Identification of ST elevation on the electrocardiogram (ECG) is the cornerstone of diagnosis of ST-elevation myocardial infarction (STEMI). While lesion localisation can usually be achieved by regional ST-elevation patterns on ECG, clinicians often neglect changes in the ST segment of lead aVR, possibly contributing to delayed recognition and poorer outcomes for these patients.
This study compared the ‘door-to-balloon time’ and peak troponins – as a surrogate marker of infarct size – for patients presenting with STEMI with ST-segment elevation in aVR compared with those patients without elevation in aVR. A total of 179 patients, including 17 patients presenting with ST-elevation in aVR, were included in this study. Patients presenting with elevation in aVR had significantly longer door-to-balloon times than those patients presenting with ‘traditional’ patterns of ST-elevation. There was, however, no significant difference in peak troponin as a marker of infarct size. While patients presenting with ST-elevation in lead aVR may have a delayed time to intervention, the present study does not suggest the use of aVR elevation as an indication for urgent angiography.
Introduction
The variety of electrocardiogram (ECG) changes that occur following acute myocardial infarction (AMI), occur in concordance with coronary circulation anatomy. ST-segment elevation in lead aVR can indicate an anterior wall AMI.1,2 However, lead aVR is commonly neglected by clinicians,3 and as such, this may be a potential source of adverse patient outcomes.
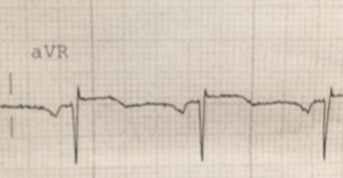
The aim of this single-centre study is to investigate how proficiently AMIs presenting with aVR ST-elevation are recognised, using ‘door-to-balloon times’ as an outcome measure in patients having primary percutaneous coronary intervention (PCI) or those having elective PCI within 24 hours of acute coronary syndrome (ACS), with significant occlusion. The secondary objective was to determine whether poor recognition translates to larger infarction using a surrogate measure of peak troponin levels compared with patients meeting standard ST-elevation myocardial infarction (STEMI) criteria.4 A sample ECG demonstrating elevation in aVR is shown in figure 1.
Materials and methods
This was a retrospective cohort study performed at a single tertiary institution, using The Wollongong Hospital (TWH) catheterisation database. Ethics approval was granted by TWH and the University of Wollongong Human Research Ethics Committee. TWH catheterisation database was searched for non-ST-elevation myocardial infarction (NSTEMI) and STEMI patients over a two-year period ending December 2013. De-identified, coded data included: ECG and basic clinical and demographic data including age, gender, family history of cardiovascular disease, smoking status, hypercholesterolaemia, hypertension and diabetes mellitus. The time from onset of symptoms until presentation at triage, and door-to-balloon times were also recorded. Patients included in this study were those that had a primary PCI, or elective PCI within 24 hours post-ACS, with a significant occlusion. Occlusion was defined as a thrombolysis in myocardial infarction (TIMI) score of 0 or 1.5 Troponin and angiography results were interpreted by the treating cardiology consultant at the time of admission.
All ECGs were independently analysed by a trained investigator (JW) who was blinded to identity and other clinical variables. ST-segment elevation was determined to be present if greater than 0.5 mm, in keeping with current ACS guidelines.6 Confounders that commonly mimic occlusion on ECG, including hyperkalaemia (>5.5 mEq/L), tachycardia (>130 bpm), pulmonary oedema with respiratory failure and diastolic blood pressure (DBP) >120 mmHg were excluded.5 Patients were also excluded if they had a pacemaker, were post-cardiac arrest or presenting with re-infarction within one week due to likely confounding ECG abnormalities or persistence of troponin elevation. Patients transferred from other wards or operating theatres were also excluded as this study aimed to specifically include those patients presenting from the community, not already in monitored medical care, where identification of ECG changes and symptoms at an earlier stage may have expedited transfer for angiography. Statistical analyses were performed using SPSS (version 21.0; SPSS, Inc., Chicago). Independent samples t-tests were used to compare continuous variables. Significance was set at p<0.05.
Results
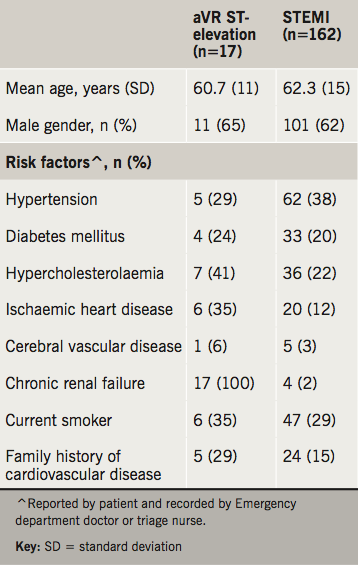
During the data collection period, 1,429 patients underwent coronary angiography at TWH. Of these, 28 met exclusion criteria, 375 had missing data, 807 had either no lesion or TIMI flow ≥2 on elective PCI. Of the remaining 219 patients, 17 met aVR ST-elevation criteria and 162 met STEMI criteria. Patient demographics for aVR ST-elevation and STEMI groups are presented in table 1.
When comparing patients with aVR elevation to patients without elevation in aVR, there was a significant trend towards longer door-to-balloon time (2,759 ± 286 vs. 172 ± 526, p<0.001). There was no statistically significant difference between the initial troponins (147 ± 314 vs. 245 ± 889, p=0.41), or peak 24-hour troponins (1,833 ± 373 vs. 3,526 ± 380, p=0.14) between these groups. In the 17 patients with ST-elevation in aVR, angiography revealed occlusion could be in any of the coronary arteries – including left anterior descending (LAD) (39%), right coronary artery (RCA) (22%), diagonal (6%), circumflex (28%) and the left main coronary artery (LMCA) (6%).
Discussion
This was a single-centre retrospective cohort study with the aim of determining how well ACS presenting with aVR ST-elevation is recognised, using ‘door-to-balloon times’ as an outcome measure. The secondary aim was to determine whether this translates to a larger infarction through a surrogate measure of peak troponin levels.
The mechanism of ST-elevation in aVR in ACS is not fully understood.8 In the present study, a wide variety of coronary arteries were occluded in patients with aVR ST-elevation. This ECG pattern has previously been attributed to LMCA occlusion.1 However, the present study illustrates that the pattern is not confined to an occlusion in this vessel, with only one of the 17 aVR AMI patients presenting with an LMCA occlusion.
This was a single-centre retrospective study, with a small number of aVR AMI patients, limiting the statistical power of this study. Unmeasured confounders, including angiography lab availability, communication, staffing and volume of emergency department presentations, may also influence the ‘door-to-balloon time’ used here as a surrogate measure of recognition of STEMI with aVR ST-elevation. Although delay in door-to-balloon time was not associated with increased infarct size, troponin rise can be confounded by other factors such as renal failure.9 Although the correlation of troponin elevation and infarct size is established, additional measures that were not available in this study, but may be useful in further characterising this end point, include cardiac magnetic resonance imaging (MRI) for illustration of infarct size, as well as long-term outcomes of cardiac function.
In this study there was a significantly longer door-to-balloon time in the aVR ST-elevation group compared with the group of patients with STEMI indicated by elevation in other ECG leads. This did not, however, result in a significantly larger size of infarction, as shown by peak troponin levels. Despite a significant delay in the transfer of patients for angiography, this lack of recognition and/or prioritisation of ST-segment elevation in aVR has no significant impact on infarction size. Therefore, the present study does not support the inclusion of ST-segment elevation in aVR into the criteria for urgent angiography.
Key messages
- Patients presenting with ST-elevation in aVR may be under-recognised as cases of ST-elevation myocardial infarction (STEMI) and, therefore, have longer ‘door-to-balloon’ times than those patients who present with traditional patterns of ST-elevation
- This delayed time to intervention does not correlate with higher peak troponins as a surrogate measure of infarct size, and, therefore, does not suggest that aVR ST-elevation should be used as an indication for urgent angiography
- While aVR elevation has been traditionally associated with left main coronary artery (LMCA) stenosis or occlusion, the present study found that ST-elevation in aVR is relatively non-specific, and could be related to disease in any of the coronary vessels
Conflict of Interest
None declared.
References
1. Aygul N, Ozdemir K, Tokac M et al. Value of lead aVR in predicting acute occlusion of proximal left anterior descending coronary artery and in-hospital outcome in ST-elevation myocardial infarction: an electrocardiographic predictor of poor prognosis. J Electrocardiol 2008;41:335–41. https://doi.org/10.1016/j.jelectrocard.2008.02.025
2. Jong GP, Ma T, Chou P et al. Reciprocal changes in 12-lead electrocardiography can predict left main coronary artery lesion in patients with acute myocardial infarction. Int Heart J 2006;47:13–20. https://doi.org/10.1536/ihj.47.13
3. Kireyev D, Arkhipov MV, Zador ST et al. Clinical utility of aVR – the neglected electrocardiographic lead. Ann Noninvasive Electrocardiol 2010;15:175–80. https://doi.org/10.1111/j.1542-474X.2010.00359.x
4. Hallén J. Troponin for the estimation of infarct size: what have we learned? Cardiology 2012;121:204–12. https://doi.org/10.1159/000337113
5. Smith SW, Khalil A, Henry TD et al. Electrocardiographic differentiation of early repolarization from subtle anterior ST-segment elevation myocardial infarction. Ann Emerg Med 2012;60:45–56. https://doi.org/10.1016/j.annemergmed.2012.02.015
6. Chew DP, Scott IA, Cullen L et al. National Heart Foundation of Australia and Cardiac Society of Australia and New Zealand: Australian clinical guidelines for the management of acute coronary syndromes 2016. Med J Aust 2016;205:128–33. https://doi.org/10.5694/mja16.00368
7. Razali NM, Wah YB. Power comparisons of Shapiro-Wilk, Kolmogorov-Smirnov, Lilliefors and Anderson-Darling tests. Journal of Statistical Modeling and Analytics 2011;2:21–33. Available from: https://www.nrc.gov/docs/ML1714/ML17143A100.pdf
8. de Winter RJ, Verouden NJ, Wellens HJ, Wilde AA. A new ECG sign of proximal LAD occlusion. N Engl J Med 2008;6:2071–3. https://doi.org/10.1056/NEJMc0804737
9. Song D, de Zoysa JR, Ng A, Chiu W. Troponins in acute kidney injury. Ren Fail 2012;34:35–9. https://doi.org/10.3109/0886022X.2011.623440
