Current statistics, available from outcomes following the National Service Framework (NSF) on Coronary Heart Disease,1 show that more people are surviving longer both after an acute coronary event and after a symptom-led diagnosis of coronary artery disease. In the past, cardiac rehabilitation (CR) played a key role in preventing premature mortality2 but more recently the greatly enhanced emergency services, better public education and more aggressive and widely available medical interventions may have diminished the effect of CR on premature mortality. There is now an increasing focus on productivity of life in those surviving acute myocardial events. Productivity refers to people’s active involvement in the local social and economic fabric of their families, friends and community. Some of these matters are less likely to be a function of technical medical care but rather a function of healthcare professionals providing therapeutic and health-promoting support for people to manage the physical, mental, domestic, occupational and social aspects of their lives – all of the goals at the heart of a good CR and chronic disease management and prevention programme.
WHO definition
The World Health Organization (WHO) defined CR in 1993 in a timeless way that is inclusive and sensitive to the psychosocial, biomedical, professional expertise and service delivery mode and location elements required of a contemporary CR service.
“The sum of activities required to influence favourably the underlying cause of the disease so that (people) may by their own efforts preserve, or resume when lost, as normal a place in the community…
…it must be integrated within secondary prevention services of which it forms one facet”.3
BACR definition
This article reflects on how this definition dovetails with the BACR Standards and Core Components and the various considerations required for delivering a successful CR service.
The WHO definition starts with the words, “the sum of activities”; the BACR describes these activities as its core components, including:4
- physical activity and exercise
- diet and weight management
- smoking cessation
- education
- risk factor management
- psychosocial elements
- cardioprotective drug therapy and implantable devices, and a
- long-term management strategy.
Figure 1 illustrates a model to show how the psychosocial and educational (health behavioural) component of CR has a central core role that is linked with the successful management or change of each of the other components.4 Figure 1 also aims to represent a patient-centred approach, again reflecting the WHO definition (…by their own efforts preserve, or resume when lost, as normal a place in the community).
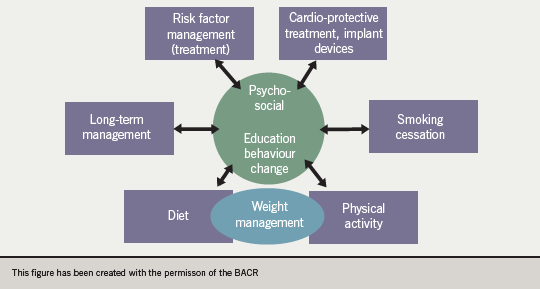
In this schematic, the patient’s psychosocial status and mental well-being as well as his or her readiness and ability to make health behaviour changes, supported through education and ‘motivation-to-change’ techniques, are at the core of achieving each of all the other components.
In facilitating the patient to take control of managing his or her own condition, CR services ideally need to provide each patient with the choice of receiving his/her programme in the setting most conducive to achieving the greatest chance of long-term adherence to a healthier lifestyle. Typical choices are a hospital, community or home-based programme; each of these venues has benefits and drawbacks. Without going into further detail, there is one underlying factor that needs to be ensured; that all the BACR Standards and Core Components should be provided, wherever the patient participates in the programme. Patients should all receive expert support, care and guidance in each of the components required to meet their individual needs.
Creation and definition of the success of a CR programme are concepts determined from examples of good practice. The BACR Standards are built on a foundation of scientifically proven studies.4 Contemporary work defines the need for an integrated multidisciplinary team of specialised practitioners who can demonstrate expertise and leadership in the core components. Two factors make programmes successful: the ability to recruit a large percentage of eligible patients to join and then complete the programme; and a programme that delivers what is required in the BACR Standards. The required health outcomes are then more likely to be achieved.
Creating a successful programme
Currently, the National Audit for Cardiac Rehabilitation (NACR) reports that fewer than 40% of eligible patients take up CR.5 There are model programmes throughout the UK, however, that do meet National Service Framework (NSF) targets of 85%.6 In my observations and discussions of these programmes there seem to be two key ingredients that lead to such success:
- A doctor specialising in cardiovascular disease who is an integral part of the CR team and who uses his/her influence not only clinically but in management and service delivery/funding issues and planning.
- A lead clinician who is experienced in cardiac care and service management and who has the initiative and ability to integrate many people, facilities and departments. This is all done with the aim of recruiting the highest proportion of eligible patients, by managing an information and communication system that encourages patients to recognise the value of the CR service as a key part of their cardiac care and hence the need for them to participate in the programme.
The final statement of the WHO definition highlights the importance of integrating with secondary prevention services. In the UK, this responsibility lies mainly with the GPs and local primary care teams. Therefore, there has to be good communication, with referral and re-referral systems in place between the CR team and the primary care services. Furthermore, many of the elements of the core rehabilitation components are also delivered by other teams within a given community or primary care service (exercise referral and physical activity leisure services, diet, weight management, counselling and mental health and smoking cessation services). Each CR team needs to think and plan carefully how it wishes to integrate with these services, either by incorporating them into their CR programme or as part of the BACR Component identified as long-term management. The recognition and integration of primary care through Quality and Outcomes Framework (QoF) standards is one of the key facets related to CR. With the development of service commissioning guides to be released by the Department of Health, the value of CR will be brought into much sharper focus.
References
1. Department of Health, The Coronary Heart Disease National Service Framework: Building on excellence, maintaining progress – Progress report for 2008. www.dh.gov.uk/en/Publicationsandstatistics/Publications
2. Jolliffe J, Rees K, Taylor RRS, Thompson DR, Oldridge N, Ebrahim S.
Exercise-based rehabilitation for coronary heart disease. Cochrane Database of Systematic Reviews, 2001, Issue 1. Art. No.: CD001800. DOI: 10.1002/14651858.CD001800
3. World Health Organization (WHO). In: National Institute for Health and Clinical Excellence. Secondary prevention in primary and secondary care following myocardial infarction. Clinical Guidelines CG 48. London: NICE, 2007. www.nice.org.uk/nicemedia/pdf/CG48FullGuideline.pdf
4. British Association for Cardiac Rehabilitation (2007); Standards and Core Components for Cardiac Rehabilitation. www.bcs.com
5. National Audit of Cardiac Rehabilitation. Annual Statistical Report 2009. www.cardiacrehabilitation.org.uk/nacr/docs/2009.pdf
6. Department of Health. Coronary
heart disease: National Service Framework for Coronary Heart Disease – modern standards and service models.
www.dh.gov.uk/prod_consum_dh/groups/dh_digitalassets/@dh/@en/documents/digitalasset/dh_4057526.pdf

