Elevated cholesterol/lipid levels, especially low-density lipoprotein cholesterol (LDL-C) are known to contribute to the development of atherosclerotic cardiovascular disease (ASCVD). The attainment of lipid targets is known to be suboptimal both globally and locally. This study aimed to evaluate the effectiveness of a lipid management pathway (LMP) in supporting attainment of lipid targets following an acute coronary syndrome (ACS) in a local cohort of cardiac rehabilitation (CR) patients.
Quantitative data were retrospectively collected from 54 CR patient records. Local lipid target attainment was benchmarked against national guidelines and pre-pathway implementation audit results.
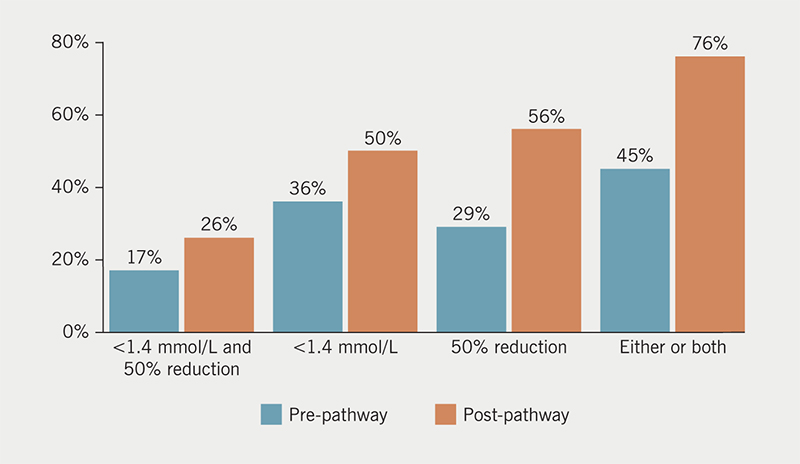
The number of admission lipid profiles increased by 24.8% to 79.6% following implementation of the LMP. There was a 31% improvement in the number of patients achieving either a 50% reduction in LDL-C or an LDL-C level of <1.4 mmol/L. In conclusion, the LMP had a significant positive impact upon the attainment of lipid goals.
Introduction

Research suggests that globally, attainment of lipid targets is poor, with significant scope for improved optimisation of lipid lowering therapy (LLT) and cardiovascular (CV) risk factor management. Evidence suggests that the key initiating event in atherogenesis is retention of low-density lipoprotein cholesterol (LDL-C). To align with this, the European Society of Cardiology and European Atherosclerosis Society (ESC/EAS) proposed new LDL-C goals in 2019,1 and revised CV risk stratification guidance (particularly relevant to high-risk and very high-risk patients).
National Institute for Health and Care Excellence (NICE) guidance for lipid management in CV disease recommends a lipid target of >40% reduction in non-high-density lipoprotein (HDL).2 However, preliminary local audit data revealed levels of LDL-C often remaining above the more recent ESC/EAS recommended level of 1.4 mmol/L, despite a >40% reduction in non-HDL. The primary focus of this study was, therefore, LDL-C levels.
Research has found that reducing LDL-C by 1 mmol/L can lead to a 22–26% reduction of major adverse CV events, and suggested there is no lower limit for these benefits.3 Despite this, low rates of LDL-C goal attainment are noted.4,5 EUROASPIRE (European Action on Secondary and Primary Prevention by Intervention to Reduce Events) IV,5 a multi-national, cross-sectional study to determine whether CV ESC/EAS prevention guidelines were being followed in everyday clinical practice, found that only 19.5% of coronary patients had LDL-C levels below 1.8 mmol/L. This evidence indicates that the ESC/EAS recommendation for LDL-C of <1.4 mmol/L is not being widely met and lower goals may be even more difficult to attain.6
A lipid management pathway (LMP) was created with the purpose of facilitating the attainment of individual lipid targets. It was designed to act as a prompting tool for clinicians, and a guide to ensure patients are monitored adequately and optimised on the most appropriate LLT for CV risk reduction. This audit aimed to evaluate the effectiveness of this pathway in improving attainment of lipid targets.
Materials and method
A retrospective, post-pathway clinical audit assessed the effectiveness of the LMP in improving the attainment of lipid level targets, focused on LDL-C targets in high-risk and very high-risk patients1 in the secondary prevention of CV disease.
The audit included all patients referred to cardiac rehabilitation (CR) following ST-elevation myocardial infarction (STEMI) or non-ST-elevation myocardial infarction (NSTEMI) between 1 June 2020 and 1 December 2020. Standard data included hospital admission lipid profile, follow-up lipid profile during CR, and LDL-C level on admission and on discharge from CR. Lipid levels attained during CR were benchmarked against the ESC/EAS targets for high and very high-risk patients,1 and compared with results from a pre-pathway audit.
Sampling
An unbiased selection of patients was obtained by purposive sampling of all patients who attended CR and were discharged within the specified time frame. Fifty-four patients met the inclusion criteria.
Results
Demographics

Patients’ ages ranged between 48 and 94 years with a mean of 69.4 years, compared with a mean age of 67 years in the participating programmes in the recent National Audit of Cardiac Rehabilitation (NACR) Quality and Outcomes Report,7 so the sample was representative of the wider CR population in the UK.
In the post-pathway sample 37% were female (63% male) compared with 38% female (62% male) in the pre-pathway sample.
Initiating event
There was a higher rate of NSTEMI (59%) initiating events compared with STEMI (37%), consistent across genders.
Admission lipids
In the pre-pathway audit 54.8% of patients had a recorded lipid profile on admission to hospital in North Wales. In the post-pathway audit documented lipids increased to 79.6%.
Baseline and discharge lipid levels
Table 1 compares the baseline and discharge LDL-C and non-HDL levels between the pre- and post-pathway cohorts.
Table 1. Baseline and discharge low-density lipoprotein cholesterol (LDL-C) and non-high-density lipoprotein (HDL)
| Baseline | Discharge | |||
|---|---|---|---|---|
| Pre-pathway (mmol/L) |
Post-pathway (mmol/L) |
Pre-pathway (mmol/L) |
Post-pathway (mmol/L) |
|
| Minimum LDL-C | 0.9 | 1.0 | 0.7 | 0.2 |
| Maximum LDL-C | 5.6 | 7.4 | 4.3 | 5.3 |
| Mean LDL-C | 3.1 | 3.52 | 2.0 | 1.6 |
| Minimum non-HDL | 1.5 | 1.4 | 1.4 | 1.2 |
| Maximum non-HDL | 9.5 | 8.7 | 9.5 | 6.4 |
| Mean non-HDL | 4.1 | 4.5 | 2.7 | 2.3 |
LDL-C reduction
The pre-pathway audit revealed suboptimal lipid management, consistent with findings from studies across the UK and Europe. Figure 1 demonstrates the improvement in ESC/EAS1 target attainment in the six months following the introduction of the LMP. The total number of patients achieving both a LDL-C reduction of 50% and a level of below 1.4 mmol/L increased from 17% to 26%. The number achieving the target LDL-C increased from 36% to 50%, while 56% achieved a >50% reduction in LDL-C compared with 29% pre-pathway. Most notably, 76% of patients were achieving either or both of those targets in the post-pathway audit, compared with only 45% pre-pathway.
Results from the pre-pathway audit showed that females were less likely to achieve their lipid targets, with only 37.5% of females compared with 61.5% of males to target by the end of their CR. This again was consistent with findings from other larger studies. Interestingly, females were more likely to achieve a >50% reduction in LDL-C levels than males in the post-pathway audit cohort, while males were more likely to have an LDL-C level of <1.4 mmol/L. When looking at the combined target of a >50% reduction in LDL-C and LDL-C level of <1.4 mmol/L, males were more than twice as likely to attain the target than females with 32% and 15%, respectively.
Those patients classified as having had a STEMI were slightly more likely (55%) to achieve the LDL-C target of <1.4 mmol/L compared with NSTEMI (47%).
A significant 70% of STEMI patients had a more than 50% reduction in LDL-C compared with 47% of NSTEMI patients, while the combined target achievement difference between the groups is more modest with only a 5% difference (30% of STEMI patients and 25% of NSTEMI patients).
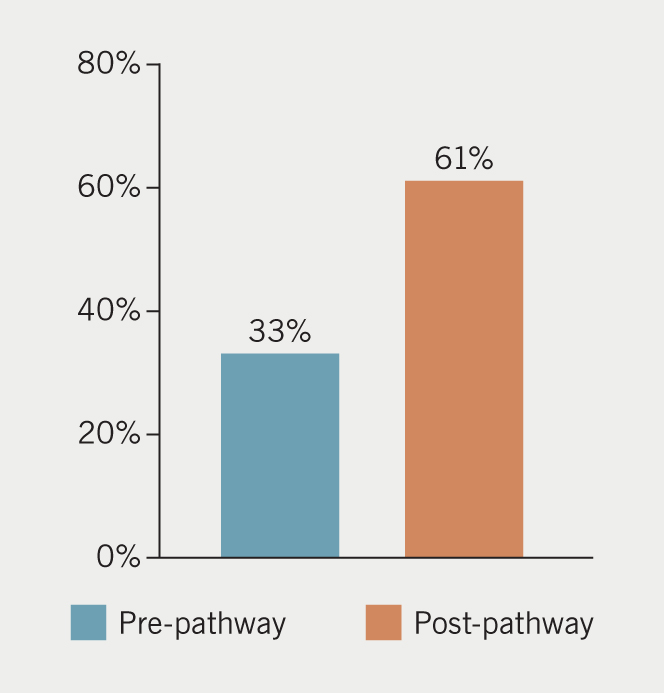
Non-HDL reduction
The percentage of those achieving the NICE target of a >40% reduction in non-HDL increased by 48% in the post-pathway group compared with the pre-pathway group (figure 2). Females were also more likely to achieve this target in the post-pathway group with 70% achieving a >40% reduction in non-HDL compared with 56% of males.
Discussion
The mean age of patients in this study is comparable with those in NACR’s 2019 Quality and Outcomes Report. Other key studies in this field have slightly lower mean ages, having excluded more elderly patients.8 More elderly patients may not be eligible for more aggressive lipid management owing to an increased risk of liver disease and polypharmacy,9 which may account for exclusion of more elderly patients from other clinical research. However, with patients living longer and more surviving myocardial infarction (MI),10 there will continue to be more elderly patients requiring CR input and effective lipid management. This study gives an accurate representation of the management of lipid levels among the local population.
There was a higher proportion of male patients in the younger age groups, with numbers in each gender group becoming more equally distributed around age 60 years. The mean female age at the time of their cardiac event was 72.9 years and the mean male age was 67.3 years. Based on current knowledge of demographical trends in coronary heart disease (CHD), the results will be relevant to the wider target population.
The rate of NSTEMI (59%) was higher than STEMI (37%), without disparity between genders, in keeping with national audit figures.10
ESC/EAS1 recommend a follow-up lipid profile four to six weeks after the start of treatment, whereas NICE2 recommends that a repeat lipid sample is taken about three months after the start of treatment. Allowing a longer period between samples may give a more accurate depiction of the effect of the current LLT, but this delay between samples has been observed locally to result in lack of follow-up lipid profiles and, potentially, missed opportunities for optimisation of LLT, perhaps owing to an average CR duration of three months.
It was felt that by re-checking at four to six weeks, those presenting with persistently elevated lipid levels despite their current LLT could be identified earlier, allowing increased opportunity during CR for discussion around concordance, diet, and other options for further optimisation of their LLT.
A marked improvement in the overall attainment of lipid target goals was observed (figure 1). LDL-C target attainment has been found to be generally poor, particularly among very high-risk groups, women, and those with a history of chronic kidney disease (CKD) and ischaemic stroke.11-14 Several themes emerge from analysis of the literature, including clinician perception of LDL-C targets,15 and under-utilisation of add-on therapies, such as ezetimibe.11-13,15,16 The pre-pathway audit supported the findings of the literature, and the LMP was, therefore, designed with these themes in mind.
ESC/EAS guidance1 recommends aiming to achieve both LDL-C of <1.4 mmol/L and a 50% reduction in LDL-C. As part of the data analysis for this study, these targets were measured both independently and in combination. The most significant improvement noted was those who achieved either an LDL-C <1.4 mmol/L, or >50% reduction, or both. This improvement points to a significant CHD risk reduction benefit to patients.
NICE’s 2014 guidance is to aim for a >40% reduction in non-HDL: 33% of patients achieved the non-HDL target in the pre-pathway cohort, compared with 61% in the post-pathway cohort – a significant improvement. Females (70%) were more likely to achieve this target than males (56%), which is unusual given the consensus among researchers that females are generally less likely to achieve their lipid targets.6 Females in the post-pathway cohort were also more likely to have >50% reduction in LDL-C. There was no gender demographic discrepancy between the cohorts to account for this, and the mean baseline LDL-C and non-HDL levels were also similar, hence, it can be assumed that the LMP facilitated an improvement in lipid target achievement, particularly in females.
Limitations
The sample size was small, and while smaller sample sizes have potential to lack accuracy,17 the cohort was representative demographically of the target population, as demonstrated by its consistency with national cardiac audit data.
The retrospective collection of data is a recognised limitation. The data for this study were not collected for the sole purpose of the study and, therefore, data extraction was less straightforward.
Inevitably, optimisation of lipid-lowering therapy, if not achieved with the initial LLT, takes longer, owing to the need to adequately trial different therapies. It is, therefore, acknowledged that a longer follow-up period could have rectified this and offered richer data, potentially offering a more accurate analysis of the LMP as a tool to support lipid target attainment.
Conclusion and recommendations
The findings indicate that the development and implementation of the LMP has been successful in improving the attainment of lipid goals, beyond those achieved in other parts of the UK and Europe.
The ability of CR programmes to facilitate lipid goal attainment has been highlighted. Non-medical prescribers may have further complemented this, although as full pharmacological data were not collected as part of this audit, it is not possible to draw this conclusion without further audit taking place. To date, there are no other published studies evaluating any other such tools, so this study offers valuable insight into the potential a LMP can provide in improving lipid levels in a post-ACS cohort of CR patients, thus supporting CV risk reduction.
Key messages
- The use of a lipid management pathway (LMP) appears to have had a significant impact upon the attainment of lipid goals
- Future investment in cardiac rehabilitation (CR) services could further enhance the attainment of lipid goals, allowing increased opportunities for patient monitoring, education and lipid-lowering treatment (LLT) optimisation
- CR clinicians are in a prime position to support cardiovascular risk reduction, which includes the reduction of low-density lipoprotein cholesterol (LDL-C) to help prevent future disease progression and incidence of myocardial infarction (MI)
Conflicts of interest
None declared.
Funding
None.
Study approval
The main ethical risks with clinical audit identified by The Healthcare Quality Improvement Partnership18 include the maintenance of anonymity and confidentiality. The data collection proforma was designed so as not to include any patient identifiable information and the information was gathered by the sole investigator.
Editors’ note
See accompanying article by Khan and Rakhit in this issue.
References
1. Mach F, Baigent C, Catapano AL et al. ESC/EAS 2019 guidelines for the management of dyslipidaemias: lipid modification to reduce cardiovascular risk. Eur Heart J 2020;41:111–88. https://doi.org/10.1093/eurheartj/ehz455
2. National Institute for Health and Care Excellence. Cardiovascular disease: risk assessment and reduction, including lipid modification. CG181. London: NICE, 2014. Available from: https://www.nice.org.uk/guidance/cg181
3. Collins R, Reith C, Emberson J et al. Interpretation of the evidence for the efficacy and safety of statin therapy. Lancet 2016;388:2532–61. https://doi.org/10.1016/S0140-6736(16)31357-5
4. Wong ND, Chuang J, Wong K, Pham A, Neff D, Marrett E. Residual dyslipidemia among United States adults treated with lipid modifying therapy (data from National Health and Nutrition Examination Survey 2009–2010). Am J Cardiol 2013;112:373–9. https://doi.org/10.1016/j.amjcard.2013.03.041
5. Kotseva K, Wood D, De Bacquer D et al.; EUROASPIRE Investigators. EUROASPIRE IV: a European Society of Cardiology survey on the lifestyle, risk factor and therapeutic management of coronary patients from 24 European countries. Eur J Prev Cardiol 2016;23:636–48. https://doi.org/10.1177/2047487315569401
6. Harris DE, Lacey A, Akbari A et al. Achievement of European guideline-recommended lipid levels post-percutaneous coronary intervention: a population-level observational cohort study. Eur J Prev Cardiol 2021;28:854–61. https://doi.org/10.1177/2047487320914115
7. British Heart Foundation. The national audit of cardiac rehabilitation: quality and outcomes report 2019. London: BHF, 2019. Available from: https://www.bhf.org.uk/informationsupport/publications/statistics/national-audit-of-cardiac-rehabilitation-quality-and-outcomes-report-2019
8. Zafrir B, Saliba W, Jaffe R, Sliman H, Flugelman MY, Sharoni E. Attainment of lipid goals and long-term mortality after coronary-artery bypass surgery. Eur J Prev Cardiol 2019;26:401–08. https://doi.org/10.1177/2047487318812962
9. Zhang N, Sundquist J, Sundquist K, Ji J. An increasing trend in the prevalence of polypharmacy in Sweden: a nationwide register-based study. Front Pharmacol 2020;11:326. https://doi.org/10.3389/fphar.2020.00326
10. National Institute for Cardiovascular Outcomes Research (NICOR). Myocardial ischaemia national audit project: 2019 summary report (2017/2018 data). London: NICOR, 2019. Available from: https://www.nicor.org.uk/wp-content/uploads/2019/09/MINAP-2019-Summary-Report-final.pdf
11. Farmakis I, Zafeiropoulos S, Pagiantza A et al. Low-density lipoprotein cholesterol target value attainment based on 2019 ESC/EAS guidelines and lipid-lowering therapy titration for patients with acute coronary syndrome. Eur J Prev Cardiol 2020;27:2314–17. https://doi.org/10.1177/2047487319891780
12. Ferrieres J, De Ferrari GM, Hermans MP et al. Predictors of LDL-cholesterol target value attainment differ in acute and chronic coronary heart disease patients: results from DYSIS II Europe. Eur J Prev Cardiol 2018;25:1966–76. https://doi.org/10.1177/2047487318806359
13. Halcox JP, Tubach F, Lopez-Garcia E et al. Low rates of both lipid-lowering therapy use and achievement of low-density lipoprotein cholesterol targets in individuals at high-risk for cardiovascular disease across Europe. PLoS One 2015;10:e0115270. https://doi.org/10.1371/journal.pone.0115270
14. Harris DE, Lacey A, Akbari A et al. Early discontinuation of P2Y12 antagonists and adverse clinical events post-percutaneous coronary intervention: a hospital and primary care linked cohort. J Am Heart Assoc 2019;8:e012812. https://doi.org/10.1161/JAHA.119.012812
15. Laufs U, Karmann B, Pittrow D. Atorvastatin treatment and LDL cholesterol target attainment in patients at very high cardiovascular risk. Clin Res Cardiol 2016;105:783–90. https://doi.org/10.1007/s00392-016-0991-z
16. Banefelt J, Lindh M, Svensson MK, Eliasson B, Tai M. Statin dose titration patterns and subsequent major cardiovascular events in very high-risk patients: estimates from Swedish population-based registry data. Eur Heart J Qual Care Clin Outcomes 2020;6:323–31. https://doi.org/10.1093/ehjqcco/qcaa023
17. Polit DF, Beck CT. Essentials of nursing research: appraising evidence for nursing practice. 9th ed. China: Walters Kluwer, 2018.
18. Healthcare Quality Improvement Partnership. Guide to managing ethical issues in quality improvement or clinical audit projects. London: HQIP, 2017. Available from: https://www.hqip.org.uk/wp-content/uploads/2017/02/guide-to-managing-ethical-issues-in-quality-improvement-or-clinical-audit-projects.pdf
