This case report explores the effects of myocarditis induced by coronavirus disease 2019 (COVID-19) on a cardiac implanted electronic device (CIED) and its ability to differentiate depolarisation and repolarisation. Through the modification of the device settings, inappropriate CIED discharges were prevented for the duration of the illness in this 76-year-old male patient. This provides supporting evidence to consider episodes of acute COVID-19 as a cause for T-wave oversensing (TWOS).
Introduction
T-wave oversensing (TWOS) is a well-recognised phenomenon encountered in cardiac implantable electronic devices (CIEDs), particularly in high-energy platforms.1 TWOS occurs when the ventricular repolarisation signal, corresponding to the surface ECG T-wave, is mistakenly identified as a de novo depolarisation by the device. The principal effect of this is to ‘double count’ the heart rate. This may lead the device to mistakenly register a ventricular rate high enough to reach the threshold for detection of a tachycardic episode, which may in turn precipitate the CIED to inappropriately discharge. TWOS may be seen for a number of reasons,2,3 including clinical factors that alter the T-wave morphology and timing, as well as programming set-up and changes.
Case presentation
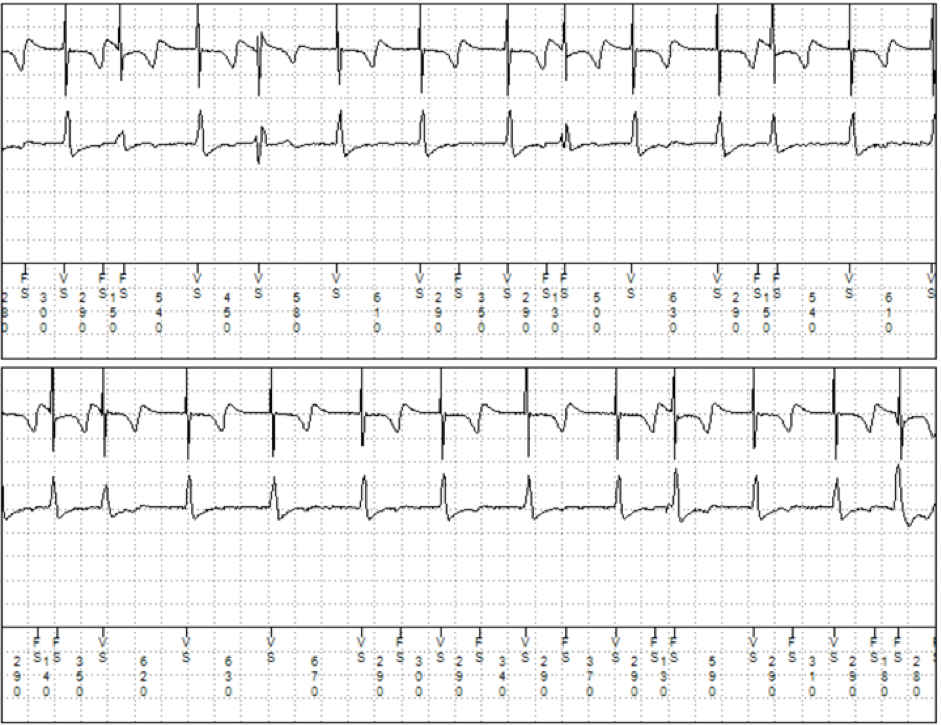
A 76-year-old male patient had a single-chamber single-coil implantable cardiac defibrillator (Visia AF MRI S VR, Medtronic Ltd., Watford) inserted in 2018 for primary prevention in the setting of persistent atrial fibrillation and severe left ventricular systolic dysfunction as a consequence of an ischaemic cardiomyopathy. All subsequent device follow-up checks were satisfactory until a remote monitoring alert was received in September 2022. Subsequent interrogation and analysis demonstrated over 500 episodes of TWOS within this short period of time (figure 1). This was correlated with a clinical picture of acute coronavirus disease 2019 (COVID-19) in association with a positive home swab test. A minor change was made to the sensitivity of the device to prevent TWOS in the short term. He was seen four weeks later when his COVID-19 symptoms had resolved; no further TWOS was identified. He remained free of TWOS episodes during his ongoing follow-up in the subsequent 12 months. Notably, there was no imaging, laboratory serology or troponins evidenced in this case.
Discussion
The case presented herein describes a case where a longstanding implanted, well-functioning, high-energy CIED demonstrated a transient period of TWOS correlating with COVID-19.
The development of clinically apparent myocarditis is a recognised complication of COVID-19,4 although the exact incidence is still undetermined. There is some evidence that the myocardial injury caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection may be more severe than viral myocarditis caused by other organisms.5
Hyperacute T-waves mediated through myocardial ischaemia have previously been described as a cause for TWOS, with resolution of the issue after revascularisation.6 There is a large body of published work describing the range of surface ECG T-wave changes that may additionally be seen,7 and Doyen et al. correlated significant changes in ECG and serum troponin levels in people with COVID-19.8 Barman et al. demonstrated significant T-wave inversion and ST-T changes in both severe and non-severe COVID-19.9
Conclusion
COVID-19 may manifest a number of cardiac findings due to ischaemia, myocarditis and pericarditis. Although these may have clinical relevance in their own right, particular care is needed in patients with CIEDs due to the risks of TWOS. COVID-19 should be considered as a diagnosis in patients who present with unheralded TWOS in the absence of other identifiable causes.
Key messages
- The development of clinically apparent myocarditis is a recognised complication of COVID-19, although the exact incidence is unknown
- T-wave oversensing (TWOS) is a well-recognised phenomenon encountered in cardiac implantable electronic devices (CIEDs) and may represent cardiac pathology when presenting de novo in these cases
- TWOS may result in the inappropriate discharge of a CIED
- In patients with CIEDs who develop unprovoked TWOS, COVID-19 should be considered as a possible cause and temporary changes made to CIED settings with ongoing monitoring.
Conflicts of interest
None declared.
Funding
None.
Informed consent
Informed consent was obtained from the patient prior to publishing.
References
1. Swerdlow CD, Asirvatham SJ, Ellenbogen KA, Friedman PA. Troubleshooting implanted cardioverter defibrillator sensing problems I. Circ Arrhythm Electrophysiol 2014;7:1237–61. https://doi.org/10.1161/circep.114.002344
2. Chhabra L, Khalid N, Kluger J. Myocardial ischemic hyperacute T-wave oversensing leading to a defibrillator shock storm. Proc (Bayl Univ Med Cent) 2015;28:200–3. https://doi.org/10.1080/08998280.2015.11929229
3. Siripanthong B, Nazarian S, Muser D et al. Recognizing COVID-19–related myocarditis: the possible pathophysiology and proposed guideline for diagnosis and management. Heart Rhythm 2020;17:1463–71. https://doi.org/10.1016/j.hrthm.2020.05.001
4. Patone M, Mei XW, Handunnetthi L et al. Risks of myocarditis, pericarditis, and cardiac arrhythmias associated with COVID-19 vaccination or SARS-COV-2 infection. Nat Med 2022;28:410–22. https://doi.org/10.1038/s41591-021-01630-0 [Epub online ahead of print]
5. Bortnik M, Fundaliotis A, Schaffer A, Occhetta E, Marino P. Transient hyperkalemia-induced T-wave oversensing as a cause of inappropriate ICD discharges. J Cardiol Cases 2013;8:164–7. https://doi.org/10.1016/j.jccase.2013.07.008
6. Topf A, Motloch LJ, Kraus J et al. Exercise-related T-wave oversensing: an underestimated cause of reduced exercise capacity in a pacemaker-dependent patient—a case report and review of the literature. J Interv Card Electrophysiol 2020;59:67–70. https://doi.org/10.1007/s10840-019-00698-6 [Epub online ahead of print]
7. Fernandez R, Mihos CG, Torres JL, Tolentino AO. Inappropriate pacing due to T-wave oversensing. J Thorac Dis 2020;12:2983–5. https://doi.org/10.21037/jtd.2020.02.19
8. Doyen D, Moceri P, Ducreux D, Dellamonica J. Myocarditis in a patient with covid-19: a cause of raised troponin and ECG changes. Lancet 2020;395:1516. https://doi.org/10.1016/s0140-6736(20)30912-0
9. Barman HA, Atici A, Alici G et al. The effect of the severity COVID-19 infection on electrocardiography. Am J Emerg Med 2021;46:317–22. https://doi.org/10.1016/j.ajem.2020.10.005
