This paper summarises ‘Share The Pressure’, a project that developed and piloted a scalable model for engaging patients on the benefits of risk factor control for healthy ageing; training healthcare professionals (HCPs) in cardiovascular disease (CVD) risk communication; and improving the shared decision-making process between nurses, pharmacists and patients. The study features the use of a CVD risk tool called Heart Age, which has been shown to effectively motivate risk factor reduction in individuals.
The study team engaged virtually with patients and HCPs through established relationships within the community, third sector, charities, and social media. In addition, patients living with high blood pressure (hypertension) participated via online focus groups and surveys, which provided insight into patients’ preferences for conveying CVD risk, quantification of intervention benefits, side effects and processes to facilitate shared decision-making.
This insight gained from the focus group and survey data informed adaptations made to the Heart Age tool to provide ‘years off’ – or lowering of heart age – benefits for different aspects of blood pressure lowering, focusing on the independent and joint benefits of medication management and lifestyle.
The study piloted a training programme for nurses and pharmacists to support them in communicating and framing risk and intervention benefits.
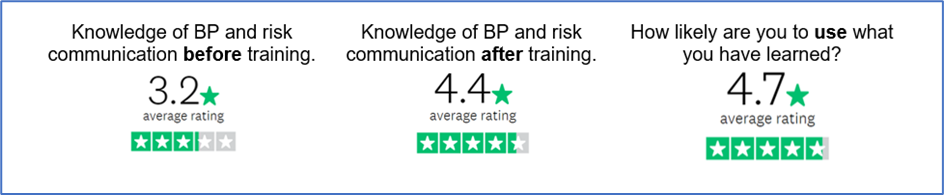
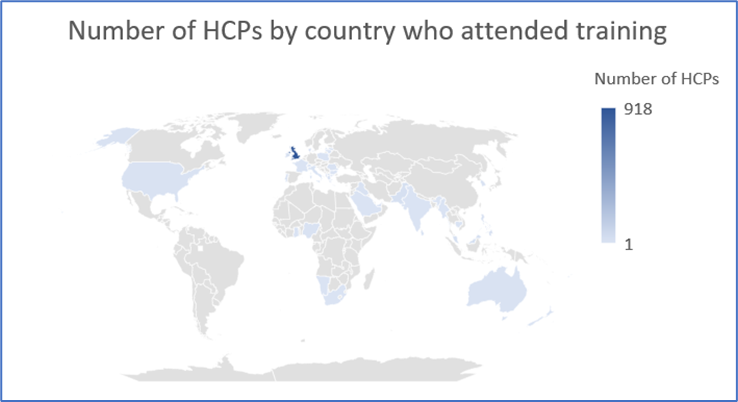
The study trained 1,148 HCPs from 37 countries over 17 sessions. Post-training survey results of HCPs indicated an increase in self-rated knowledge and a strong likelihood of applying information learned to their clinical practice. In addition, the Heart Age users found the personalised report and Heart Age test results very motivating for patients with high blood pressure.
Introduction
High blood pressure (BP) is a major risk factor for reduced healthy life-expectancy and unhealthy ageing. While it is fundamentally treatable, it is currently not optimally managed. To meet national public health targets, patients must play an active role in their decisions about how best to manage their own BP through lifestyle change and drug treatment.1,2
This paper summarises ‘Share The Pressure’ (STP), a project that developed and piloted a scalable model for engaging patients on the benefits of risk factor control for healthy ageing; training healthcare professionals (HCPs) in cardiovascular disease (CVD) risk communication and to engage patients around the benefits of understanding risk factor control to enable healthy ageing (age-based approaches have been demonstrated to be motivating for patients). Thus, to improve shared decision-making processes between nurses, pharmacists, and patients. The study features the use of a CVD risk tool called Heart Age,3 which has been shown to effectively motivate risk factor reduction in individuals.4
HCPs must establish an effective dialogue with patients around the benefits of living a healthy and long life and the importance of BP control. The STP project focused on nurses and pharmacists who engage with patients in primary care and community settings. The project aimed to enable nurses and pharmacists to participate in meaningful dialogue with patients living with high BP about its impact on CVD risk and equip patients with the tools to allow them to understand the benefits of different risk reduction approaches.
Effective control of BP and increasing physical activity are known to impact healthy life-expectancy in patients diagnosed with hypertension. However, to have a meaningful impact on this condition – a crucial driver of healthy ageing – patients must play an active role in decisions about the management of their disease. This ‘shared decision-making process’ sits at the heart of national hypertension control guidelines – and arguably the fundamental ethics of patient care.
Reducing high BP cannot be achieved without patients actively participating in lifestyle changes or medication adherence. Patients’ decisions about lifestyle changes and medication should be communicated in the context of their actual and perceived CVD risk. However, evidence shows that a mismatch exists between the perception of risk and measured risk in patients at all levels of CVD risk. For example, the REACT (Reassessing European Attitudes about Cardiovascular Treatment) survey demonstrated that the individual perception of CVD risk in five European countries was lower than the measured risk.5
The revised National Institute for Health and Care Excellence (NICE) guideline, Hypertension in adults: diagnosis and management,6 supports a shared decision-making approach to care. The guideline includes a patient decision aid (PDA) for hypertension in adults to support HCPs to explain trade-offs between reducing the risk of CVD and the disutility of taking daily medicines, monitoring requirements and the possibility of side effects; and help people with hypertension make more informed decisions about whether to take medicines at all; whether to add extra medicines to their treatment; and, if so, which medicines they would like to try.7
Study design
The STP project used a mixed-methods study design, over five project stages. Stages 1 and 2 focused on identifying current approaches and barriers to optimal patient communication. This served to generate insights, engage stakeholders, and promote their role in the project’s ongoing development and provide stimulus to adapt the CVD risk tool (Heart Age) that we planned to use in the programme. This project built on previous work applying the use of Heart Age to patient populations in the community and within healthcare practices. Previous work has primarily been conducted in the UK, Australia and the US; however, we have also implemented Heart Age in Singapore and the Middle East. Furthermore, the Joint British Societies for Cardiovascular Disease have implemented a form of Heart Age in their CVD risk app, which has been deployed by the former agency, Public Health England.
During stage 3, adaptations were made to the Heart Age tool derived from the findings from stage 2. These modifications were tested with a small group before launching a final version of Heart Age. Both this stage and the subsequent stage (stage 4), focused on the development, testing and roll-out of a training programme for HCPs.
Stage 5 focused on evaluating and identifying a sustainability plan for longer-term usage after the pilot was completed.
Before these stages, we established a steering group to provide strategic and tactical project oversight.
Results
The STP project commenced in January 2020. By March 2020, the COVID-19 pandemic forced governments worldwide – including the four nations of the UK – to introduce population-wide physical distancing restrictions. The combination of these restrictions and the significant diversion of healthcare resources towards the management of COVID-19 resulted in substantial reductions in screening and routine patient care. Furthermore, due to the considerable pressure facing primary-care professionals during the pandemic, the Quality and Outcomes Framework (QoF) was discontinued in 2020,8 including metrics related to BP measurement.
The project methodology was adapted in response to the pandemic, most notably by transferring to virtual engagement with HCPs. As a result, 1,148 HCPs from 37 countries engaged over 17 training sessions, significantly surpassing the target number of 60 nurses and pharmacists in England and Ireland; 918 participants were from the UK and 16 from Ireland. In addition, post-training feedback via electronic survey was positive, rating knowledge before training at 3.2/5 to 4.4/5 afterwards and 4.7/5 for how likely to use what they had learned in clinical practice.
This was an important finding as significant knowledge gaps were revealed in a blood pressure quiz offered over social media, via nursing groups on Facebook and Twitter (table 1). To note, the quiz was available to all, so some respondents were not HCPs.
Table 1. Results of 1,348 blood pressure quizzers
| 1,348 quizzers completed 10 multiple-choice questions | |||
|---|---|---|---|
| Lowest score | 8% | Highest score | 100% |
| Mean score | 64% | Median score | 68% |
| Multiple-choice questions | Mean score per question | ||
| Which of these medications would be a recommended first-line choice for a 48-year-old male of South Asian Origin? | 31% | ||
| At which of these levels of cardiovascular risk would antihypertensive medications be indicated in stage one hypertension? | 36% | ||
| Which two types of blood pressure readings are required to assess for hypertension? | 53% | ||
| What should you do first before adding in a new antihypertensive medication? | 54% | ||
| Which two of these sets of readings would confirm a diagnosis of stage one hypertension? | 63% | ||
| If a diagnosis of stage one hypertension is made, which two things needs to happen next? | 69% | ||
| How do we assess target organ damage? | 73% | ||
| What should you do before measuring blood pressure? (choose as many as you want to) | 90% | ||
| What could be a helpful strategy to support your patients to improve their blood pressure? | 96% | ||
Patient engagement was more complicated digitally due to challenges and illness associated with COVID-19. However, despite these challenges, survey and focus-group results indicated that patients feel strongly that there is a need for better shared decision-making with their HCPs. They also provided valuable feedback about what resources they needed and the applicability of Heart Age tool.
Patient insights (pre-Heart Age tool adaptation)
In total, there were 65 patients engaged across a survey (n=62) and in-depth interviews (n=3). The age spread was 41.5% (n=27) 31–50 years, 38.5% (n=24) 51–65 years, and 20% (n=13) 66–80 years. Most were female (69% n=44), with 18 (28%) males, one (1.5%) transgender and one (1.5%) who preferred not to say. Ethnicity was 95.5% (n=61) white, 3% (n=2) Asian and 1.5% (n=1) Black.
Patients complained about their HCP’s lack of explanation about their high BP and the impact of medications. They shared that there is minimal discussion about lifestyle from HCPs during appointments; instead, dialogue is focused mainly on medication. Also, patients observed that medical jargon is widespread and somewhat meaningless, e.g. stage 1 or 2 hypertension. Subsequently, patients turn to social media groups for explainers, such as the Facebook Blood Pressure UK group (from which we recruited).
Patient feedback also clarified that Heart Age resonates with them, given their age and their feelings of susceptibility due to being older. It must be accompanied by information that equips and prepares them for a conversation with an HCP about their BP. When survey respondents answered the question “Would you agree that you and your healthcare professional worked together to decide how to manage your blood pressure?” only 8.33% said strongly agree, 31.67% somewhat agreed, and 45% somewhat or strongly disagreed.
The Heart Age tool has been widely used and previously studied through randomised trials.4,9-11 These studies have found Heart Age to be an effective CVD risk communication tool and that it can also increase patients’ physical activity. As a result, it has been adopted for use by leading organisations in numerous countries. Through STP, we harness HCP and patient insights to refine the Heart Age tool and enable it to be more patient-centric and fit for use.
The project also showed that patients found HCP’s reliance on and use of medical jargon is a substantial information access barrier and that it can be a prompt for them to turn to social media groups to understand their health condition. This poses a significant threat as it exposes them to information and recommendations that may not be evidence-based. Therefore, online information about the STP platform needed to be accessible, easy-to-read and informative, while making clear the current evidence about lowering BP.
Patients also observed a fragile balance between receiving too much information before an appointment with their HCP, which can be overwhelming, and receiving too little information, which prevents them from appropriately preparing questions to ask. Information offering excessive detail before an appointment can lead to anxiety. However, it remains essential to know what questions to ask your doctor, e.g. how long might I be on medication? And/or what are the side effects? Patients felt that having the correct information available before and after appointments was important to manage anxiety at different stages and take away afterwards.
Engagement with HCPs illustrated an appetite to increase and enhance their knowledge around hypertension and use tools such as Heart Age to improve their engagement with patients. Unfortunately, in the COVID-19 context, suspension of QoF prevented HCPs from immediately putting Heart Age into practice with patients.
Discussion
The STP project found that patients want to know their Heart Age results, are interested in understanding hypertension and want to be more engaged in decision-making about their management in partnership with their HCPs (table 2). Furthermore, the project was conducted during the unprecedented COVID-19 pandemic. As a result, patients acknowledged the importance of hypertension as a critical non-communicable disease risk factor, a risk factor for serious illness from COVID-19 and the importance of playing an active role in their health.
Table 2. What patients want to know more about to help manage their blood pressure
| Questions and answers | Mean response N=62 |
|---|---|
| 1. What would help you make a decision about whether to take tablets for your blood pressure? (could choose more than one answer) | |
| Knowing how important blood pressure is | 55.17% |
| How serious my own risk of a heart attack or stroke is | 74.14% |
| Understanding how taking tablets every day can reduce my risk of a heart attack or stroke | 51.72% |
| What the side effects might be of taking tablets every day | 46.55% |
| How to remember to take my tablets every day | 12.07% |
| None of these | 8.62% |
| 2. What would help you make a decision about whether to become more active or take exercise to manage your blood pressure? (could choose more than one answer) | |
| Knowing how important blood pressure is | 39.66% |
| How serious my own risk of a heart attack or stroke is | 55.17% |
| Understanding how doing physical activity or exercise every day for 30 minutes can reduce my risk of a heart attack or stroke | 67.24% |
| What different types of physical activity/exercise can help | 51.72% |
| How I can fit 30 minutes of physical activity/exercise into my normal day | 29.31% |
| 3. Which of the following works best for you in making decisions about your blood pressure? | |
| A healthcare professional makes the decision for me | 12.07% |
| A healthcare professional gives me all the information I need and we make a decision together | 65.52% |
| A healthcare professional gives me all the information I need and then I make the decision myself | 22.41% |
Table 3. What healthcare professionals say would help them to help patients
| What would help you to help patients? |
|---|
| Training |
|
| Practical support |
|
| Key: ABPM = ambulatory blood pressure monitoring; BP = blood pressure; HBPM = home blood pressure measurement |
The project also found that HCPs want to deepen their understanding of hypertension and improve their ability to support patients living with it (table 3).
They were keen on further training and engaged well with the project’s adapted training model. Although the original project methodology included face-to-face training to demonstrate the Heart Age tool, there was no loss in the perceived value when presented to HCPs during virtual training sessions. HCPs indicated that they could visualise using it to aid their clinical management and conversations with patients. It was only due to COVID-19 and the subsequent effect on the clinical work environments, e.g. the suspension of QoF and the lack of in-person care, that HCPs could not use the tool immediately after participating in a training session.
STP has enabled both patients and HCPs to think differently about hypertension. As a result, the 1,148 HCPs in the training programme increased their knowledge of BP and risk communication score from 3.5/5 to 4.4/5, and likelihood of using what they have learned is 4.7/5 (appendix 1).
The project modification relating to the delivery of training sessions to HCPs, i.e. from face-to-face to virtual training, ultimately allowed the project to exceed the target number of HCPs engaged in numbers of participants across 37 countries reached (appendix 2). This has dramatically enhanced accessibility by HCPs and enabled those who may otherwise have been unable to access face-to-face training. Although much of healthcare has accelerated the use of digitally based care since the start of the COVID-19 pandemic, care must be taken to ensure people who do not have access to technology are not being digitally excluded.
Limitations
The COVID-19 pandemic meant recruitment of patients had to deviate from the original plan of through HCPs. Most of the people involved were from a BP Facebook group, which then limited who could respond. While there was good inclusion of women, there was a very low uptake from people with Asian or Black heritage. Most of the HCPs trained were nurses and so the outcome of both usability of the tool and potential improvement of doctors’ knowledge is unknown. The survey had age ranges for people to select, which meant the mean age of patients could not be calculated. Patients who participated tended to be younger.
Conclusion
The implications for clinical practice from STP are multiple. The project has demonstrated an innovative working model that is fit for purpose within the clinical practice of the NHS. Evidence from the project indicates interest and knowledge acquisition around hypertension and risk communication by HCPs in the UK and other countries. The challenge now is to see if STP can be used to support patients in the future and help the NHS with the post-COVID-19 recovery. The project was supported by Viatris Inc., a biopharmaceutical company, and demonstrates the importance of private–public partnership models in combating hypertension – a major risk factor for CVD and the most common non-communicable disease globally. Share The Pressure 2 started in August 2022, tailored to people of African and African-Caribbean heritage with funding by The Burdett Trust for Nursing.
Key messages
- While hypertension remains a major risk factor for reduced life-expectancy and healthy ageing, there remains a significant gap in healthcare professionals’ knowledge
- Patients want to understand how their blood pressure affects their heart attack or stroke risk and be involved in shared decision-making about their care
- Share The Pressure, utilising the Heart Age tool, supported by a training programme, is ideal for delivering both
Conflicts of interest
MN is a director at Smart Health Solutions. MC is employed by Younger Lives Ltd., a company specialising in the development of risk communication and behaviour change tools to use with patients. SD is a full-time employee of Viatris Inc. JH is a contractor at Smart Health Solutions.
Funding
The project was supported by Viatris Inc., a biopharmaceutical company.
Study approval
All participants were fully informed of the requirements of the study and what was asked of them prior to participation. We required active consent and this was free to be removed at any stage. The purpose of the research was to evaluate current understanding of blood pressure, the Heart Age tool and discussions with their healthcare professional. Online data provided were anonymous and interviews conducted under strict confidentiality with personal details removed as soon as the interviews were terminated. To ascertain whether we required a formal NHS ethics review we used the tool at https://www.hra-decisiontools.org.uk to get guidance from the NHS Health Research Authority. The feedback from the tool was that an ethical review was not required.
References
1. Public Health England. Health matters: preventing cardiovascular disease. London: Public Health England, 2019. Available from: https://www.gov.uk/government/publications/health-matters-preventing-cardiovascular-disease/health-matters-preventing-cardiovascular-disease [accessed January 2022].
2. National Health Service. The NHS long term plan. London: DoH, 2019. Available from: https://www.longtermplan.nhs.uk/publication/nhs-long-term-plan/
3. Share The Pressure website. Available at: https://www.sharethepressure.com/
4. Lopez-Gonzalez AA, Aguilo A, Frontera M et al. Effectiveness of the Heart Age tool for improving modifiable cardiovascular risk factors in a Southern European population: a randomized trial. Eur J Prev Cardiol 2015;22:389–96. https://doi.org/10.1177/2047487313518479
5. Erhardt L, Hobbs FDR. Public perceptions of cardiovascular risk in five European countries: the REACT survey. Int J Clin Pract 2002;56:638–44. https://doi.org/10.1111/j.1742-1241.2002.tb11344.x
6. National Institute for Health and Care Excellence. Hypertension in adults: diagnosis and management. NG136. London: NICE, 2019. Available from: https://www.nice.org.uk/guidance/ng136
7. National Institute for Health and Care Excellence. How do I control my blood pressure? Lifestyle options and choice of medicines. Patient decision aid. London: NICE, 2019. Available from: https://www.nice.org.uk/guidance/ng136/resources/how-do-i-control-my-blood-pressure-lifestyle-options-and-choice-of-medicines-patient-decision-aid-pdf-6899918221
8. National Health Service. Update to GP contracts. London: NHS, 9 July 2020. Available from: https://www.england.nhs.uk/coronavirus/wp-content/uploads/sites/52/2020/03/C0569-Second-phase-of-General-Practice-response-to-COVID-19–update-to-GP-contracts-and-income-protection-a.pdf
9. Soureti A, Hurling R, Murray P, van Mechelen W, Cobain M. Evaluation of a cardiovascular disease risk assessment tool for the promotion of healthier lifestyles. Eur J Cardiovasc Prev Rehabil 2010;17:519–23. https://doi.org/10.1097/HJR.0b013e328337ccd3
10. Soureti A, Murray P, Cobain M, van Mechelen W, Hurling R. Web-based risk communication and planning in an obese population: exploratory study. J Med Internet Res 2011;13:e100. https://doi.org/10.2196/jmir.1579
11. Bonner C, Raffoul N, Battaglia T, Mitchell JA, Batcup C, Stavreski B. Experiences of a national web-based heart age calculator for cardiovascular disease prevention: user characteristics, Heart Age results, and behavior change survey. J Med Internet Res 2020;22:e19028. https://doi.org/10.2196/19028
