Data for low-risk ST-elevation myocardial infarction (STEMI) patients in the Essex cardiothoracic centre (CTC) during a three-month period were evaluated and the average duration of admission was calculated to be 67.2 hours. The data were sifted by applying Second Primary Angioplasty in Myocardial Infarction (PAMI-II) criteria for low-risk STEMI patients who could be safely discharged after 48 hours. After application of a proforma as a quality improvement intervention tool, data were re-assessed and the average time of admission observed for a similar cohort of patients dropped down to an average of 55.2 hours. Overall, there was a 13% average increase in rate of early discharge for low-risk STEMI patients.
Introduction
According to the British Heart Foundation (BHF), in the UK there are more than 100,000 hospital admissions each year due to ST-elevation myocardial infarction (STEMI), equating to 280 admissions each day, or one every five minutes.1 The Essex cardiothoracic centre (CTC) is a tertiary, state-of-the-art centre that is equipped to deal with these high-risk cases. There are five district hospitals covered by the Essex CTC to provide a primary percutaneous coronary intervention (PCI) service. The patient turnover is high and there are emergency and elective procedures undertaken every day. The discharge of patients needs to be timely and organised.
The timing of discharge after inpatient reperfusion therapy post-STEMI is variable. It is dependent upon factors such as medical history, social factors and the extent of myocardial damage. However, low-risk patients can be identified based on the success of the reperfusion therapy and residual functional status of the heart.
Second Primary Angioplasty in Myocardial Infarction (PAMI-II) criteria have been identified in the European Society of Cardiology (ESC) guidelines 2017 to access and identify low-risk groups of patients who can be discharged early.2
Post-STEMI early discharge of low-risk patients has been shown to be safe (PAMI II study).3 There are numerous benefits of early discharges, such as:4
- Less chance of infection
- Increased social support
- Decreased recovery time
- Less stressful
- Economic benefit for hospital
- Increased patient turnover
- Patient satisfaction.
Method
In Essex CTC, an audit was undertaken to assess the discharge duration of patients presenting as STEMIs during a three-month period (September to December 2018). For this purpose, retrospective clinical data were collected from Essex CTC electronically. Low-risk patients were identified using the PAMI-II criteria.
Patients were treated as per standard primary PCI protocol. All patients were loaded with aspirin 300 mg, clopidogrel 600 mg or ticagrelor 180 mg. Unfractionated heparin was administered as per body weight during the procedure. Aspiration catheter and glycoprotein (GP)IIb/IIIa inhibitor, mainly tirofiban, were used where appropriate. Drug-eluting stents were used in all patients where needed. All patients had routine bloods performed on admission. Following successful primary PCI, patients were monitored on the coronary care unit (CCU) for the first 24 hours. Transthoracic echocardiography (TTE) was performed and reported by British Society of Echocardiography (BSE) accredited technicians on all patients. Patients were discharged on dual antiplatelets, statins, beta blockers and angiotensin-converting enzyme (ACE) inhibitors. Cardiac rehabilitation was organised at the local hospital.
Data collection
Out of 196 patients admitted with STEMI, 73 fulfilled the PAMI-II criteria. Only 38 (53%) patients were discharged within 48 hours. There were an extra 17 days of bed occupancy, with an associated cost of £3,893 in 3 months.5
Intervention
After this assessment, a proforma was designed to aid the relevant healthcare professionals in recognising eligible lower-risk patients who could be discharged early. This included the PAMI-II criteria:
- STEMI
- Age <70 years
- 1–2 vessel disease with effective PCI treatment
- Left ventricular ejection fraction (LVEF) >45%
- No persistent arrhythmia.
The proforma for change in discharge protocol was included in the patient notes. Results were assessed monthly for two months. All patients were required to have transthoracic echocardiography (TTE) prior to discharge. This facility was unavailable during the weekends. Patients admitted on Fridays had to stay until Monday to have their TTE performed.
Results
After one month, the data were re-assessed. Of 87 STEMI patients, 34 fulfilled the early discharge criteria. Of these, 26 (76%) were discharged within 48 hours. After the second month, 19 out of 93 STEMI patients fulfilled the criteria, and 11 (58%) were discharged after 48 hours.
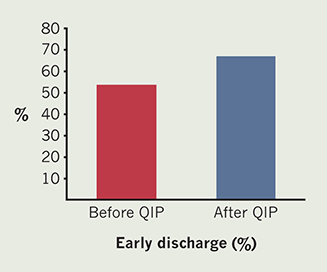
There was a decrease in admission days from 2.8 to 2.3 (67.2 hours to 55.2 hours). It was noticed that there was an increased awareness among doctors and nurses regarding the safety of early discharges. In total, there was a 13% average increase in the rate of early discharges post-quality improvement project (QIP) (figure 1).
The safety of the early discharged patients was assessed by reviewing the 30-day mortality.6,7 The 30-day mortality was zero in this group.
The reasons cited for delayed discharges in the eligible patients included Friday admissions, patients needing medication optimisations prior to discharge, longer clinical observation for left anterior descending (LAD) territory infarction and complications during admission. It was noticed that there was also an increased awareness among doctors and nurses regarding the safety and feasibility of early discharges in low-risk STEMI patents.
Discussion
ESC (2017)2 provided guidelines to assess and identify low-risk groups of patients who can be discharged early. The duration of hospital admission varies greatly depending upon individual factors such as comorbidities, associated risk factors, baseline functionality and social setup. Low-risk patients are identified as those who are less likely to suffer from comorbidities during or after discharge, including those with TIMI (thrombolysis in myocardial infarction) 3 flow on reperfusion,7-9 no significant residual disease in other coronaries needing further intervention, preserved LV systolic function and rhythmic stability. The optimal short stay also implies that patients have the correct cardiac rehabilitation education and optimal titration of medications prior to discharge, including adequate follow-up and safety-net therapy. There have been few studies that support the view that low-risk patients can have safe early discharge post-reperfusion therapy.7 It has been shown by studies that cohorts of early and delayed discharges post-STEMI repercussions have no difference in mortality and rates of readmission.10,11 There was a low risk of complications following an early discharge.12
It could be argued that the short duration of stay in the hospital potentially gives less time for the optimisation of medical therapy. However, a multi-disciplinary approach for the care of these following discharge can address this. Patients are reviewed by the cardiac rehabilitation team in the community upon discharge,13 and then returned for an early review at six weeks in the hospital.
Conclusion
From these data, our study confirms the feasibility of safe and early discharge14 of low-risk STEMI patients using simple criteria with no difference in 30-day mortality.
Key messages
- Timely discharge of acute ST-elevation myocardial infarction (STEMI) patients
- Second Primary Angioplasty in Myocardial Infarction (PAMI-II) criteria applied
- Safety assessed using 30-day mortality
- Safe discharges within 48 hours
Conflicts of interest
None declared.
Funding
None.
Study approval
The QIP Project was registered and approved by the hospital audit department. No patient identifiable data was used.
Editors’ note
Additional data from this paper are available on request.
References
1. British Heart Foundation. Incidence and prevalence. Available at: https://www.bhf.org.uk/what-we-do/our-research/heart-and-circulatory-diseases-in-numbers
2. Ibanez B, James S, Agewall S et al. 2017 ESC guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: the Task Force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology (ESC). Eur Heart J 2017;39:119–77. https://doi.org/10.1093/eurheartj/ehx393
3. Grines CL, Marsalese DL, Brodie B et al. Safety and cost-effectiveness of early discharge after primary angioplasty in low risk patients with acute myocardial infarction. PAMI-II Investigators. Primary Angioplasty in Myocardial Infarction. J Am Coll Cardiol 1998;31:967–72. https://doi.org/10.1016/S0735-1097(98)00031-X
4. Laurencet M-E, Girardin F, Rigamonti F et al. Early discharge in low-risk patients hospitalized for acute coronary syndromes: feasibility, safety and reasons for prolonged length of stay. PLoS ONE 2016;11:e0161493. https://doi.org/10.1371/journal.pone.0161493
5. Data from CTC hospital admissions policy.
6. Spencer FA, Lessard D, Gore JM, Yarzebski J, Goldberg RJ. Declining length of hospital stay for acute myocardial infarction and postdischarge outcomes: a community-wide perspective. Arch Intern Med 2004;164:733–40. https://doi.org/10.1001/archinte.164.7.733
7. Berger AK, Duval S, Jacobs DR Jr. et al. Relation of length of hospital stay in acute myocardial infarction to postdischarge mortality. Am J Cardiol 2008;101:428–34. https://doi.org/10.1016/j.amjcard.2007.09.090
8. Mark DB, Sigmon K, Topol EJ et al. Identification of acute myocardial infarction patients suitable for early hospital discharge after aggressive interventional therapy. Results from the Thrombolysis and Angioplasty in Acute Myocardial Infarction Registry. Circulation 1991;83:1186–93. https://doi.org/10.1161/01.CIR.83.4.1186
9. Luca GD, Suryapranata H, Hof AWJvt et al. Prognostic assessment of patients with acute myocardial infarction treated with primary angioplasty. Circulation 2004;109:2737–43. https://doi.org/10.1161/01.CIR.0000131765.73959.87
10. Gong W, Li A, Ai H, Shi H, Wang X, Nie S. Safety of early discharge after primary angioplasty in low-risk patients with ST-segment elevation myocardial infarction: a meta-analysis of randomised controlled trials. Eur J Prev Cardiol 2018;25:807–15. https://doi.org/10.1177/2047487318763823
11. Jones DA, Rathod KS, Howard JP et al. Safety and feasibility of hospital discharge 2 days following primary percutaneous intervention for ST-segment elevation myocardial infarction. Heart 2012;98:1722–7. https://doi.org/10.1136/heartjnl-2012-302414
12. Sharkawi MA, Filippaios A, Dani SS et al. Identifying patients for safe early hospital discharge following ST elevation myocardial infarction. Cathet Cardiovasc Intervent 2017;89:1141–6. https://doi.org/10.1002/ccd.26873
13. Piepoli MF, Corrà U, Adamopoulos S et al. Secondary prevention in the clinical management of patients with cardiovascular diseases. Core components, standards and outcome measures for referral and delivery: a Policy Statement from the Cardiac Rehabilitation Section of the European Association for Cardiovascular Prevention & Rehabilitation. Endorsed by the Committee for Practice Guidelines of the European Society of Cardiology. Eur J Prev Cardiol 2014;21:664–81. https://doi.org/10.1177/2047487312449597
14. Roberts L, Parfrey S, Andrianopoulos N et al. TCT-187 safety of early discharge following percutaneous coronary intervention (PCI) for STEMI. J Am Coll Cardiol 2016;68(18 suppl):B76–B77. https://doi.org/10.1016/j.jacc.2016.09.329
