We developed and piloted an innovative family-centred preventive cardiology programme (MyAction) that aimed to both integrate the care of patients with vascular disease with that of individuals identified at high multi-factorial risk and help them achieve recommended lifestyle, medical risk factors and therapeutic targets. The 16-week nurse-led programme was delivered by a multi-disciplinary team, including a dietitian, physical activity specialist and cardiologist, in a community setting. Of 206 patients who attended the initial assessment, 54% attended with their partner and 142 patients completed the programme (69%). By the end of the programme, there was a significant improvement seen in adherence to a Mediterranean diet, as well as substantial increases in physical activity levels supported by objective evidence of improved functional capacity. These changes contributed to significant reductions in body mass index (BMI), weight and abdominal obesity. Very similar changes were seen in partners. Blood pressure control also improved significantly, as did achievement of the low-density lipoprotein (LDL)-cholesterol target, and there was a significant increase in the use of cardioprotective medication. Quality of life also improved in both patients and partners. The significant changes achieved by the MyAction preventive cardiology programme should substantially reduce the cardiovascular risk of these patients and their partners in the future.
Introduction

The Government white paper put ‘prevention first’ because there is strong evidence that a healthy lifestyle, control of other risk factors and cardioprotective medications can substantially reduce cardiovascular disease (CVD).1
Patient priorities for prevention are defined in the Joint British Societies’ Guidelines (JBS2): established vascular disease; asymptomatic high total risk of developing CVD (JBS2 CVD risk ≥20%); and these guidelines, together with the British Association for Cardiac Rehabilitation (BACR) standards, have defined quality care.2,3 Yet, preventive care for these patients is less than optimal.4
The National Audit of Cardiac Rehabilitation shows that only 38% of eligible coronary patients accessed rehabilitation programmes in 2009,5 and patients with exertional angina, the most common presentation of coronary artery disease,6 are not usually included, and nor are other patients with atherosclerotic disease. The new NHS Health Checks programme will result in many more individuals being identified at high multifactorial risk,1 so there is a pressing need for an effective, evidence-based preventive cardiology model for secondary and primary prevention.
We undertook the EUROACTION study, a cluster randomised-controlled trial of a preventive cardiology programme in hospital and primary care, across eight countries in Europe.7 One-year outcomes showed that a nurse-managed, multi-disciplinary, family approach, yielded significant lifestyle improvements and risk factor reductions for both coronary patients (COR), high-risk individuals (HRI) and partners (PR), compared with usual care.8
We developed the MyAction model for the National Health Service (NHS) by integrating the care of those with coronary disease with that of HRI in a community setting, all based on the principles of EUROACTION. The pilot programme was led by a cardiac specialist nurse (nurse prescriber), and the multi-disciplinary team (MDT) included a dietitian, a physical activity specialist and a visiting cardiologist. We set up the first MyAction programme in a public leisure centre in Bromley in partnership with Mytime Active, a leisure trust, and the primary care trust (PCT). This paper describes end of programme results.
Methods
COR were recruited from the Princess Royal Hospital: acute myocardial ischaemia (troponin negative) and stable angina (not eligible for the hospital cardiac rehabilitation programme). HRI were referred from local general practices.
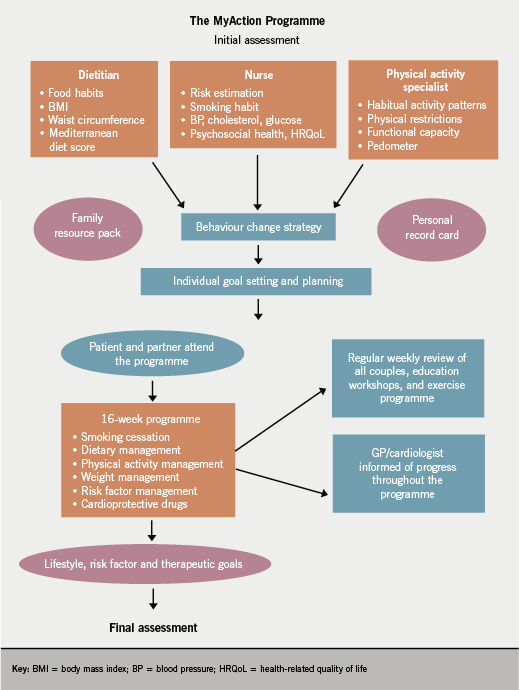
We developed a health professional manual (HPM) for lifestyle and risk factor assessment and management. At initial assessment (IA), patients and partners were seen as couples, but individually assessed by each MDT member for: smoking habit (breath CO); diet (diet history, food habit questionnaire and Mediterranean diet score9); weight and height, body mass index (BMI) and waist circumference; physical activity levels (seven-day physical activity recall) and functional capacity (Chester step test10); psychosocial measures (Dartmouth CO-OP, EuroQol EQVAS and Hospital Anxiety and Depression Scale [HADS]); blood pressure (BP), fasting lipids and glucose; and use of cardioprotective medications. This assessment identified the couple’s priorities and needs to reduce their cardiovascular risk, as well as exploring beliefs, barriers and motivators to change. Motivational interviewing and goal setting were used. The 16-week programme included individualised follow-up, a weekly educational workshop and supervised exercise session in which all members of the MDT took part. A weekly meeting between the MDT and cardiologist reviewed lifestyle, risk factor and therapeutic goals, and the nurse and cardiologist followed protocols (HPM) for risk factor management including medication as appropriate (figure 1).
After programme completion, the couple had an end of programme (EOP) assessment, which recorded the same data as at IA. Data were stored on a secure electronic database. The outcome measures reported are changes in proportions, between IA and EOP assessment, achieving lifestyle, risk factor and therapeutic targets.3
Statistical analysis
Variables are summarised at IA and EOP using means and standard deviations (SDs) for quantitative measurements, and percentages for binary variables are used. The t-test (or Mann-Whitney test) is used for quantitative measurements to compare those who attended EOP with those who did not. The chi-square test (or Fisher’s exact test) is used for comparison of proportions.
Comparisons of those who had both IA and EOP measurements were made using the paired t-test, Wilcoxon signed-rank test for nonsymmetric distributions and McNemar’s test for paired proportions. Confidence intervals (CIs) for differences in means or proportions were calculated. All significance tests were performed at the 5% level with no adjustment for multiple testing.
Results
Referrals
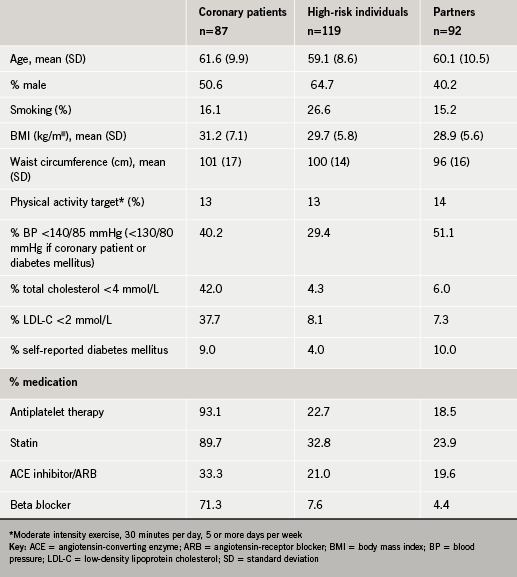
There were 306 patients (142 COR and 164 HRI) referred to the programme, all of whom were invited to attend an IA. Of these 87 (61%) of COR and 119 (73%) HRI attended: 93 partners (PR) (54% of those with a partner) also attended.
Assessments
Baseline characteristics of patients and partners at IA are shown in table 1. Twenty-two per cent of partners already had a history of either CVD or diabetes mellitus, and a further 21% were subsequently found to have a CVD risk score ≥20% at their initial assessment. Of those who attended IA, 70% (and 63% of partners) attended for an EOP assessment. Those who did not return at EOP were significantly younger (HRI) and more obese (COR) compared with EOP attendees.
Lifestyle
At IA, 20 patients were current smokers, of whom five (25%) had stopped by EOP (self-reported and CO <6 ppm). Table 2 shows changes between initial and EOP assessment for COR, HRI and PR. Adherence to the Mediterranean diet significantly improved in all three groups. In those overweight at baseline (BMI ≥25 kg/m2), there were significant reductions in mean weight in all three groups, and significant reductions in abdominal obesity in HRI and PRs. At IA, only one fifth of patients and partners were achieving the physical activity target of 30 minutes of moderate intensity aerobic activity five or more times a week, but by EOP, the proportions achieving this target had increased substantially in all three groups. There was also evidence of improved cardiorespiratory fitness with a significant increase in seconds achieved (between 70 and 77 seconds) in the Chester step test in all groups.
Health-related quality of life (HRQoL), as measured by the EQ-VAS and the total Dartmouth CO-OP score, both significantly improved in each patient group and EQVAS alone improved in partners. Significant reductions were also seen in anxiety scores in COR, and in depression scores for both COR and HRI.
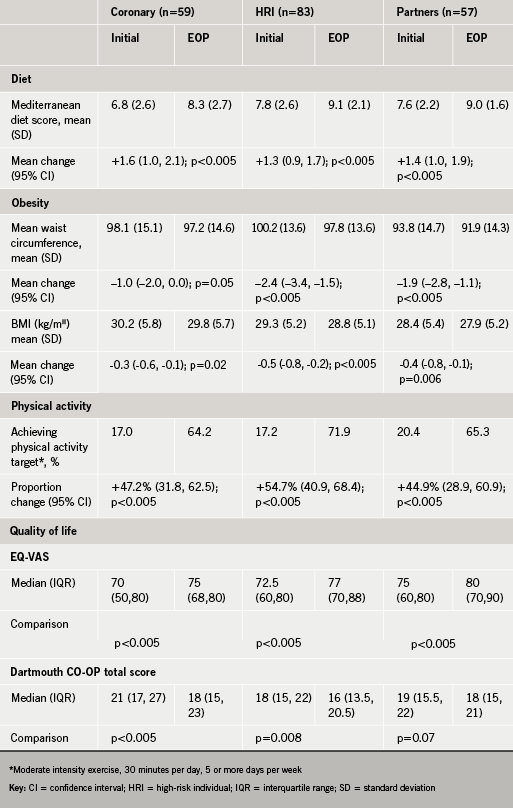
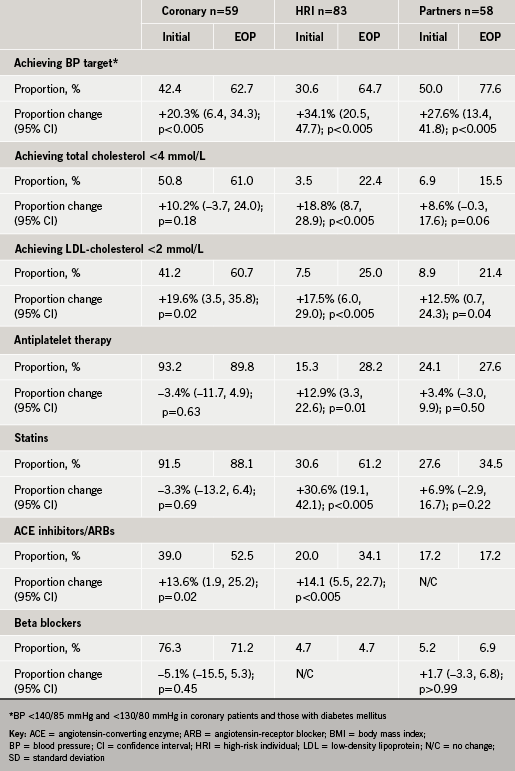
Table 3 shows the results for medical risk factors and cardioprotective drugs. There was a significant increase in proportions achieving the BP target in all three groups. There were also significant increases in proportions achieving the total and low-density lipoprotein (LDL)-cholesterol targets; the latter was statistically significant in all three groups. A fasting blood glucose (FBG) was measured in all patients and partners at IA (target ≤6 mmol/L) and glycosylated haemoglobin (HbA1c) was measured in those with known diabetes or newly diagnosed diabetes (FBG >7 mmol/L on two occasions). Only one COR and one HRI were diagnosed with new diabetes at IA. For cardioprotective medication, there was a significant increase in prescription of angiotensin-converting enzyme (ACE) inhibitor/angiotensin-receptor blockers (ARBs) in COR patients; and, in HRI, significant increases in antiplatelet therapy, statins, ACE inhibitors/ARBs and calcium channel blockers occurred.
Discussion
The MyAction programme offers an innovative approach to secondary and primary prevention in the community. It successfully recruited and retained the majority of patients referred, together with their partners. There was a significant improvement seen in adherence to a Mediterranean diet, as well as substantial increases in physical activity levels supported by objective evidence of improved functional capacity. These changes contributed to significant reductions in BMI, weight and abdominal obesity.
BP control also improved significantly as did achievement of the LDL-cholesterol target. The use of medication in COR was high at IA, but there was also a significant increase in the use of ACE inhibitors/ARBs in both COR and HRI, and statins and calcium channel blockers in HRI alone. Interestingly, although there was no significant increase in medication use in partners, this group also had significant reductions in BP and cholesterol levels, possibly consequent on healthier lifestyle changes. Quality of life also improved in both patients and partners.
The scientific evidence from randomised controlled trials for cardiac rehabilitation and secondary prevention programmes is compelling.11,12 However, in the UK only about a third of coronary patients are accessing such a programme.5 Furthermore, restricting programmes to those who have had surgery or myocardial infarction misses the majority of coronary patients, as the most common presentation is with angina. Moreover, only a minority of cardiac rehabilitation programmes meet the BACR standards in terms of a dedicated MDT, and few provide a comprehensive approach to cardiovascular prevention, the main emphasis being on exercise and physical activity.13 Patients with other forms of atherosclerosis such as transient ischaemic attack (TIA) or peripheral arterial disease, rarely access such programmes, despite having the same disease.
In contrast, the MyAction programme is open to all patients with any presentation of coronary artery disease, or other atherosclerotic disease, and importantly MyAction meets the BACR standards in terms of staffing and also provides all the core components.2
The new NHS Health Checks programme in England will identify those at high total risk of developing CVD.1 Many PCTs are using health trainers to deliver a brief lifestyle intervention and signpost patients to existing local services, including smoking cessation, weight loss programmes and exercise referral schemes. However, there is no evidence that either health trainers or signposting will improve lifestyle and risk factor outcomes.14 In contrast, the MyAction programme provides comprehensive preventive care under one roof for all high-risk patients. Although the meta-analysis of randomised-controlled trials of multi-factorial programmes in primary prevention found no significant effect on total or coronary mortality, a small and potentially important 10% reduction in coronary heart disease (CHD) mortality may have been missed,15 and this apparent lack of effect reflects a modest reduction in smoking and small changes in BP and lipids, the latter due to limited drug treatment in these trials. In contrast, single risk factor trials using drug therapies to lower BP or lipids have shown comparable reductions in CVD risk as predicted by epidemiological relationships.16,17 This pilot of the MyAction programme, like the EUROACTION trial, achieved healthy lifestyle changes, but also significant improvements in the therapeutic control of BP and lipids commensurate with those achieved in the single risk factor trials.
Thus, it is reasonable to postulate that MyAction will substantially reduce total cardiovascular risk in coronary and high-risk patients and their families.
The inclusion of family is important as risk factors for heart disease cluster in families due to shared lifestyles, and there is good evidence that healthy lifestyle change is more likely to occur if the family changes together.18,19 This is supported by the results for partners in the MyAction programme which matched, for the most part, those of the patients.
Study limitations
This is a descriptive study with no control group and, therefore, the results may be due to regression to the mean, not necessarily the effect of MyAction. In addition, not all those who attended IA came back for the EOP assessment, and they had some different characteristics, which is a potential source of bias. However, the statistical analyses presented are based only on those individuals who attended both IA and EOP assessment. Another limitation is the patient population, which was principally white British and from a relatively affluent area in Southeast London. So the MyAction model needs to be validated in different ethnic groups and across all socio-economic strata. This is now taking place in four programmes in NHS Westminster. The lifestyle and risk factor changes described occurred over a short time period (about four months), and it is recognised that such changes may be difficult to maintain over the longer term, although in the EUROACTION trial the same benefits were still evident at one year.8
A MyAction programme is now also being initiated by NHS Heart of Birmingham and more are planned for other parts of the UK. With Westminister, these other programmes will form part of a national demonstration project, which aims to model the cost-effectiveness of the MyAction lifestyle and risk factor outcomes at one year. This will contribute to ongoing evaluation of what is best value for money for prevention in the NHS.
Acknowledgements
We would like to thank. Mike Galvin (Referral Co-ordinator), Dr Ed Langford (Consultant Cardiologist, Princess Royal Hospital, Farnborough), Dr Nada Lemic (Director of Public Health, Bromley PCT), Michaela Nuttall (CHD Coordinator, Bromley PCT), Mr Steve Price (CEO Mytime Active), Angie Sutcliffe (Acute Coronary Syndrome Nurse, Princess Royal Hospital), Clare Schaar (Rapid Access Medical Clinic Nurse, Princess Royal Hospital), Dr Ray Vella (GP CHD Lead, Bromley PCT), and all the general practitioners in Bromley PCT who referred the patients with their families to the programme.
Conflict of interest
The MyAction pilot was funded by an unrestricted educational grant from AstraZeneca UK. SC has received speaker’s honoraria from Merck, Pfizer, AstraZeneca and Abbott Healthcare. AH, ET, GF, JS, MH, AM, KK, CJ, JJ, DAW: none declared.
Key messages
- The MyAction preventive cardiology programme is designed to integrate the care of patients with vascular disease with individuals at high multi-factorial risk (JBS2 ≥20%) in a community setting
- The 16-week programme is family-centred and delivered by a nurse-led multi-disciplinary team. The foundation of the programme is healthy lifestyle change, management of medical risk factors and prescription of appropriate cardioprotective medication
- The results from this pilot in Bromley suggest that the programme was successful in recruiting and retaining the majority of the patients referred, as well as their families, with significant changes achieved in terms of lifestyle, medical risk factors and use of appropriate medication
References
- Department of Health. Putting prevention first. Vascular checks: risk assessment and management. London: DoH, 2008.
- British Association for Cardiac Rehabilitation. Standards and core components for cardiac rehabilitation. London: BACR, 2007.
- Joint British Societies. JBS2: Joint British Societies’ guidelines on prevention of cardiovascular disease in clinical practice. Heart 2009;91(suppl V).
- Kotseva K, Wood D, De BG, De BD, Pyorala K, Keil U. EUROASPIRE III: a survey on the lifestyle, risk factors and use of cardioprotective drug therapies in coronary patients from 22 European countries. Eur J Cardiovasc Prev Rehabil 2009;16:121–37.
- British Heart Foundation. The national audit of cardiac rehabilitation. Annual statistical report 2009. Available from: http://www.cardiacrehabilitation.org.uk/docs/2009.pdf
- Sutcliffe SJ, Fox KF, Wood DA et al. Incidence of coronary heart disease in a health authority in London: review of a community register. BMJ 2003;326:20.
- Wood DA. EUROACTION: A European Society of Cardiology demonstration project in preventive cardiology. Kotseva K, Jennings C, Mead A et al., editors. A cluster randomized controlled trial of a multi-disciplinary preventive cardiology programme for coronary patients, asymptomatic high risk individuals and their families. Summary of design, methodology and outcomes. Eur Heart J 2005;6(suppl J):J3–J15.
- Wood DA, Kotseva K, Connolly S et al. Nurse-coordinated multidisciplinary, family-based cardiovascular disease prevention programme (EUROACTION) for patients with coronary heart disease and asymptomatic individuals at high risk of cardiovascular disease: a paired, cluster-randomised controlled trial. Lancet 2008;371:1999–2012.
- Estruch R, Martinez-Gonzalez MA, Corella D et al. Effects of a Mediterranean-style diet on cardiovascular risk factors: a randomized trial. Ann Intern Med 2006;145:1–11.
- Sykes K. Chester step test; resource pack (Version 3). Cheshire, UK: Chester College of Higher Education, 1998.
- Clark AM, Hartling L, Vandermeer B, McAlister FA. Meta-analysis: secondary prevention programs for patients with coronary artery disease. Ann Intern Med 2005;143:659–72.
- Taylor RS, Brown A, Ebrahim S et al. Exercise-based rehabilitation for patients with coronary heart disease: systematic review and meta-analysis of randomized controlled trials. Am J Med 2004;116:682–92.
- Brodie D, Bethell H, Breen S. Cardiac rehabilitation in England: a detailed national survey. Eur J Cardiovasc Prev Rehabil 2006;13:122–8.
- Kinmonth AL, Wareham NJ, Hardeman W et al. Efficacy of a theory-based behavioural intervention to increase physical activity in an at-risk group in primary care (ProActive UK): a randomised trial. Lancet 2008;371:41–8.
- Ebrahim S, Beswick A, Burke M, Davey SG. Multiple risk factor interventions for primary prevention of coronary heart disease. Cochrane Database Syst Rev 2006;(4):CD001561.
- Baigent C, Keech A, Kearney PM et al. Efficacy and safety of cholesterol-lowering treatment: prospective meta-analysis of data from 90,056 participants in 14 randomised trials of statins. Lancet 2005;366:1267–78.
- Law MR, Morris JK, Wald NJ. Use of blood pressure lowering drugs in the prevention of cardiovascular disease: meta-analysis of 147 randomised trials in the context of expectations from prospective epidemiological studies. BMJ 2009;338:b1665.
- Pyke SD, Wood DA, Kinmonth AL, Thompson SG. Change in coronary risk and coronary risk factor levels in couples following lifestyle intervention. The British Family Heart Study. Arch Fam Med 1997;6:354–60.
- Wood DA, Roberts TL, Campbell M. Women married to men with myocardial infarction are at increased risk of coronary heart disease. J Cardiovasc Risk 1997;4:7–11.
