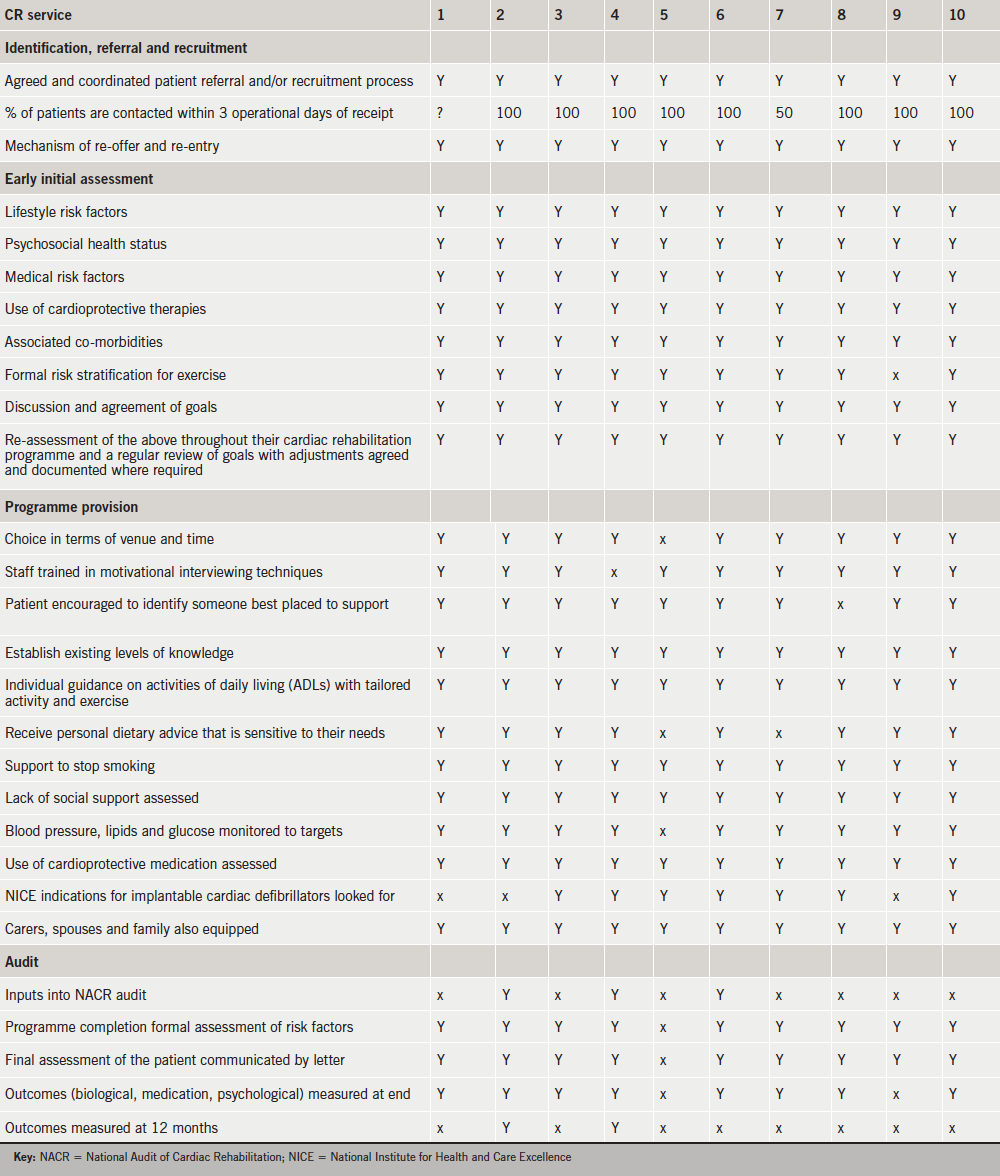
Table 2 shows the results of the main body of the audit.
- There was a region-wide excellence in the identification and referral process, with very quick initial contact of patients as emphasised strongly in BACPR guidance. The audit did not assess which types of patient group were eligible as that was specific to the centre (for example tertiary centres had more non-ischaemic patients, e.g. valve disease, dilated cardiomyopathy). Only one centre had a cultural issue with a reasonably high proportion of South Asian patients, and the way in which this was dealt with is discussed further below.
- Early initial assessment was excellent in all centres, with a thorough initial appraisal evident in all, a prerequisite to a patient-centred approach. BACPR state that “a formal assessment of lifestyle risk factors (smoking, diet and physical activity), psychosocial health status, medical risk factors (blood pressure, lipids and glucose) and use of cardioprotective therapies” is needed, and all centres follow these guidelines. All services set goals, and most did risk stratification.
- Programme provision was very good – the region’s CR programmes demonstrated a great deal of flexibility in their services (e.g. in terms of times and venues of CR programmes), as well as the broad-based approach recommended in CR, with lots involving family/carers. Audit was patchier, with only a minority of centres contributing to the national audit – feedback was that this was mostly down to an issue of time and lack of administrative skills, most CR services felt they were not resourced for this, but more for programme delivery.
Overall, all 10 CR services were compliant with the vast majority of basic standards set by BACPR. In particular, all 10 services were able to demonstrate that they were delivering the seven core components of cardiac rehabilitation, though more work was needed to ensure all were able to fully deliver the final component, audit and evaluation.
The Anglia CR network local strengths
Exercise specialist
One hospital had a highly individualised approach, particularly in activity. It chooses to employ an exercise specialist, rather than a physiotherapist, to focus, it argues, on health, not illness. The exercise prescription is novel within the Anglia region, and tailored to each patient.
Low impact class
Another service offered a low-impact class that extends out to those patients who would not normally have come to traditional exercise classes – this broadens the inclusion criteria when resources are limited towards providing a more generic service to the cardiac population.
Psychological rehabilitation
Another two services reminded all those involved in CR that broad outcome data can only say so much. One highlighted the case of a 70-year-old man who, after his heart attack, suffered so emotionally that he purchased a sofa bed and commode as he felt unable to climb stairs, and he was even unwilling to lift his head from the pillow. He would not even attend for the coronary angiogram. With much CR effort and education, GP review, help from a local hospice and careful liaison with his consultant cardiologist with regards to timing and logistics of his angiogram, he made it through the angiogram and at six-month follow-up was found to be doing very well and walking for half a mile with only slight breathlessness, as well as being free from anginal symptoms. On a 12-month audit sheet of ‘hard’ data, this would reveal little of the extensive multi-disciplinary work that was undertaken by the CR team and others to fully rehabilitate this patient after his heart attack, a time-consuming but ultimately highly rewarding care process. One CR service uniquely provides a cognitive behavioural therapy (CBT) service. Overall, however, the lack of formal psychological service support was highlighted.
Social inequality
One service was relatively unique in the area having a high ethnic (South Asian) population, a population that is known to have a higher burden of cardiac disease but often less access to cardiac services.5 However, this CR service maintained a very high proportionate uptake among ethnic groups (e.g. by using specially trained healthcare professionals of South Asian background) and, thus, was able to avoid potential local health inequalities in using specialist services to ensure equitable uptake of CR.
Phase 4 classes
Another service presented their follow-on exercise class after the CR programme with the local council. It was initially funded from the Academic Health Science Network which piloted a Phase 4/follow-on class for patients. Funding was then continued from the council for this follow-on class, which had been oversubscribed from the start.
Education exhibition
One service has been running an Education Exhibition since April 2011; they wanted to target a wider group of patients and partners that would not traditionally receive education, i.e. heart failure, patients awaiting intervention (valve surgery, bypass surgery, complex pacing, angina). Every eight weeks they invite patients and partners to attend the event, held in their Hospital Education Centre. British Heart Foundation (BHF) literature and magazines are available for patients to take away near the refreshments. They also have information regarding erectile dysfunction and place some of these in the men’s toilets. They have two projector screens playing educational videos, so patients and partners can sit and watch while drinking coffee, and waiting for the next health professional to become available. Health professionals that attend are: pharmacist, dietitian, occupational therapist, smoking cessation advisor (level 3) (also targets partners and passive smoking), UPBEAT (patient support group), cardiac rehab nurse specialists/cognitive behavioural therapist and physiotherapist.
Community services
Two community-based CR services exist within Anglia, and allow these patients to access a CR programme nearer to home. Home visiting is also possible, and community venues aid accessibility and increase uptake. These CR services are particularly flexible, even offering evening classes to aid accessibility. Strong links with community cardiac support groups also exist, and they work in partnerships with Phase 4 exercise instructors based in the communities, for instance through the local council.
Menu-based services
One CR service from a tertiary centre offered a menu-based, flexible, inclusive programme. In addition to an in-house programme offering three levels of exercise, there is a home-based programme for those who cannot attend the usual CR programme – these patients get an initial assessment via telephone or email, and then patients are given a diary and DVD, heart rate monitor or pedometer depending on their needs. Weekly telephone calls/emails are planned for the first six weeks, then at nine weeks and a final assessment (can be visit or telephone call) at 12 weeks, with an education topic for each weekly call to cover what would be traditionally done at group education. This home programme enables patients to complete a CR programme if returning to work, have transport issues or simply that they do not wish to exercise as part of a group. It even allows patients to continue on the programme if they live or plan to travel overseas (recent patients on this programme have lived in Spain, Portugal, Hong Kong, Oman and Australia).
Outcome data and future challenges
We found that outcomes were collected variably (no standard agreement for instance on best physical activity variable), and ad hoc across the region. Some services collected no outcomes at all. This was mostly down to lack of time and resources (personnel and financial) to collect either local outcomes, let alone input into the national audit. The practitioners fed back that CR services were not set-up to audit themselves, as they focus on delivering the actual care process. We were unable to compare clinical outcomes pre- and post-programmes in a formal and consistent manner, but there was some consistency from locally collected before-and-after data (available on request) that CR across the region improved exercise and anxiety, reduced smoking but had little effect on blood pressure and body mass index. We compared our regional results with the NACR audit and found many similarities, in particular that CR over a 12-week period impacted mostly on physical activity, smoking cessation and, to a degree, psychological health (though the latter depends on baseline levels of anxiety – as illustrated in the individual case examples above, CR can be very effective in very anxious patients) – there was less impact on weight. Our levels of staffing regionally, also looked remarkably similar to national figures (box 2). Using questionnaires and testimonials that local services collected, overall patient satisfaction was very positive overall.
Discussion
We have conducted a comprehensive and rigorous audit across the region to establish a baseline position from BACPR standards. We present data that show that all our region’s CR services met the vast majority of the exacting standards in the BACPR standards publication. By conducting this survey in the way we have (driven by a consultant cardiologist who is not directly involved in CR delivery), we have stood back from our services. The rebooting of our network into an Alliance has led to us working more collaboratively than ever before, and in the process of this audit (one that took one year to plan and do), we have succeeded in terms of cross-pollination of knowledge. We used the same care process benchmarking tool (BACPR) across the network to ensure consistency of approach across all services and this helps to standardise services across the patch – what we lacked were consistent outcome measures. By presenting these data at an open-invite East of England Clinical Network organised meeting, we consulted with and incorporated views from all key stakeholders – the day’s attendees included consultant cardiologists, cardiac service managers, commissioners, clinical leads from neighbouring regions, senior academics (a professor of nursing and a professor of public health), and patient representatives. We aspire to include commissioners further in plans for future service redesign.
Strengths and weaknesses
We accept this is a self-completed audit by the CR practitioners themselves. The audit questionnaire was broad and pragmatic, given the time constraints of the practitioners, and the variation of services across the region. It sought mostly to demonstrate, to any interested outside observers or internal commissioners, the degree to which local services conformed to broad standards as taken from BACPR. The other key issue was to highlight gaps, and it did highlight areas of deficiency, which though few, had a degree of consistency across the region (e.g. in lack of certain types of healthcare professional, lack of audit). We acknowledge that this was not a clinical trial seeking to counter-balance recent research suggesting CR is not effective, and for that, we would look to future large, multi-centre CR randomised trials that examined outcomes in standard CR against another care pathway following myocardial infarction.
Conclusion
We show here that CR services within the Anglia region of the East of England are fit-for-purpose and we present local areas of excellence for wider learning for others; we also highlight local areas of need and gaps in CR that we will cross-pollinate to improve all CR services in East Anglia. Whether or not the current format of CR is valid remains up for debate, and research is needed into whether a more flexible and tailored approach6 is of greater benefit to this population. CR is likely to continue to get more referrals as survival improves quicker than incidence falls. The indications for CR will further broaden (e.g. into angina, heart failure, post-surgical) and there remain a lot of patients that do not attend, often the ones who really need CR.7 EUROASPIRE (European Action on Secondary and Primary Prevention through Intervention to Reduce Events) shows secondary prevention behaviour change outcomes remain very poor8 and, thus, given all this, CR remains the vital other ‘bookend’ to coronary care, a continuous pathway of care for a condition, which usually starts with the patient with chest pain calling for an ambulance.
Acknowledgement
The ACRAN team would like to thank Delyth Williams (Quality Improvement Lead, Strategic Clinical Networks – Cardiovascular, NHS England, East Anglia Area Team) for providing the infrastructure and support to be able to present our audit idea and subsequent results to all interested parties in the region. Without her, this work would not have been given the platform it ultimately was.
Conflict of interest
None declared.
Key messages
- British Association of Cardiovascular Prevention and Rehabilitation (BACPR) espouses seven core standards for cardiac rehabilitation (CR)
- In this audit, all 10 CR services in Anglia were compliant with the vast majority of basic standards set by BACPR
- The audit highlighted gaps in multi-disciplinary staff (psychologists, occupational therapists and pharmacists) and audit
- Local strengths were highlighted that will encourage future cross-pollination across the network
- CR across the region improves exercise tolerance, reduces anxiety and reduces smoking, but had little effect on blood pressure and body mass index, comparable to the national audit
References
1. Mampuya WM. Cardiac rehabilitation past, present and future: an overview. Cardiovasc Diagn Ther 2012;2:38–49. http://dx.doi.org/10.3978/j.issn.2223-3652.2012.01.02
2. Heran BS, Chen JMH, Ebrahim S et al. Exercise-based cardiac rehabilitation for coronary heart disease. Cochrane Database Syst Rev 2011;(7):CD001800-CD. http://dx.doi.org/10.1002/14651858.cd001800.pub2
3. West RR, Jones DA, Henderson AH. Rehabilitation after myocardial infarction trial (RAMIT): multi-centre randomised controlled trial of comprehensive cardiac rehabilitation in patients following acute myocardial infarction. Heart 2012;98:637–44. http://dx.doi.org/10.1136/heartjnl-2011-300302
4. British Association for Cardiovascular Prevention and Rehabilitation. The BACPR Standards and Core Components for Cardiovascular Disease Prevention and Rehabilitation 2012. London: BACPR, 2012. Available from: http://www.bacpr.com/resources/46c_bacpr_standards_and_core_components_2012.pdf
5. Zaman MJ, Philipson P, Chen R et al. South Asians and coronary disease: is there discordance between effects on incidence and prognosis? Heart 2013;99:729–36. http://dx.doi.org/10.1136/heartjnl-2012-302925
6. Redfern J, Maiorana A, Neubeck L, Clark AM, Briffa T. Achieving coordinated secondary prevention of coronary heart disease for all in need (SPAN). Int J Cardiol 2011;146:1–3. http://dx.doi.org/10.1016/j.ijcard.2010.08.046
7. Mosleh S, Campbell N, Kiger A. Improving the uptake of cardiac rehabilitation – redesign the service or rewrite the invitation. Br J Cardiol 2009;16:57–9. Available from: https://bjcardio.co.uk/2009/03/improving-the-uptake-of-cardiac-rehabilitation-redesign-the-service-or-rewrite-the-invitation/
8. Kotseva K, Wood D, De Backer G et al. EUROASPIRE III. Management of cardiovascular risk factors in asymptomatic high-risk patients in general practice: cross-sectional survey in 12 European countries. Eur J Cardiovasc Prev Rehabil 2010;17:530–40. http://dx.doi.org/10.1097/HJR.0b013e3283383f30
