Renal denervation (RDN) revisited
A novel, catheter-based technique is looking promising for the treatment of refractory hypertension. Renal sympathetic hyperactivity is associated with the development of hypertension and its progression, as well as chronic kidney disease (CKD) and heart failure. While sympathectomy procedures have been considered over the past 50 or more years, it is now possible, using a steerable femoral 6F catheter with an RF energy electrode tip, to deliver a series of 2 minute ablations to the renal artery, causing renal denervation (RDN) and blood pressure reduction.
 An initial proof of principle study was reported in The Lancet (Krum H et al. Lancet 2009;373:1275–81) by Dr Henry Krum (Monash University, Melbourne, Australia) and co-investigators who, using the newly developed Symplicity® catheter system, performed RDN in 45 patients with resistant hypertension (systolic blood pressure [SBP] ≥160 mmHg on three antihypertensive agents); the procedure lasting a median of 38 minutes. The primary end points were office blood pressure (BP) and safety data at one, three, six, nine and 12 months, and patient’s renal angiography and magnetic resonance angiography during follow-up. BP was significantly reduced by, -14/-10, -21/-10, -22/-11, -24/-11 and -27/-17 mmHg at these pre-specified time points compared with five non-treated patients who had elevations in BP. Renal function (estimated glomerular filtration rate [GFR] and creatinine) was sustained and there were no renovascular complications. One intraprocedural renal artery dissection occurred before the ablation without sequelae.
An initial proof of principle study was reported in The Lancet (Krum H et al. Lancet 2009;373:1275–81) by Dr Henry Krum (Monash University, Melbourne, Australia) and co-investigators who, using the newly developed Symplicity® catheter system, performed RDN in 45 patients with resistant hypertension (systolic blood pressure [SBP] ≥160 mmHg on three antihypertensive agents); the procedure lasting a median of 38 minutes. The primary end points were office blood pressure (BP) and safety data at one, three, six, nine and 12 months, and patient’s renal angiography and magnetic resonance angiography during follow-up. BP was significantly reduced by, -14/-10, -21/-10, -22/-11, -24/-11 and -27/-17 mmHg at these pre-specified time points compared with five non-treated patients who had elevations in BP. Renal function (estimated glomerular filtration rate [GFR] and creatinine) was sustained and there were no renovascular complications. One intraprocedural renal artery dissection occurred before the ablation without sequelae.
The same team reported the two-year ‘durability’ of BP reduction among the cohort after RDN, during the ESH Congress. In all, 117 patients were treated at 17 centres. BPs were reduced by -20/-11, -24/-10, -24/-12, -25/-12, -29/-17 and -33/-14 mmHg at, one, three, six, 12, 18 and 24 months respectively. One patient required renal artery stenting for a lesion present at baseline, otherwise there were no adverse late events. Catheter-based RDN therefore appears to produce substantial reduction in BP sustained to at least two years and changes in eGFR “are better than the natural history reported in similar patients” say the authors. UK workers, notably at Barts & the London Hospital, are involved in further assessment of RDN as a treatment for resistant hypertension.
ROADMAP: olmesartan delays progression to microalbuminuria in type 2 diabetes
Can the presence of microalbuminuria act as a sensitive surrogate end point to identify early stages of preventable disease? This was the question posed by the ROADMAP study, which was presented at the meeting.
Explaining the rationale for the trial, the study’s lead investigator Dr Hermann Haller (Hannover Medical School, Hannover, Germany) said: “We are treating our patients too late and every diagnostic criteria we have to be able to treat early is important”. He called microalbuminuria an early window into a person’s vasculature: “Microalbuminuria is very strongly associated with future cardiovascular events and it is relatively easy to measure,” he added, saying he thought that of all the measurements for organ damage, microalbuminuria should, at the moment, be “number one”.
ROADMAP (Randomised Olmesartan and Diabetes Microalbuminuria Prevention) was set up to determine whether the angiotensin receptor blocker (ARB), olmesartan, could delay the onset of microalbuminuria in normoalbuminuric patients with type 2 diabetes and at least one additional cardiovascular risk factor, who had not received an ACE inhibitor or an ARB within the last six months.
The double-blind, randomised, controlled study was carried out in 262 centres in 19 European countries. Some 4,447 patients (mean age 57.7 +/- 8.72 years, mean systolic blood pressure 136 +/- 15 mmHg, mean diastolic blood pressure 81 +/- 10 mmHg) with type 2 diabetes (mean duration 6.1 +/- 6.0 years, BMI 31.0 +/- 14.91 kg/m2, HbA1c 7.65 +/- 1.62%) were randomised to either treatment with olmesartan 40 mg (n = 2,232) or placebo (n=2,215).
To reach the target blood pressure of < 130/80 mmHg, other antihypertensive agents were used with the exception of drugs affecting the renin-angiotensin- system. Follow-up was for 3.2 years and urinary albumin to creatinine ratio (UACR) was determined every six months. The primary end point was time to onset of microalbuminuria and secondary end points were cardiovascular and renal morbidity and mortality.
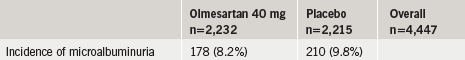
Results showed that patients in the olmesartan group had a significant 23% risk reduction (p= 0.01) in time to onset of microalbuminuria, the study’s primary end point (table 1). Blood pressure was very well controlled in the study with more than 75% of all patients achieving the blood pressure target of < 130/80 mmHg.
Safety
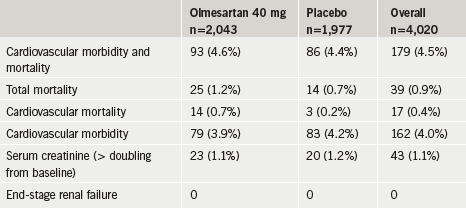
Results for secondary end points in the hypertensive sub population are summarised in table 2. Although results for the secondary end points were similar between the two groups, there was an increase in the numbers of cardiovascular deaths in the olmesartan group compared to the placebo group. This was also seen in the total study population where there were 15 cardiovascular deaths in the olmesartan group compared to three in the placebo group. Dr Haller maintained these numbers were low and not a cause for concern. He said analysis of the data had shown the higher cardiovascular mortality occurred only in those patients with existing cardiovascular disease and a low systolic blood pressure (i.e. < 120/mmHg). “This fits very nicely with the recommendations of the European guidelines that target blood pressure in patients with cardiovascular disease should be between systolic 130 and 140 mmHg,” he said.
He added that predictors for a better response to treatment with olmesartan were those with a higher baseline systolic blood pressure (>135 mmHg), a high UACR (> 4 mg/g), a low HbA1c (< 7.3%) and a low estimated glomerular filtration rate of 83.79. The majority of the effect on microalbuminuria appeared to be blood pressure independent.
Atrial fibrillation and hypertension
“Hypertension is the most prevalent risk factor leading to the development of atrial fibrillation (AF), the most common arrhythmia,” according to Dr I Grundvold (University of Oslo, Norway). In the ATHENA study with dronederone, for example, 86% of patients had hypertension. It is assumed that this risk increases with increasing blood pressure (BP) levels, but it is not known at which level systolic BP imposes a risk for AF.
He presented data from 2,014 apparently healthy men aged 45–59 years who were included in the Oslo Ischemia Study, between 1972–75 and who were followed for 35 years. By this time some 272 men (14% of total) had a diagnosis of AF. The adjusted risk of developing AF was increased by 63% for study participants with baseline BP >128 mmHg (p=0.0003) compared to participants with systolic BP <128 mmHg. This, therefore, represented a “strong, independent long-term predictor of AF” according to these investigators.
Salt controversy, the spice of life
High blood pressure is “the biggest cause of death in the world… and we must do something about it”, said Professor Graham MacGregor (Wolfson Institute of Preventive Medicine, Barts & The London School of Medicine and Dentistry, London).
A well-known advocate for dietary salt restriction, he said that the problem is predominantly one of salt intake, 80% of which is “hidden” in foods. Less is now used for food preservation, with the exception of anchovies and smoked salmon. Salt is also used as a binding agent, to hold water in meat and thus increase its weight and sales price. Similarly, salt is used to make “inedible things edible” and it is, of course, a major driver of thirst, leading to increases in soft sugar-containing drinks, to which children become addicted, leading to weight gain.
The goals in Professor MacGregors view are to get the UK population blood pressure down and to treat those with high blood pressure. He believes the adverse effects of dietary salt are overwhelming and we need to halve our intake to 4 g a day. This is “the most efficient and cheapest thing you can do for public health” he said.
The pressure group, Consensus Action on Salt and Health (CASH; www.actiononsalt.org.uk) for which he is Chairman, has been very successful in influencing the UK Department of Health and the Food Standards Agency in changing policy, and gaining public advocacy and support to bring pressure to bear on the food industry to reduce added salt levels. It issues a press release every six weeks. “The public in the UK know that salt is dangerous but they don’t know what to do about it,” he said. He is pleased with progress and major food manufacturers in the UK have been gradually reducing salt in their products at a rate of about 10–20% per year without rejection or public outcry. He believes that a 6 g a day salt target will be reached in the UK in the next four years.
This is in harmony with the recently launched UK National Institute for Health and Clinical Excellence (NICE) public health guidance on prevention of cardiovascular disease which recommends reducing mean salt intakes by 3 g a day for adults (to achieve a target of 6 g a day) and which would, in the UK, lead to around 14–20,000 fewer annual cardiovascular deaths each year (see page 163).
Professor MacGregor, with help from World Health Organisation, is rolling his message out worldwide. (See review; He FJ, MacGregor GA. Reducing population salt intake worldwide; from evidence to implementation. Prog Cardiovasc Dis 2010;52:363–82.
[www.onlinepcd.com]).
Leg over and blood pressure
 Crossing your leg over may not be good for your blood pressure! A team from Radboud University Medical Centre, Nijmegen, The Netherlands, has shown, in a study of 25 subjects, that the mere act of crossing their ankle over their knee, in the sitting position, caused considerable haemodynamic changes. For example, compared to the ‘uncrossed position’, blood pressure rose +11.4/+3.8 mmHg, mean arterial pressure (MAP) rose 7.0 mmHg and heart rate by 1.7 beats per minute. There were also increases in cardiac output and stroke volume. The authors recommend that all those who measure blood pressure should be aware of these effects and patients advised to keep their feet on the floor during measurements. They also suggest that, “the position of the legs should be mentioned in all guidelines and publications regarding blood pressure”.
Crossing your leg over may not be good for your blood pressure! A team from Radboud University Medical Centre, Nijmegen, The Netherlands, has shown, in a study of 25 subjects, that the mere act of crossing their ankle over their knee, in the sitting position, caused considerable haemodynamic changes. For example, compared to the ‘uncrossed position’, blood pressure rose +11.4/+3.8 mmHg, mean arterial pressure (MAP) rose 7.0 mmHg and heart rate by 1.7 beats per minute. There were also increases in cardiac output and stroke volume. The authors recommend that all those who measure blood pressure should be aware of these effects and patients advised to keep their feet on the floor during measurements. They also suggest that, “the position of the legs should be mentioned in all guidelines and publications regarding blood pressure”.
Hypertension trial round up
TALENT
It is important to achieve blood pressure control quickly. But is it more beneficial to start with combination antihypertensive therapy than to start with monotherapy and then add another drug, i.e. stepped care? This was the key question addressed in the TALENT study (a multicentre study evaluating Efficacy of Nifedipine GITS-Telmisartan Combination in blood pressure control and beyond:Comparison of two strategies).
The study recruited 405 high risk hypertensive patients in 40 centres in Spain and Italy. “The primary end point of TALENT, to assess 24-hour mean systolic blood pressure by ambulatory blood pressure monitoring (ABPM) after 16 weeks compared with baseline, was met,” according to Professor Luis Ruilope, Octuber Hospital, Madrid, Spain.
After eight weeks of treatment, the combination of nifedipine GITS 20 mg/telmisartan 80 mg reduced office blood pressure from a baseline of 153/90 mmHg to 138/83 mmHg, with a blood pressure-lowering effect evident at two weeks. The effect was achieved earlier than with monotherapy and the addition of another drug after eight weeks, leading Professor Ruilope to conclude that the message from this is: “don’t be afraid to use two drugs up front”.
ESPORT
Professor Gulianno Tocci (Rome, Italy) presented findings for a team of Italian and French investigators, looking at the efficacy and safety of olmesartan versus ramipril in 351 elderly hypertensive patients. The eight-week active treatment phase showed that olmesartan provided greater blood pressure normalisation compared to ramipril, and that this ARB should be considered a good first-line treatment in these patients. Similar findings were shown in the larger ESPORT study of 1,320 patients.
Commenting on the initial study, Professor Gordon McInnes (Glasgow) suggested that the findings may be explained by using ramipril as a comparator, which he believes is a less effective drug, which should be taken twice a day rather than once daily.
TEAMSTA
Professor M Volpe (Rome) presented the TEAMSTA study results. This looked at the combination of telmisartan 80 mg/amlodipine 10 mg versus their single components in over 800 patients with severe hypertension (blood pressure ≥180/95 mmHg). Again the combination was superior to monotherapies and 80% of the effect was seen early in the eight-week active treatment phase.
Antihypertensive combinations
In a review of which antihypertensive combination to use (ACE inhibitors or angiotensin receptor blockers with calcium channel blockers, when treating hypertension, Professor McInnes reminded delegates of the adage, “it’s the blood pressure, stupid” and he suggested we avoid “woolly thinking”.
Antihypertensives were probably much the same, he said, and what is most important is to use agents, which provide efficacious and sustained reduction of blood pressure.
In a discussion session, mention was made of a recent meta-analysis, which purported to show an increase in cancer in patients taking angiotensin receptor blockers. The view from Oslo was that this represented ‘junk science’ and looked selectively at data, out of context, and that it should be dismissed.
SHARE
Failure to reach blood pressure targets is often blamed on poor patient compliance with antihypertensive medication but it now seems that physician inertia must also be overcome.
Results from the SHARE (New Supporting Hypertension Awareness and Research Europe-wide) study showed that in a survey of 2,629 physicians in Europe, most (76%) felt the European Society of Hypertension guidelines blood pressure targets of 140/90 mmHg were ‘about right’. But the study highlighted the mean blood pressure that physicians became ‘concerned with’ was 149/92 mmHg and most physicians (78% and 61%, respectively) would not consider taking any action in general hypertensive patients until systolic and diastolic blood pressures were above 140 and 90 mmHg, respectively. Some (50%) would not take any action until blood pressure was higher than 168/100 mmHg.
The results also showed that physicians underestimate the number of challenging patients they treat. Challenging patients were defined as those not reaching a blood pressure goal of <140/90 mmHg – physicians estimated 34% of their patients were not at goal, while in reality, this number was 47%.
