The assessment of the prognostic value of the admission electrocardiography (ECG) (specifically of the duration of the PR and QTc intervals, the QRS complex and the heart rate [HR]) in COVID-19 patients on the basis of nine observational studies (n=1,424) indicates that relatively long duration of the QTc interval and QRS complex, as well as higher HR, are linked to a severe course of COVID-19, which may be of use in risk stratification. Since there are important differences in suggested indicators of adverse prognosis between observational studies, further research is necessary to clarify high-risk criteria.
Introduction
The COVID-19 pandemic has posed a serious threat to global health worldwide. In an acute disease process, which is the case in COVID-19, electrocardiography (ECG) abnormalities are common, present in up to 93% of hospitalised critically ill patients.1 Any specific ECG alteration criteria could help emergency clinicians establish the prognosis and assess the risk of adverse events resulting from coronavirus infection.
The purpose of this meta-analysis was to assess the prognostic value of the admission ECG (specifically: the duration of the PR interval, the QTc interval and the QRS complex and the heart rate [HR]) in COVID-19 patients.
Materials and method
A literature selection was performed in the PubMed database for articles up to 9 April 2021, using the keywords “(EKG or electrocardiography or ECG) and (COVID or COVID-19 or coronavirus)”. The eligibility criteria included prospective or retrospective observational cohort studies in which patients were diagnosed with COVID-19 confirmed with RT-PCR (reverse transcriptase polymerase chain reaction) test. The patients should have also undergone ECG on admission and their clinical outcomes should have been evaluated. The ECG results presented in the study should have contained the mean or median duration of the PR interval, of the QTc interval and of the QRS complex, as well as the mean HR, with their standard deviations or interquartile ranges.
We have divided the included patients into two groups: Group I – with favourable clinical outcome – no major adverse events during hospitalisation; Group II – with adverse clinical outcome – major adverse events, transfer to intensive care unit (ICU), death. Then the mean values of studied parameters with their standard deviations were calculated for both groups and compared using Student’s t-test. QTc intervals in almost all included studies were calculated based on Bazett formula. Those specific ECG parameters were selected based on data availability. Online Mean Variance Estimator – HKBU MATH2,3 was used to estimate the sample mean and standard deviation if the included study contained medians with interquartile ranges. Data were analysed in MS Excel 2016 and the significance of the tested differences was assumed on the p<0.05 level. Ethical approval was not required for our study.
Results
Our approach led to identification of a total of 502 potentially relevant studies out of which nine observational studies were eventually included.1,4-11 This brought the total number of examined patients to 1,424. The studies were published between June 2020 and February 2021, and 63 to 431 patients were included in each study, however, in four cases, only a part of the study group was suitable for this meta-analysis. Three studies were conducted in Italy, one in Germany, two in the United States, one in Iraq, one in China and one in Turkey.
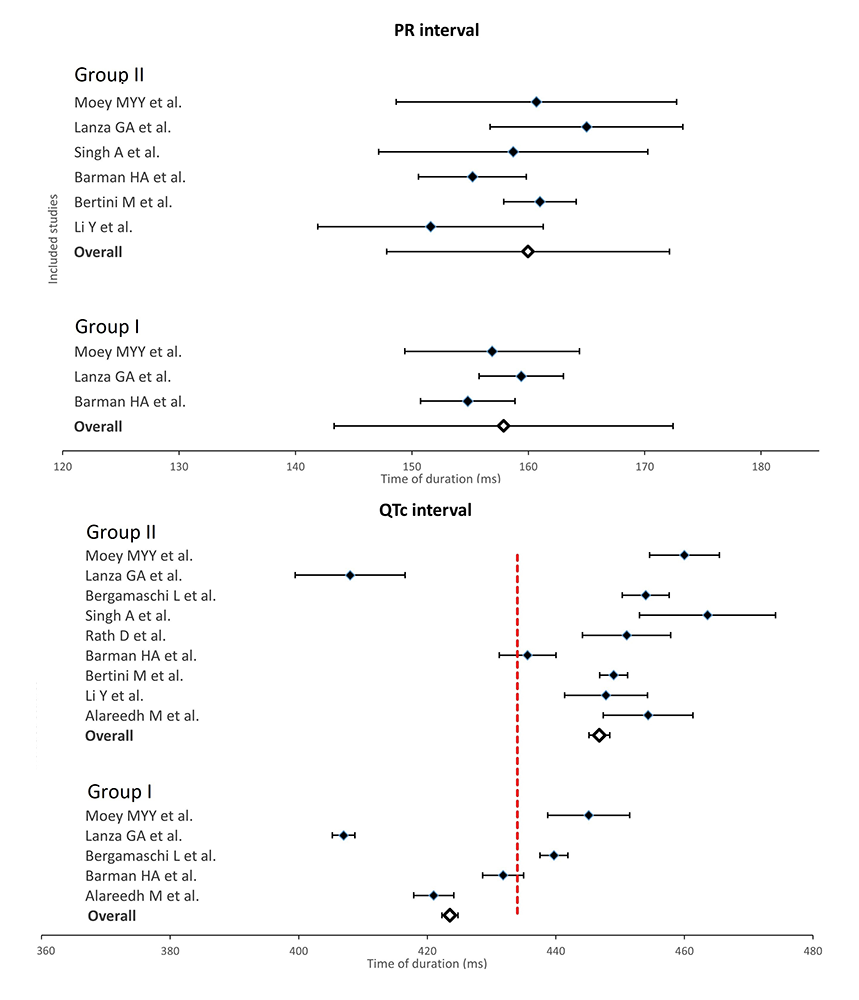
Among the enrolled patients, 665 were assigned to Group I and Group II consisted of 759 patients. After calculation of means with standard deviations for Groups I and II, we found differences in every assessed parameter (table 1), but only QRS complex (p<0.001), QTc interval (p<0.000001) and HR (p<0.0001) were proven to be significantly different. Mean values for each parameter in included studies and in both analysed groups are displayed in figures 1A and 1B.
Table 1. Comparison of electrocardiogram (ECG) parameters between Groups I and II: descriptive statistics
| ECG parameter | Group I (favourable outcome) |
Group II (adverse outcome) |
Total | |||
|---|---|---|---|---|---|---|
| n | mean ± SD | n | mean ± SD | n | mean ± SD | |
| PR interval, ms | 452 | 157.87 ± 28.57 | 667 | 159.98 ± 31.69 | 1,119 | 159.13 ± 30.47 |
| QRS complex, ms | 665 | 94.88 ± 16.20 | 751 | 98.43 ± 22.44 | 1,416 | 96.76 ± 19.83 |
| QTc interval, ms | 665 | 423.52 ± 32.25 | 759 | 446.76 ± 45.99 | 1,424 | 435.91 ± 41.79 |
| Heart rate, bpm | 566 | 82.11 ± 16.41 | 700 | 88.29 ± 23.56 | 1,266 | 85.52 ± 20.89 |
| Key: bpm = beats per minute; ECG = electrocardiogram; SD = standard deviation | ||||||

Discussion
In our study, the patients with worse clinical outcomes proved to have longer mean values of all studied admission ECG parameters than those whose clinical outcome was defined as favourable (table 1). However, statistical analysis revealed significant differences only in the duration of QRS complex, QTc interval and in the HR.
Our findings suggest that assessment of the duration of QRS complex, QTc interval and the HR performed on admission could be potentially beneficial in clinical management of patients with confirmed COVID-19. Clearly identified ECG predictors of adverse prognosis can be of help in pre-empting the appearance of more serious manifestations of the disease.
From this meta-analysis, we hypothesise that a potential high-risk profile for major adverse events, transfer to ICU or death may consist of:
- QRS complex ≥97 ms
- QTc interval >435 ms
- HR >85 bpm.
All those criteria are presented as red dashed lines in the charts (figure 1). Undoubtedly, this estimation should be verified in further studies, since all the included original research were observational studies.
In fact, similar ECG changes have been already proven to foreshadow increased risk of adverse events in myocarditis, where prolonged QRS duration was an independent predictor for cardiac death or heart transplantation, and QTc prolongation was associated with poor outcome as well.12 The possibility of such an application in COVID-19 patients is at least worth investigation.
We have to acknowledge the limitations of our study. First of all, the analysis is vulnerable to any deviation from a normal distribution in included study groups. Moreover, in our approach we did not take into account the course of COVID-19, such as the onset time of the patients’ COVID-19 symptoms. Furthermore, some patients in the selected studies were treated with hydroxychloroquine and/or azithromycin or lopinavir/ritonavir. The influence of those drug therapies could be relevant.
In summary, we found that ECG is of potential use in the triage of COVID-19 patients as patients with poor clinical outcome present significantly longer QRS complex, QTc interval and greater HR than patients with favourable prognosis. Since there are important differences in suggested indicators of adverse prognosis between observational studies, further research is necessary to clarify high-risk criteria.
Key messages
- There is some evidence for the existence of statistically significant differences in the duration of QRS complex, QTc interval and in the heart rate (HR) between COVID-19 patients with favourable and unfavourable clinical outcome
- Assessment of the duration of QRS complex, QTc interval and the HR performed on admission could be of help in pre-empting the appearance of more serious manifestations of COVID-19
- A potential high-risk profile for major adverse events, transfer to intensive care unit (ICU) or death in COVID-19 may consist of: QRS complex ≥97 ms; QTc interval >435 ms; HR >85 bpm
Conflicts of interest
None declared.
Funding
None.
References
1. Bertini M, Ferrari R, Guardigli G et al. Electrocardiographic features of 431 consecutive, critically ill COVID-19 patients: an insight into the mechanisms of cardiac involvement. Europace 2020;22:1848–54. https://doi.org/10.1093/europace/euaa258
2. Luo D, Wan X, Liu J, Tong T. Optimally estimating the sample mean from the sample size, median, mid-range, and/or mid-quartile range. Stat Methods Med Res 2018;27:1785–805. https://doi.org/10.1177/0962280216669183
3. Wan X, Wang W, Liu J, Tong T. Estimating the sample mean and standard deviation from the sample size, median, range and/or interquartile range. BMC Med Res Methodol 2014;14:135. https://doi.org/10.1186/1471-2288-14-135
4. Moey MYY, Sengodan PM, Shah N et al. Electrocardiographic changes and arrhythmias in hospitalized patients with COVID-19. Circ Arrhythm Electrophysiol 2020;13:e009023. https://doi.org/10.1161/CIRCEP.120.009023
5. Lanza GA, De Vita A, Ravenna SE et al. Electrocardiographic findings at presentation and clinical outcome in patients with SARS-CoV-2 infection. Europace 2021;23:123–9. https://doi.org/10.1093/europace/euaa245
6. Bergamaschi L, D’Angelo EC, Paolisso P et al. The value of ECG changes in risk stratification of COVID-19 patients. Ann Noninvasive Electrocardiol 2021;26:e12815. https://doi.org/10.1111/anec.12815
7. Singh A, Akbar MS, McElroy D et al. The electrocardiographic manifestations and derangements of 2019 novel coronavirus disease (COVID-19). Indian Pacing Electrophysiol J 2021;21:156–61. https://doi.org/10.1016/j.ipej.2021.02.005
8. Rath D, Petersen-Uribe A, Avdiu A et al. Impaired cardiac function is associated with mortality in patients with acute COVID-19 infection. Clin Res Cardiol 2020;109:1491–9. https://doi.org/10.1007/s00392-020-01683-0
9. Barman HA, Atici A, Alici G et al. The effect of the severity COVID-19 infection on electrocardiography. Am J Emerg Med 2020;46:317–22. https://doi.org/10.1016/j.ajem.2020.10.005
10. Li Y, Liu T, Tse G et al. Electrocardiographic characteristics in patients with coronavirus infection: a single-center observational study. Ann Noninvasive Electrocardiol 2020;25:e12805. https://doi.org/10.1111/anec.12805
11. Alareedh M, Nafakhi H, Shaghee F, Nafakhi A. Electrocardiographic markers of increased risk of sudden cardiac death in patients with COVID-19 pneumonia. Ann Noninvasive Electrocardiol 2021;26:e12824. https://doi.org/10.1111/anec.12824
12. Ukena C, Mahfoud F, Kindermann I, Kandolf R, Kindermann M, Bohm M. Prognostic electrocardiographic parameters in patients with suspected myocarditis. Eur J Heart Fail 2011;13:398–405. https://doi.org/10.1093/eurjhf/hfq229
