Reflex syncope is the most common cause of transient loss of consciousness. Practical manoeuvres may help, but additional measures are often required. In our experience, midodrine gives consistently good results in patients with reflex syncope. This study also provides reassurance that the effect on blood pressure is measureable, but small, and side effects are infrequent. UK prescribing may have been limited when midodrine was unlicensed, but midodrine is now licensed.
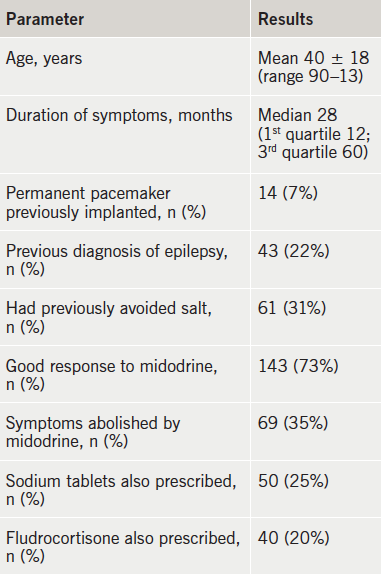
We treated 195 patients, age 40 ± 18 years, 72 (37%) aged under 30 years, 151 female (78%), who attended a Rapid Access Blackouts Triage Clinic and gave a clear history of reflex syncope. The median duration of symptoms was 28 months. A misdiagnosis of epilepsy had occurred in 39 patients and 42 had significantly low blood pressure.
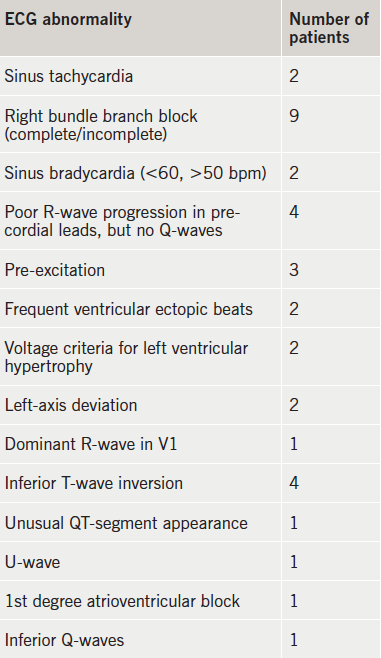
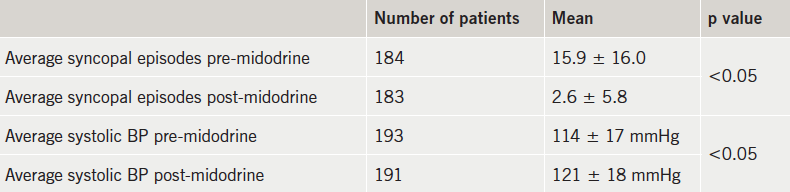
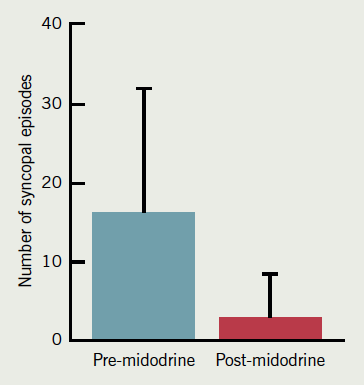
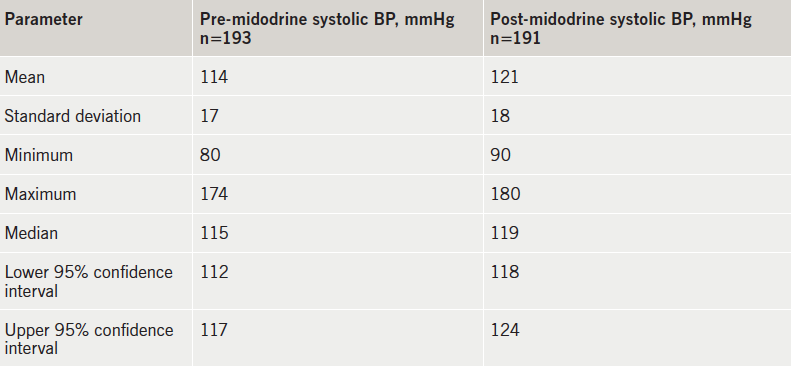
Follow-up was 50 ± 42 months in 184 patients (93%), with 11 patients lost to follow-up. Twenty-eight patients had minor electrocardiogram (ECG) changes but had a normal echocardiogram. Overall, 143 (73%) patients improved on a mean dose of 10 mg a day of midodrine. Syncopal events fell from 16 ± 16 to 2.6 ± 5 per six months (p<0.05), and in 69 (35%) patients, syncope was eradicated. Nineteen (10%) patients were able to stop midodrine after 52 ± 42 months due to symptom resolution. Fifteen patients (7%) stopped midodrine because of side effects, while 17 (8%) patients failed to respond. Mean supine systolic blood pressure rose from 114 mmHg to 121 mmHg at final midodrine dose (p<0.05).
In conclusion, in patients with reflex syncope, midodrine shows clinical benefit in greater than 70%, with 24% having complete symptom resolution. Side effects are rare, and there is little evidence of a hypertensive effect.
Introduction
‘Collapse_?cause’ is common in primary and secondary care, with most cases precipitated by transient loss of consciousness (T-LOC, or blackout). Many patients with T-LOC suffer long delays and errors in risk assessment, diagnostic testing, and specialist referral. Syncope has a pronounced health and economic impact, causing 3–5% of emergency room visits and 1–3% of hospital admissions.1 Reflex syncope is by far the most common cause of syncope. The European Society of Cardiology (ESC) has defined syncope as “T-LOC due to transient global cerebral hypoperfusion characterised by rapid onset, short duration and spontaneous complete recovery”; and reflex syncope results from “impairment of cardiovascular reflexes that are normally useful in controlling the circulation”.2 The ESC guidelines recommend non-pharmacological measures as first-line treatment, which include emphasising fluid and salt intake, regular exercise and physical counter-pressure manoeuvres.3 These are effective in some cases. However, symptoms may persist and be disabling, and further treatment may be needed. Commonly used drugs are beta blockers and fludrocortisone. However, both treatments have been found to be ineffective in recent trials.4,5 Midodrine, an alpha-adrenergic agonist, has been used in patients who are not responding to non-pharmacological treatments.3,6 However, less is known about midodrine treatment, particularly in younger patients with reflex syncope versus older patients with orthostatic hypotension.7 Furthermore, midodrine was not being prescribed as it was unlicensed, but this has recently changed. The Food and Drugs Administration (FDA) has previously tried to unlicense midodrine (2010 http://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/2010/ucm222580.htm). The ESC has recommended midodrine, but only as a class IIa indication.2 Information on when, why and how to prescribe midodrine in order to get good results without side effects is needed.
Methods
We report a single-centre experience of midodrine in patients with reflex syncope, no clinical ‘Red Flags’, and a normal or near-normal electrocardiogram (ECG). These ‘Red Flags’ include five cardiac features (abnormal 12-lead ECG, family history of sudden cardiac death <40 years, significant structural heart disease, T-LOC during exercise, new/unexplained shortness of breath) and three neurological features (history of brain injury, history strongly suggestive of epilepsy, new or evolving neurological deficit). Patients with near-normal/abnormal ECG underwent an echocardiogram. Patients attended a Rapid Access Blackout Triage Clinic (RABTC). Specialist nurses in arrhythmia, falls and epilepsy assessed patients using a web-based blackouts assessment tool (demo at: http://www.manchesterheartcentre.org/blackouts/), which included a risk assessment for ‘Red Flag’ features. Medical overview was provided by a cardiologist. A large proportion of patients had a diagnosis of reflex syncope based on history, examination and normal ECG. Initial management strategies for these patients included lifestyle modification, adequate fluid and salt supplementation and counter-pulsation manoeuvres.8,9 Patients with continuing syncope were offered midodrine as first-line treatment.
Midodrine is an alpha-adrenoceptor agonist and increases arteriolar tone at skeletal muscle arterioles. It is assumed that this action inhibits the abrupt loss of tone in these arterioles when sympathetic outflow is suddenly shut off at the onset of a reflex syncopal attack. Blood pressure can be shown to rise during midodrine treatment.10 Midodrine has been unlicensed in the UK, and was only prescribed on a named-patient basis. Although it has recently been licensed, it is still being prescribed in a similar way because of lack of expertise. There is a hope, with more experience and evidence, like our paper, it will be widely prescribed when required.
In the USA, the FDA has tried to unlicense the drug due to lack of evidence of efficacy, and concerns about a hypertensive response. This caused widespread protests from patients. As a result the FDA issued an update, confirming that midodrine “remains approved and available in the marketplace” (http://www.fda.gov/Drugs/DrugSafety/ucm225444.htm). However, there is currently no good evidence to support its use in reflex syncope, particularly in younger patients, and no evidence that shows a reduction in spontaneous episodes of syncope in reflex syncope patients.
Patients
We analysed our use of midodrine in 195 consecutive patients with reflex syncope seen in our RABTC over 10 years. Reflex syncope was diagnosed clinically from a history of syncope, and recognised features of reflex syncope. Most such patients had a normal or near-normal 12-lead ECG. No cardiac ‘Red Flags’ were present to suggest a cardiac or arrhythmic cause of syncope, nor neurological ‘Red Flags’ that might suggest a diagnosis of epilepsy. In some cases, we assessed patients with a previous diagnosis of epilepsy. In these cases, lack of response to multiple epilepsy drug trials had placed that diagnosis in doubt, and a new diagnosis of convulsive syncope had been made. In some patients there were minor ECG abnormalities, these all had normal echocardiography, and the clinical diagnosis of reflex syncope was convincing.
Treatment
Patients with reflex syncope were advised to increase fluid and salt intake and practice other non-pharmacological measures, as above. The number of syncopal episodes and the duration of symptoms, along with lying and standing blood pressure, were recorded. Those who continued to have episodes of reflex syncope were prescribed midodrine as a first-line drug treatment. If patients had already tried fluid and salt, midodrine was prescribed at their initial consultation. The usual starting dose was 2.5 mg three times daily. Regular blood pressure monitoring was arranged. Side effects, such as tingling and numbness of the scalp, were explained. Evening doses were prescribed a few hours prior to sleep in order to avoid supine hypertension. Patients were advised to avoid midodrine in pregnancy, if possible. Regular follow-up assessed symptoms and side effects. Response to medication was assessed by the number of syncopal episodes and by blood pressure. Gradual increments in dose were made, up to a maximum of 15 mg three times daily, depending upon response. Patients were told to stop treatment if unbearable side effects occurred, and contact the centre.
Data collection and analysis
Data were collected from the electronic database and case notes, and prepared for a descriptive analysis. Syncope rates before and after midodrine were compared. The primary end point of the study was the difference in number of syncopal episodes before and after midodrine. These were assessed at follow-up visits and documented in study notes. These are then compared with the frequency of syncopal episodes pre-midodrine. Using SPSS software, non-parametric tests were used for descriptive analysis. Associated significance values were based on Wilcoxon signed-rank test.
Results
Effect on rate of syncope
We treated 195 patients, who were predominantly female (n=151, 78%). The age range was 13–90 (mean 40 ± 18) years. Seventy-five patients were under 30 years of age (37%). Patient characteristics are given in table 1. Sixty-one patients (31%), seen with reflex syncope, had been avoiding salt because of an over-zealous response to public health messages, and responded to salt supplementation alone, and are not included in the midodrine treatment data.
abnormalities
All patients had had syncope. The duration of symptoms prior to RABTC assessment varied from four to 300 months. Thirty-nine patients had previously been diagnosed with epilepsy and treated with anticonvulsants to which there had been no response, resulting in referral to the RABTC. Anticonvulsants were weaned off in these patients before midodrine was commenced.
Follow-up data were available for 184 patients (93%), while 11 were lost to follow-up. One hundred and fifty-six patients had a normal ECG (ECG abnormalities in 35 patients are shown in table 2).
There was improvement in symptoms in 143 patients (73%) treated with midodrine titrated upwards from 2.5 mg three times a day. The mean daily total dose of midodrine was 10 mg. Sixty-nine (35%) patients had complete resolution of symptoms. A quarter (24%) of patients were already taking salt supplements as sodium chloride tablets. Forty patients (20%) had taken fludrocortisone without improvement. Nineteen patients (13% of responders) were able to stop treatment when symptoms resolved completely after 52 ± 42 months of treatment. Fifteen patients (7%) could only tolerate the starting dose of midodrine (2.5 mg three times daily), 20 of 41 non-responders had to stop midodrine because of side effects. Seventeen patients (9%) had no response at all. Results are expanded in table 3 and figure 1.
pressure (BP) pre- and post-midodrine per 6 months
syncopal episodes pre- and post-midodrine per 6 months
Effect of midodrine on blood pressure
We measured the effect of midodrine on blood pressure. As discussed above, all patients had measurement of blood pressure at the start of midodrine with subsequent regular monitoring. Mean systolic blood pressure rose from 114 mmHg to 121 mmHg with midodrine treatment (tables 3 and 4).
Discussion
The management of reflex syncope can be difficult. Patient education is important, especially when there is a constant public health message warning against salt intake, in spite of the fact that salt is an essential component of a healthy diet. Counter-pulsation measures and the avoidance of prolonged standing may be useful,3 but only if there is sufficient warning before an attack. While reflex syncope seems to be benign, the risk of accidents and injuries is clear, and counter-pulsation may be ineffective if there is little warning before syncope. Patients should be informed about the mechanism and importance of recognising warning signs so that chances of injuries can be avoided. However, there is currently no treatment for reflex syncope that has been proven conclusively in a double-blind, randomised, placebo-controlled trial. Many treatments have been advocated, and volume expansion has been the foundation of treatment, with increased dietary salt and fluid intake.
Among prescription drugs for volume expansion, fludrocortisone is widely used, especially in younger patients. However, the Second Prevention of Syncope Trial (POST II)5 found no benefit from fludrocortisone when used as monotherapy for reflex syncope. Beta blockers are widely prescribed in reflex syncope but the evidence for benefit is scant. It is thought that beta blockers reduce myocardial inotropy. This then prevents the stimulation of left ventricular mechanoreceptors culminating in a Bezold-Jarisch reflex, which is thought to be responsible for triggering reflex syncope. They might also block the effects on inotropy of increases in circulating adrenaline, and blunt the heart rate increase prior to sympathetic withdrawal and syncope in many patients. However, conclusive evidence for all these theoretical effects in humans is missing. The majority of studies of beta blocker therapy in reflex syncope have been open-label and not blinded.11 Furthermore, where trial design includes randomisation and placebo-control, outcomes have only been measured in terms of reduction in the number of positive tilt tests. However, the reproducibility of tilt-table testing is well known to be poor, and hampers its use both in diagnosis and in the assessment of treatments.12,13 There are currently no studies comparing the rate of syncope before treatment with the rate of syncope on treatment. In other studies, follow-up periods have been very short. Metoprolol, pindolol, propranolol, esmolol and atenolol have all shown benefit in uncontrolled studies, but, again, benefit was reliant on repeat tilt-testing in the majority of these, not long-term symptom review. In contrast, two reports show no benefit, with one describing worsening of symptoms on atenolol treatment. Metoprolol was studied in the randomised, placebo-controlled, double-blinded, multi-centre POST trial,4 and this showed no benefit in prevention of long-term syncope recurrence. Despite the attractiveness of the pathophysiological rationale for beta-blocker therapy in reflex syncope, as well as safety and relative tolerability, there is no good evidence in their favour.
Other trials compared a variety of pharmacological therapies, including scopolamine, clonidine, cafedrine, domperidone, dihydroergotamine and disopyramide, and found no differences between placebo and treatment arms. Theophylline can antagonise adenosine receptors shown to mediate vasodilatation. It has also been tested in two small, uncontrolled studies showing modest benefit.14 An abnormally hypersensitive serotonin response within the central nervous system has been suggested as the cause of reflex syncope. Different studies have trialled selective serotonin reuptake inhibitors in reflex syncope. One randomised trial showed reduced syncope recurrence in 30 patients taking active medication compared with placebo,15 a subsequent study showed no benefit.16
Kaufmann et al.,17 in 2002, studied the effect of midodrine in 12 patients with recurrent neutrally mediated syncope and found it to be beneficial in improving orthostatic tolerance during head-up tilt, but without long-term symptom review. Another study18 also recommended midodrine in extremely symptomatic patients, but follow-up was only for one month. A beneficial effect of midodrine in paediatric patients has been claimed,19 but outcomes were based on tilt-test responses, and bias was introduced by addition of fludrocortisone therapy. In another study,20 midodrine had a good effect, but it was open-labelled. Romme et al. (STAND trial)21 found no added beneficial effect over non-pharmacological treatment. Doyle et al.22 also studied its efficacy comprehensively. A multi-centre, international, randomised, placebo-controlled trial (POST 4) is in progress to study the role of midodrine in vasovagal syncope.23 However, there will be no guidance for physicians looking after patients with troublesome reflex syncope for several years from this trial. Meanwhile, many patients with severely limiting symptoms of recurrent syncope may be denied effective treatment. This is especially the case in the UK where midodrine has been unlicensed, although things have changed recently.
This study found that midodrine gave a statistically significant benefit in over 70% of our patients, and complete resolution of syncope in 35%. Syncope rates fell very significantly. There was a clearly defined group who could not tolerate midodrine, and a group whose symptoms resolved completely. At the same time, there were no instances of a hypertensive response to treatment. Mean systolic blood pressure rose by a small but significant amount. The study end point was not dependent on tilt-test responses, which are unreliable. In the current absence of large, randomised, clinical trials, our retrospective analysis provides beneficial evidence in reflex syncope. If simple lifestyle measures, avoidance of precipitating circumstances, and salt and fluid supplementation prove to be inadequate; midodrine can be effective in some patients.
Acknowledgement
AA was funded by a grant for his research post by Medtronic Inc.
Conflict of interest
AA was in receipt of salary support from Medtronic UK during his research fellowship from 2013 to 2015.
Key messages
- Reflex syncope is the most common cause of transient loss of consciousness
- Simple measures like fluid and salt supplementation are the mainstay of treatment. Some patients with recurrent and frequent episodes require more than fluid and salt
- No drug treatment has been proven beneficial so far
- Midodrine can be helpful, but evidence is lacking
- In the absence of randomised-controlled trials, our study provides evidence of its efficacy
- Midodrine has been unlicensed, but this status has changed recently.
References
1. Savage DD, Corwin L, McGee DL, Kannel WB, Wolf PA. Epidemiologic features of isolated syncope: the Framingham Study. Stroke 1985;16:626–9. http://dx.doi.org/10.1161/01.STR.16.4.626
2. Task Force for the Diagnosis and Management of Syncope, European Society of Cardiology (ESC), European Heart Rhythm Association (EHRA) et al. Guidelines for the diagnosis and management of syncope (version 2009). Eur Heart J 2009;30:2631–71. http://dx.doi.org/10.1093/eurheartj/ehp298
3. Benditt DG, Nguyen JT. Syncope: therapeutic approaches. J Am Coll Cardiol 2009;53:1741–51. http://dx.doi.org/10.1016/j.jacc.2008.12.065
4. Sheldon R. Prevention of Syncope Trial (POST): a randomized, placebo-controlled study of metoprolol in the prevention of vasovagal syncope. Circulation 2006;113:1164–70. http://dx.doi.org/10.1161/CIRCULATIONAHA.105.535161
5. Raj SR, Rose S, Ritchie D, Sheldon RS, POST II Investigators. The Second Prevention of Syncope Trial (POST II): a randomized clinical trial of fludrocortisone for the prevention of neurally mediated syncope: rationale and study design. Am Heart J 2006;151:1186.e11–1186.e17. http://dx.doi.org/10.1016/j.ahj.2006.03.013
6. Kuriachan V, Sheldon RS, Platonov M. Evidence-based treatment for vasovagal syncope. Heart Rhythm 2008;5:1609–14. http://dx.doi.org/10.1016/j.hrthm.2008.08.023
7. Jankovic J, Gilden JL, Hiner BC et al. Neurogenic orthostatic hypotension: a double-blind, placebo-controlled study with midodrine. Am J Med 1993;95:38–48. http://dx.doi.org/10.1016/0002-9343(93)90230-M
8. Wieling W, Colman N, Krediet CT, Freeman R. Nonpharmacological treatment of reflex syncope. Clin Auton Res 2004;14(suppl 1):62–70. http://dx.doi.org/10.1007/s10286-004-1009-x
9. Claydon VE, Hainsworth R. Salt supplementation improves orthostatic cerebral and peripheral vascular control in patients with syncope. Hypertension 2004;43:809–13. http://dx.doi.org/10.1161/01.HYP.0000122269.05049.e7
10. Low PA, Gilden JL, Freeman R, Sheng KN, McElligott MA. Efficacy of midodrine vs placebo in neurogenic orthostatic hypotension. A randomized, double-blind multicenter study. Midodrine Study Group. JAMA 1997;277:1046–51. http://dx.doi.org/10.1001/jama.1997.03540370036033
11. Natale A, Newby KH, Dhala A, Akhtar M, Sra J. Response to beta blockers in patients with neurocardiogenic syncope: how to predict beneficial effects. J Cardiovasc Electrophysiol 1996;7:1154–8. http://dx.doi.org/10.1111/j.1540-8167.1996.tb00494.x
12. Fitzpatrick A, Sutton R. Tilting towards a diagnosis in recurrent unexplained syncope. Lancet 1989;333:658–60. http://dx.doi.org/10.1016/S0140-6736(89)92155-7
13. Pavri BB, Ruskin JN, Brooks R. The yield of head-up tilt testing is not significantly increased by repeating the baseline test. Clin Cardiol 1996;19:494–6. http://dx.doi.org/10.1002/clc.4960190610
14. Natale A, Sra J, Dhala A et al. Efficacy of different treatment strategies for neurocardiogenic syncope. Pacing Clin Electrophysiol 1995;18:655–62. http://dx.doi.org/10.1111/j.1540-8159.1995.tb04660.x
15. Di Girolamo E, Di Iorio C, Leonzio L, Sabatini P, Ranalli G, Barsotti A. [Effectiveness of paroxetine in the treatment of refractory vasovagal syncope in young patients]. G Ital Cardiol 1999;29:1472–7.
16. Takata TS, Wasmund SL, Smith ML et al. Serotonin reuptake inhibitor (Paxil) does not prevent the vasovagal reaction associated with carotid sinus massage and/or lower body negative pressure in healthy volunteers. Circulation 2002;106:1500–04. http://dx.doi.org/10.1161/01.CIR.0000029748.94931.96
17. Kaufmann H, Saadia D, Voustianiouk A. Midodrine in neurally mediated syncope: a double-blind, randomized, crossover study. Ann Neurol 2002;52:342–5. http://dx.doi.org/10.1002/ana.10293
18. Ward CR, Gray JC, Gilroy JJ, Kenny RA. Midodrine: a role in the management of neurocardiogenic syncope. Heart 1998;79:45–9. http://dx.doi.org/10.1136/hrt.79.1.45
19. Qingyou Z, Junbao D, Chaoshu T. The efficacy of midodrine hydrochloride in the treatment of children with vasovagal syncope. J Pediatr 2006;149:777–80. http://dx.doi.org/10.1016/j.jpeds.2006.07.031
20. Perez-Lugones A, Schweikert R, Pavia S et al. Usefulness of midodrine in patients with severely symptomatic neurocardiogenic syncope: a randomized control study. J Cardiovasc Electrophysiol 2001;12:935–8. http://dx.doi.org/10.1046/j.1540-8167.2001.00935.x
21. Romme JJCM, van Dijk N, Go-Schon IK, Reitsma JB, Wieling W. Effectiveness of midodrine treatment in patients with recurrent vasovagal syncope not responding to non-pharmacological treatment (STAND-trial). Europace 2011;13:1639–47. http://dx.doi.org/10.1093/europace/eur200
22. Doyle JF, Grocott-Mason R, Hardman TC, Malik O, Dubrey SW. Midodrine: use and current status in the treatment of hypotension. Br J Cardiol 2012;19:34–7. http://dx.doi.org/10.5837/bjc.2012.007
23. Raj SR, Faris PD, McRae M, Sheldon RS. Rationale for the prevention of syncope trial IV: assessment of midodrine. Clin Auton Res 2012;22:275–80. http://dx.doi.org/10.1007/s10286-012-0167-5
