It is well recognised that phase 3 cardiac rehabilitation is beneficial, reducing both mortality and morbidity following acute myocardial infarction. The role of ongoing phase 4 cardiac rehabilitation is less clear. This study was designed to assess the effectiveness of phase 4 cardiac rehabilitation in acute myocardial infarction.
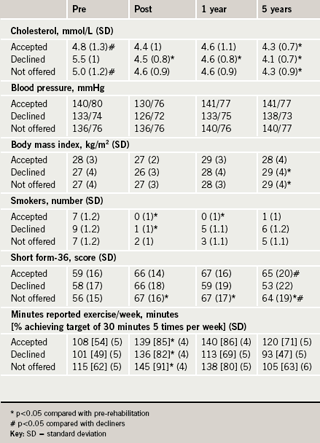
Following acute myocardial infarction, 143 patients who had completed phase 3 cardiac rehabilitation were followed up. Analysis was divided into three groups: those who took up phase 4 rehabilitation, those offered who declined and those not offered phase 4 rehabilitation because it was not available locally. Risk factor profile, self-reported exercise and quality-of-life scores using the short form (SF)-36 were assessed in all patients.
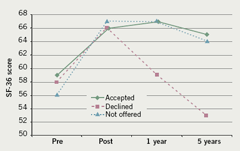
Body mass index (BMI) shows no overall change in the ‘accepted’ group, but shows a significant increase between pre and five-year levels in the ‘declined’ group (p=0.024) and in the ‘not offered’ group (p=0.014). All groups showed an increase of SF-36 scores following phase 3, which showed a trend towards significance. Both the ‘accepted’ and ‘not offered’ groups maintained this improvement, while the ‘declined’ group returned to baseline (p=0.05 vs. ‘accepted’ and p=0.03 vs. ‘not offered’). All groups had similar exercise levels initially and all showed significant improvements after phase 3 with some deterioration out to five years. This decline in exercise was significant in the ‘declined’ group (p=0.029) and shows a trend in the ‘not offered’ group (p=0.057).
This small single-centre study suggests that there are observable benefits in participating in long-term phase 4 cardiac rehabilitation. Those who decline phase 4 cardiac rehabilitation clearly do less well. Whether the benefits seen can be attributed directly to phase 4 cardiac rehabilitation would require a different study design to address this issue.
Introduction
It is now accepted that phase 3 cardiac rehabilitation post acute myocardial infarction (AMI) is beneficial in reducing long-term mortality and morbidity.1-3 It also increases exercise capacity,4-6 improves risk factor profile1,2,7 and improves quality of life.6,8-11 These benefits occur across all age groups12-14 and in both sexes15,16 – women and the elderly have been and continue to be, under-referred for cardiac rehabilitation (CR).17,18 They are also cost-effective.19,20
The ideal duration, location and composition of such CR programmes is less clear. Hospital-based programmes clearly appear to be effective.1 Using the heart manual and/or delivering CR in the community setting appears to produce equivalent results to a hospital programme.21-24
Many centres offer ‘traditional’ hospital-based phase 3 CR with ongoing phase 4 CR in the community afterwards. The benefits of this supplemental, long-term, community-based style of CR over and above what is offered in phase 3 is unknown, and we therefore conducted this trial in order to assess this potential benefit.
Phase 4 CR was initially started in the northern extreme of our district and was only available to a small number of patients. Our study looked at all patients with AMI who completed the phase 3 hospital-based programme over its first year. We assessed their progress one year and five years later and analysed according to whether they took up phase 4 CR, declined to attend or were not offered it because they lived too far away from its base (in excess of one hour travel by car).
Many patients who initially did not have local phase 4 facilities gained these during the five years of follow-up and we know some enrolled in the programme later. This study is analysed under intention to treat.
Methods
In phase 1 all patients admitted to hospital with a diagnosis of AMI were referred to the CR nurse within one working day of diagnosis and seen prior to discharge. Those who smoked were offered in-patient smoking cessation, including nicotine replacement therapy. All patients were commenced, if possible, on aspirin, atenolol, simvastatin and ramipril. All patients with a diagnosis of non-ST elevation myocardial infarction (NSTEMI) who were appropriate for revascularisation were referred for in-patient coronary angiography. All patients were commenced on the heart manual and given a date for their exercise tolerance test prior to discharge.
In phase 2 all patients were discharged with the heart manual and seen within four days of discharge by a trained heart manual facilitator. They received an exercise electrocardiogram (ECG) at two weeks to identify high-risk patients requiring urgent investigation, and to allow exercise prescription. The consultant cardiologist reported the tests and the results, along with details of the patient’s adjustable risk factors for coronary artery disease, to the patient’s general practitioner with suggestions for ongoing care and optimisation of therapy.
All patients were offered hospital-based phase 3 CR, which runs from week six to week 12 following AMI. Prior to starting, and at completion of phase 3, CR risk factor analysis, lifestyle and quality of life using the short form (SF)-36 were assessed. At completion, all patients were referred for a repeat exercise ECG, off beta blockers, to assess their progress and long-term prognosis. The consultant cardiologist reported these and sent the results, along with repeat risk factor analysis, to the patient’s general practitioner.
All patients who lived in the catchment area for the phase 4 programme were offered referral into that programme, and analysis was subdivided into those who chose to take up phase 4 CR and those who declined to attend. Patients living elsewhere were not formally offered phase 4 CR, but were encouraged to join local sports clubs and maintain their exercise by other routes. Thus, randomisation was not blinded in any way, but rather was driven by availability and patient choice into the three groups – accepted, declined and not offered. All patients were invited back at one year and five years after AMI to assess their risk factor profile, lifestyle and quality of life.
The phase 4 programme offered to patients was a multi-disciplinary programme including walking for health, a cycling project, a Young Men’s Christian Association (YMCA) programme, swimming, healthy hearts club, bowling, dancing, yoga, tai chi, food co-operatives, eating for a healthy heart, dietetic advice, ongoing smoking cessation and relaxation techniques. After three years, the initial Health Action Zone funding ran out and much of the activity was cut back. New premises were found and the programme running at the end of the project was much more gym and exercise orientated, run by two British Association for Cardiac Rehabilitation (BACR) accredited phase 4 instructors. Over the five years, similar gym-based programmes were rolled out throughout the region with BACR phase 4 accredited instructors, such that by the end of the project less than 10% of the population not originally offered CR still had no ready access.
Results
We performed a Shapiro-Wilk test on the original data and the log of the data within each of the patient groups to test the data for normality. Data analysis was based on quantifying p-values, with data considered to be normally distributed for p-values greater than 0.05. Overall, the whole of the original dataset was normally distributed.
The ANOVA single-factor test was performed both on the pre, post, one-year and five-year data for each parameter to assess for variations in time within groups, and again to assess for variations between groups.
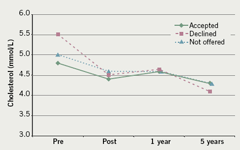
Overall data are shown in table 1, the different parameters in figures 1–6.
Cholesterol
Those who declined phase 4 had a higher cholesterol pre CR (p=0.029) than either those accepting, or those not offered CR. For those accepting CR improvement post CR approaches significance (p=0.092). This improvement was maintained to year five and reached significance (p=0.04). For those declining CR there was a highly significant reduction post CR (p<0.001), maintained to year five with further significant reduction from post to year five (p=0.027). For the no provision group there was a non-significant reduction from pre to post CR (p=0.17), which was maintained to year five with some further reduction, achieving significance relative to pre (p=0.029). Based on the year five data for all groups there was no difference between treatment groups at year five (for ANOVA on all three groups p=0.59; t-test for difference between accept and decline p=0.27).
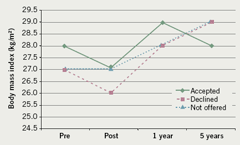
Body mass index (BMI)
There was no initial difference between the groups. For those who accepted CR there was no significant change in BMI over all time periods. For the group declining CR there was a non-significant reduction between pre and post CR (p=0.42). However, there was a significant increase in BMI between pre CR and year five (p=0.024). For the no provision group there was also a non-significant reduction between pre and post CR (p=0.87). However, there was a significant increase in BMI between pre CR and year five (p=0.014). Based on the year five data for all groups there was no difference in BMI at year five for the three groups.
Blood pressure
There was no initial difference between the groups. For those who accepted CR there was a non-significant reduction post CR, followed by a non-significant increase to year five. For the group declining CR there was a non-significant decrease between pre and post CR. This was followed by a significant increase (p=0.031) to year five. Overall, there was a non-significant increase between pre CR to year five data (p=0.38). For the no provision group any increase/decrease in blood pressure was insignificant, and there was no evidence of a change in blood pressure with time. Based on the year five data for all groups there was no evidence of any difference between treatment groups at year five.
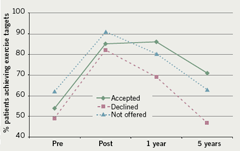
SF-36
There was no initial difference between the groups. For those who accepted CR there was a marginally significant improvement between pre and post CR (p=0.069). However, this was followed by no further significant improvement. The overall improvement from pre CR to year five was not significant (p=0.169). For the group declining CR, there was a non-significant improvement between pre and post CR (p=0.238), which was then followed by a decline to year five that approaches significance (p=0.088). For the no provision group there was a significant improvement between pre and post CR (p=0.019), which was subsequently maintained to year five (p=0.049). Based on the year five data for all groups, the group declining CR show a lower SF-36 score at year five (p=0.053, one-way ANOVA on three groups; p=0.057, Welch two sample t-test: accepters vs. decliners; p=0.030, Welch two sample t-test: no provision vs. decliners).
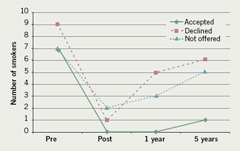
Smoking
There was no initial difference between the groups. All groups showed a reduction in the proportion of smokers post CR. This was significant for both accepters and decliners (p=0.017 and p=0.028, respectively) but not significant for the non-provision group (p=0.17). Analysis of the results between pre CR and five years shows that improvement at five years falls away for all groups. This was less so for the accepters group. For no group was the improvement at five years significant, although for accepters the improvement approaches significance (two-sided p=0.122, one-sided p=0.061). Analysis of the results between post CR and five years shows the proportion of smokers increases markedly for decliners but not for the other groups; however, the increase does not reach significance (two-sided p=0.161, one-sided p=0.08).
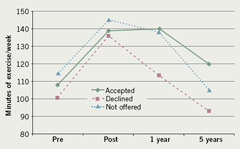
Exercise
There was no initial difference between the groups. All groups show significant improvement in exercise post CR (p=0.0036 accepters, p=0.0136 decliners and p=0.021 non-provision). Analysis of the results between pre CR and five years shows that all groups show some deterioration through to year five. For the group declining CR this was significant (p=0.029) and for the no provision group this approaches significance (p=0.057). The group declining CR exercise less at year five than the other groups, but this difference was not significant (p=0.14).
Discussion
All groups achieved good and similar benefits across all measures following phase 3 CR. This indicates that the phase 3 programme delivered locally is capable of delivering the expected improvements2,4,6 and is compliant with national guidelines and standards.25,26
The maintained benefits in cholesterol reduction and blood pressure control across all groups may be due to the new General Medical Services (GMS) contract in general practice as these are measures specifically taken to assess performance in patients with coronary heart disease. This supposition cannot be confirmed, but would explain why cholesterol levels, in particular, continued to improve between years one and five during which time frame the GMS contract was introduced.
During the five-year follow-up, phase 4 was rolled out to cover the whole locality and many people in the ‘not offered’ group took advantage of this (exact figures are not available). This makes analysis of this group difficult, but would suggest that their results should fall between the ‘accepted’ and ‘declined’ groups due to ideological ‘accepters’ and ‘decliners’ making up this group. Ideally, this group would have acted as a control against the ‘accepted’ group to show the benefits of phase 4 CR, but with the roll out of phase 4 CR this becomes impossible.
The ‘declined’ group appears to do less well than the other two groups in the areas of quality of life (as measured with the SF-36) and lifestyle measures (as assessed by smoking, BMI and exercise taken). What is not clear is if this is due to a true benefit from phase 4 CR, or whether it is because these people have a lower commitment to their personal health than those who go to phase 4 CR.
In conclusion, the data suggest that there are benefits attributable to phase 4 CR; collection of a larger dataset is necessary to resolve which factors are responsible for the benefits seen, along with a different study design specifically addressing this issue.
Acknowledgements
The authors would like to thank Dr J Vives I Batlle and Professor S Jones from the Westlakes Research Institute, Westlakes Science and Technology Park, for their assistance in the statistical analysis.
Conflict of interest
None declared.
Key messages
- Real-life phase 3 cardiac rehabilitation is effective
- Those who decline phase 4 cardiac rehabilitation have a worse long-term health status
References
- Jolliffe JA, Rees K, Taylor RS, Thompson D, Oldridge N, Ebrahim S. Exercise-based rehabilitation for coronary heart disease. Cochrane Database Syst Rev 2001;(1):CD001800. DOI:10.1002/14651858.CD001800
- Vermuelen A, Lie KI, Durrer D. Effects of cardiac rehabilitation after myocardial infarction: changes in coronary risk factors and long-term prognosis. Am Heart J 1983;105:798–801.
- Kallio V, Hamalainen H, Hakkila J, Luurila OJ. Reduction in sudden deaths by a multifactorial intervention programme after acute myocardial infarction. Lancet 1979;2:1091–4.
- Carson P, Phillips R, Lloyd M et al. Exercise after myocardial infarction: a controlled trial. J R Coll Physicians Lond 1982;16(3):147–51.
- Engblom E, Hietanen EK, Hamalainen H, Kallio V, Inberg M, Knuts LR. Exercise habits and physical performance during comprehensive rehabilitation after coronary artery bypass surgery. Eur Heart J 1992;13:1053–9.
- Carlsson R. Serum cholesterol, lifestyle, working capacity and quality of life in patients with coronary artery disease. Experiences from a hospital-based secondary prevention programme. Scand Cardiovasc J 1998;50(Suppl):1–20.
- Ballantyne FC, Clark RS, Simpson HS, Ballantyne D. The effect of moderate physical exercise on the plasma lipoprotein subfractions of male survivors of myocardial infarction. Circulation1982;65:913–18.
- Engblom E, Hamalainen H, Lind J et al. Quality of life during rehabilitation after coronary bypass surgery. Qual Life Res 1992;1:167–75.
- Engblom E, Korpilahti K, Hamalainen H, Ronnemaa T, Puukka P. Quality of life and return to work 5 years after coronary artery bypass surgery. J Cardiopulm Rehabil 1997;17:29–36.
- Taylor CB, Houston-Miller N, Ahn DK, Haskell W, DeBusk RF. The effects of exercise training programs on psychosocial improvement in uncomplicated postmyocardial infarction patients. J Psychosom Res 1986;30:581–7.
- Oldridge N, Guyatt G, Jones N et al. Effects on quality of life with comprehensive rehabilitation after acute myocardial infarction. Am J Cardiol 1991;67:1084–9.
- Ebrahim S, Davey Smith G. Health promotion in older people for cardiovascular disease prevention – a systematic review and meta-analysis. London: Health Education Authority, 1996.
- Willmer K, Simpson T, Hackett K et al. Effects of exercise rehabilitation in the elderly. Coronary Health Care 1999;3:117–20.
- Ades PA, Waldmann ML, Gillespie C. A controlled trial of exercise training in older coronary patients. J Gerontol A Biol Sci Med Sci 1995;50A:M7–M11.
- Balady GL, Jette D, Scheer J, Downing J. Changes in exercise capacity following cardiac rehabilitation in patients stratified according to age and gender. J Cardiopulm Rehabil 1996;16:38–46.
- Carhart RL, Ades PA. Gender differences in cardiac rehabilitation. Cardiology Clinics 1998;16:37–43.
- Ades PA, Waldmann Ml, Polk DM, Coflesky JT. Referral patterns and exercise response in the rehabilitation of female coronary patients aged greater than or equal to 62 years. Am J Cardiol1992;69:1422–5.
- Thomas RJ, Miller NH, Lamendola C et al. National survey on gender differences in cardiac rehabilitation programs. J Cardiopulm Rehabil 1996;16:402–12.
- Ades PA, Pashkow FJ, Nestor JR. Cost-effectiveness of cardiac rehabilitation after myocardial infarction. J Cardiopulm Rehabil 1997;17:222–31.
- Taylor R, Kirby B. The evidence base for the cost effectiveness of cardiac rehabilitation. Heart 1997;78:5–6.
- Bethell HJN, Mullee MA. A controlled trial of community based coronary rehabilitation. Br Heart J 1990;64:370–5.
- DeBusk RF, Haskell WL, Miller NH et al. Medically directed at-home rehabilitation soon after clinically uncomplicated acute myocardial infarction: a new model for patient care. Am J Cardiol1985;55:251–7.
- Miller NH, Haskell WL, Berra K, DeBusk RF. Home versus group exercise training for increasing functional capacity after myocardial infarction. Circulation 1984;70:645–9.
- Taylor CB, Miller NH, Smith PM, DeBusk RF. The effect of a home-based, case-managed, multifactorial risk-reduction program on reducing psychological distress in patients with cardiovascular disease. J Cardiopulm Rehabil 1997;17:157–62.
- Scottish Intercollegiate Guidelines Network (SIGN). Cardiac rehabilitation: A national clinical guideline. No. 57. Edinburgh: SIGN, 2002.
- British Association for Cardiac Rehabilitation. Standards and core components for cardiac rehabilitation. British Association for Cardiac Rehabilitation (BACR), 2007.
