This case describes the unfortunate consequence of hepatic abscess, initially discovered following abnormal liver function tests.
Case report
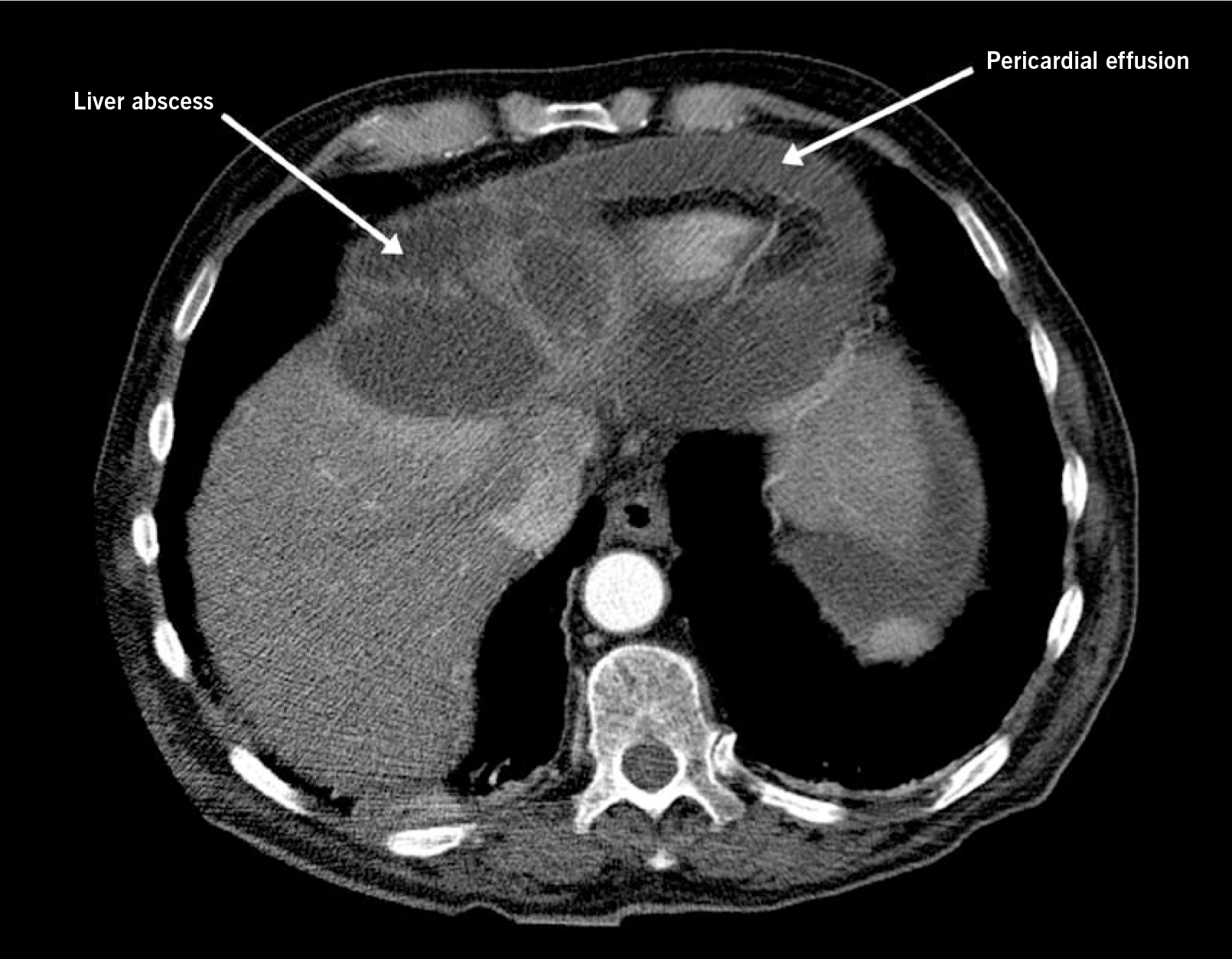
A 76-year-old diabetic male presented with a three-day history of central chest pain and breathlessness. Liver ultrasound performed two months previously due to abnormal liver function tests had shown two cysts but no action was taken. On examination, he looked unwell with a raised venous pressure. Computed tomography (CT) scan showed a 2 cm pericardial effusion and a large multi-locular cyst 12 cm x 9 cm arising from the left lobe of the liver and extending to the base of the heart (figure 1).
Half-an-hour later, the patient went into tamponade and a pericardial drain was inserted. Over a fortnight, a total of 2.5 litres were drained from the pericardium and liver. Pericardial fluid cultured Proteus mirabilis and Enterococcus.
The patient was treated with two weeks of intravenous ciprofloxacin, amoxicillin and metronidazole.
Two weeks later he clinically deteriorated, with signs of constrictive pericarditis. He underwent a pericardectomy with drainage of pericardial and pleural effusions. Despite initial improvement, the patient died 14 hours post-operatively.
Conflict of interest
None declared.
