Several imaging modalities are available for the optimal management of patients with cardiovascular disease. When assessing any imaging technique, the radiation dose must be considered along with the value of the imaging technique. In this article, we summarise the radiation doses associated with cardiovascular imaging techniques, such as heart catheterisation, nuclear medicine and multi-slice computed tomography. The effective dose of the dual isotope scan, an image modality frequently used in cardiac patients, is higher (~25 mSv) than cardiac computed tomography (~10 mSv) or diagnostic heart catheterisation (~5 mSv). The physician should weigh carefully which test to recommend in each patient.
Introduction
Several imaging modalities are available for the optimal management of patients with cardiovascular disease. When assessing any imaging technique, the radiation dose must be considered along with the value of the imaging technique. Coronary artery evaluation using multi-slice computed tomography (MSCT) was introduced recently, and this imaging modality is expected by some to become a major new player in the field of cardiac imaging. We hereby summarise the radiation doses associated with MSCT and other currently available cardiovascular imaging techniques.
Ionising radiation in medicine
The benefit to patients from the medical use of radiation has been established beyond doubt.1-3 Modern diagnostic imaging assures faster, more precise diagnosis, enables monitoring of a large proportion of diseases and, in cases of interventional cardiology, also allows therapy. Frequently, radiological procedures have a substantial impact on the speed of diagnosis and are decisive in clinical management.2,4
The most common types of ionising radiation used in medicine are X-rays, gamma-rays, beta-rays and electrons.4-11 Ionising radiation is only one part of the electromagnetic spectrum. There are numerous other types of radiation (e.g. visible light, infrared waves, ultrasound, high frequency and radiofrequency electromagnetic waves) that do not possess the ability to ionise atoms of the absorbing matter.
Radiation terms
Absorbed versus effective dose
Some ionising radiation will pass through the body without any interaction and with no biological effect. The radiation that is absorbed may be hazardous. The frequency or intensity of the biological effects and the probability of chromosomal damage is proportional to the radiation dose and is dependent upon the total energy of radiation absorbed per unit mass of a sensitive tissue or organ. This quantity is called absorbed dose and is expressed in gray (Gy) units. Absorbed doses of radiation can be indirectly calculated by measuring radiation exposure, and they form the basis for evaluation of the probability of radiation-induced effects.2
The sievert (Sv) is an SI unit used for measuring the effective (or ‘equivalent’) dose of radiation received by a living organism. The unit honours the Swedish physicist, Rolf Sievert (1898–1966), who worked for many years on measuring and standardising radiation doses used in cancer treatment.
1 Sv = 1 J/kg = 1 m2s–2
Various types of radiation have different effects on living tissue, so a simple measurement of the dose as energy received, stated in Gy or rad, does not give a clear indication of the probable biological effects of the radiation. The equivalent dose in Sv is equal to the actual dose in Gy, multiplied by a ‘quality factor’, which is larger for more dangerous forms of radiation. An effective dose of 1 Sv requires 1 Gy of beta or gamma radiation, but only 0.05 Gy of alpha radiation or 0.1 Gy of neutron radiation. One Sv is equal to 100 rem (Roentgen equivalent man). The Sv is a large unit, so radiation doses are often measured in millisieverts (mSv).
The effective dose allows for quantification of risk and comparison with more familiar sources of exposure that range from natural background radiation to radiographic medical procedures. The effective dose is not applicable to radiation therapy used to treat cancer patients, where very large absorbed doses affect individual tissues or organs.
Natural background radiation
Radiation from natural sources is present at all times. The natural background effective dose rate varies considerably from place to place, but typically is about 3.5 mSv/year (2.2 mSv in the UK).2 Altitude plays a significant role, and those living in the mountains receive about 1.5 mSv more per year than those living near sea level. The added dose from cosmic rays during a coast-to-coast round-trip flight in a commercial aeroplane is about 0.03 mSv.3 One chest X-ray has an effective radiation dose of 0.02 mSv, i.e. the radiation from one chest X-ray is equivalent to the amount of radiation exposure one experiences from natural surroundings in three days.
Hazards of radiation
Ionising radiation can disrupt DNA in the cell, causing mutations, some of which are not repaired or not repaired correctly. This may form the first step of carcinogenesis, which requires several subsequent mutations (most likely not induced by radiation) in the affected cells.1
Radiation threshold
The biological effects are of two kinds.1-3 The first are those that occur only after a dose threshold has been exceeded, known as ‘deterministic’ effects. Radiation doses that exceed a minimum (threshold) level can cause effects such as depression of the blood cell-forming process (threshold dose = 500 mSv) or cataracts (threshold dose = 5,000 mSv). The scope and severity of these effects increases as the dose increases above the corresponding threshold. The second are those that can occur at any dose with no threshold but with a probability proportional to the dose. These are known as ‘stochastic’ effects (i.e. probabilistic effects, all or none).
For radiation protection purposes, it is assumed that any dose above zero can increase the risk of radiation-induced cancer, i.e. there is no threshold. Epidemiological studies have found that the estimated lifetime risk of dying from cancer increases by about 0.004–0.008% per mSv of radiation dose to the whole body.10,11 For a full-body equivalent dose, 1 Sv causes slight blood changes, 2–5 Sv causes nausea, hair loss, and haemorrhage, and will cause death in many cases. More than 6 Sv will lead to death in less than two months in more than 80% of cases. Most cardiovascular imaging modalities are associated with around 10 mSv.
Clinical decision-making
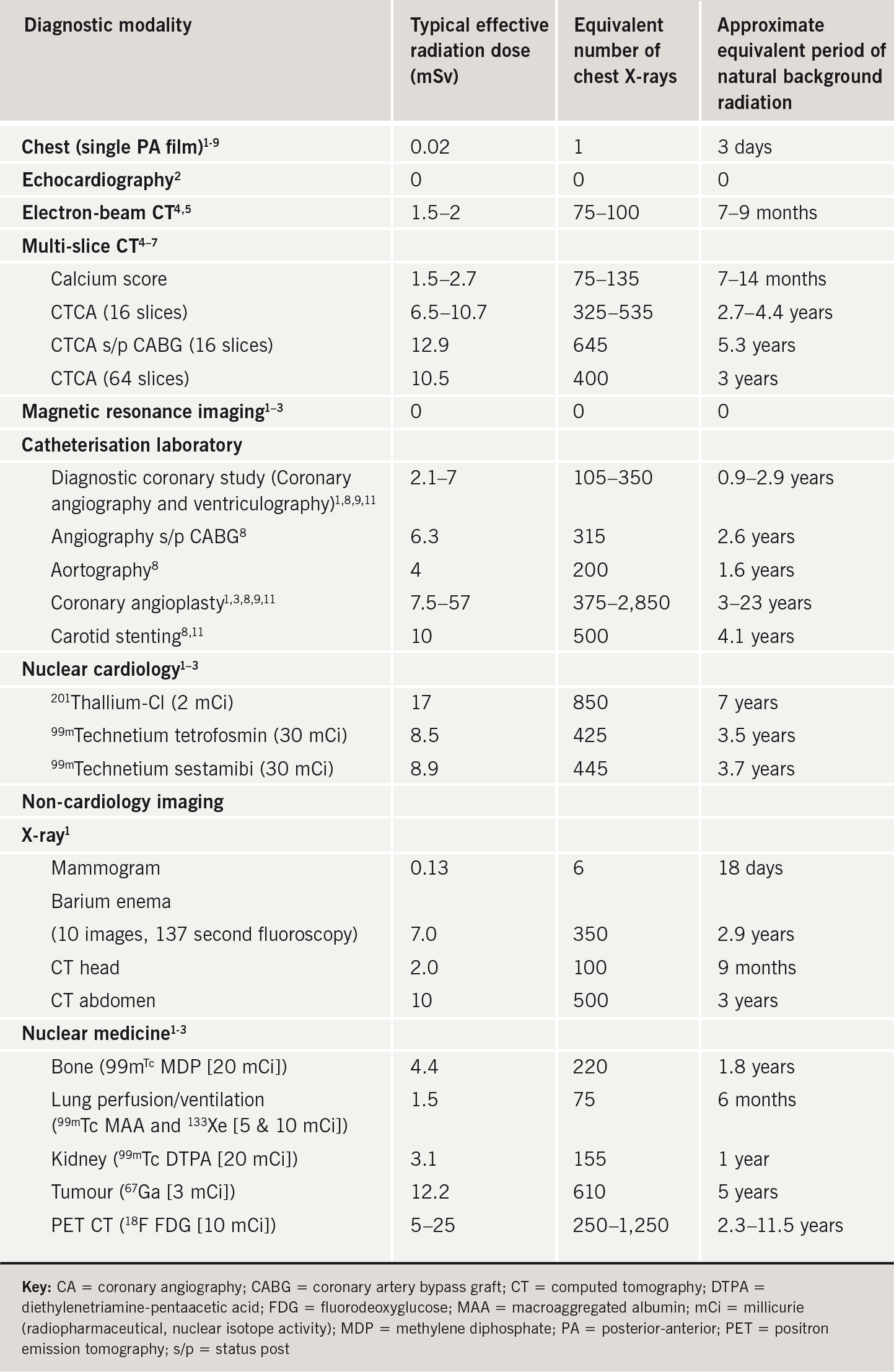
The cardiologist needs to weigh the advantages and risks of every imaging modality. The patient’s clinical characteristics and the likelihood for cardiovascular disease should be considered carefully, and each patient’s management should be tailored. Table 1 compares effective radiation doses with background radiation exposure and the equivalent number of chest X-rays for several imaging modalities frequently used in cardiology and general medicine. The calculated dose estimates originate from various papers and were obtained in a heterogeneous patient population at different institutes with a variety of equipment.
Imaging modalities
MSCT, the new imaging modality for non-invasive visualisation of the coronary arteries, is still in its early phases of clinical evaluation The newer CT scanners have improved rotation. speed and are capable of performing several rotations in a second. Scans are usually gated to the ECG trace. Frequently, a test image is taken to determine the location of the heart and the best scan settings, following which a scan for the calcium score can be performed. Of note, diabetic patients have a higher likelihood of coronary calcification, rendering MSCT coronary angiography less likely to be conclusive in
some cases.
CT angiography is obtained using an injection of 80–120 cc dye. Data acquisition takes 5–25 seconds, during which a breath-hold is required. Image reconstruction takes place at a later time point. The medical community is investigating the place of MSCT in the cardiovascular imaging arsenal. Both the 16-slice and 64-slice CT scanners are associated with substantial ionising radiation doses (6.5-10.5mSv). Nevertheless, this dose is favourably comparable to other frequently used, non-invasive procedures, such as myocardial nuclear imaging scans (table 1).
Of note, treadmill stress tests and nuclear scans provide functional data while angiography and MSCT angiography provide anatomical data. Nuclear scans and MSCT
are non-invasive and allow only diagnosis, with no therapeutic options. Heart catheterisation is an invasive diagnostic procedure that has the advantage of also being therapeutic. The diagnostic portion of this imaging modality has a lower radiation exposure than current non-invasive diagnostic imaging modalities, such as a nuclear stress test and MSCT.4-9
In general, coronary interventions use more radiation, depending on the complexity and length of the procedure. Invasive angiography may cause deterministic radiation effects (e.g. erythema, hair loss, skin ulcers) in very rare cases.12,13 Yet, such procedures improve symptoms and may also be lifesaving and, thus, the risks associated with the radiation are usually of secondary consideration. There are also non-radiation risks associated with the investigations, such as allergy due to contrast agents and the fact that false positive results may lead to additional tests.
Case history
A 52-year-old man with cardiac risk factors of hypertension, type 2 diabetes, hypertriglyceridaemia, low high-density lipoprotein (HDL), obesity, positive family history of early coronary artery disease,
and atypical anginal symptoms was referred for cardiovascular evaluation. Treadmill stress test was not conclusive, as he did not reach his target heart rate. Echocardiography was normal. He was referred for a dipyridamole dual isotope nuclear stress test, which showed lateral wall reversible ischaemia. Coronary angiography was recommended. The patient was concerned and anxious, and elected to undergo MSCT angiography, which revealed an elevated calcium score and significant coronary narrowing in the left circumflex and right coronary arteries. Coronary angiography had similar findings and the lesions were treated with stents.
Radiation exposure in our patient
Our patient underwent echocardiography that uses ultrasound energy and has no ionising radiation. Echocardiography allows estimation of heart and valve function but not of the coronary arteries. The same is true for cardiac magnetic resonance imaging (MRI), although it is much more expensive.
As he did not complete his treadmill stress test (no radiation), a pharmacological stress test was used. A dobutamine echocardiography stress test has no radiation and is excellent for this purpose, but a nuclear scan was ordered and, based on the results of this test, the patient’s history, medical therapy and risk profile, a coronary angiography was ordered. However, our patient and his wife were still very worried and hesitant about the need for an interventional procedure. After being exposed to the debate in the media concerning computed tomography (CT) in cardiology, our patient referred himself to MSCT angiography.
In the cardiovascular evaluation of our patient, he was exposed to the following ionising radiation: treadmill stress test (0 mSv), echocardiography (0 mSv), dipyridamole nuclear stress test (thallium + technetium; 25 mSv), calcium score (2 mSv), MSCT angiography (10 mSv) and diagnostic coronary angiography (5 mSv), for a total of about 42 mSv. This is equivalent to 2,100 chest X-rays or the approximate equivalent period of natural background radiation of 17 years. The percutaneous intervention was not complex and was associated with approximately an additional 15 mSv of ionising radiation. If we follow this patient with a dual isotope cardiovascular nuclear scan (25 mSv), he will be exposed to an equivalent of approximately 1,250 chest X-rays every time he has the test.
Summary
The physician’s judgment is crucial in the face of diverse clinical presentations and varying patient characteristics. The physician’s aim is to improve patient care and health outcome, not only in a cost-effective manner, but also with the safe use of available technology.
Although ionising radiation is hazardous, the risk of radiation exposure is usually not a major concern when placed in the context of the information obtained and the benefits of the procedure. Since the risk for such a complication depends on individual circumstances, the physician should carefully weigh which test should be recommended for each patient and discuss the options with the patient.
Clinical decision-making should take into account the radiation doses of the investigations. However, the key is not the dose of the investigation requested but whether it is appropriate to the actual question being asked.
Conflict of interest
None declared.
Key messages
- Several imaging modalities are available for the optimal management of patients with cardiovascular disease
- When assessing any imaging technique, radiation dose must be considered along with the value of the imaging technique
- The physician should carefully weigh which test to recommend and discuss the possibilities with the patient
- The effective dose of a dual isotope scan, an image modality frequently used in cardiac patients, is higher (~25 mSv) than cardiac computed tomography (~10 mSv) or diagnostic heart catheterisation (~5 mSv)
References
- Mettler FA. An evaluation of radiation exposure guidance for military operations. In: Johnson JC, Thaul S (eds). Report by a committee of the Institute of Medicine, Medical Follow-up Agency, National Academy of Sciences. Washington DC: National Academy Press, 1997.
- Vetter RJ. Medical health physics: a review. Health Phys 2005;88:
653–64. - United Nations Scientific Committee on the Effects of Atomic Radiation. Sources and effects of ionizing radiation, Vol. 1: Sources. New York NY: United Nations Publishing, 2000.
- Hunold P, Vogt FM, Schmermund A et al. Radiation exposure during cardiac CT: effective doses at multi-detector row CT and electron-beam CT. Radiology 2003;226:145–52.
- Hausleiter J, Meyer TS, Hadamitzky M, Martinoff S, Schoemig A. Effective radiation dose of cardiac computer tomography angiography. A comparison between 64- and 16-slice technology. Eur Heart J 2005;26(suppl 1):Abstract 3155.
- Deetjen A, Moellmann S, Conradi G et al. Multislice computed tomography of the coronaries: intraindividual comparison of radiation dose exposure with conventional coronary angiography. Eur Heart J 2005;26(suppl 1):Abstract 2749.
- Trabold T, Buchgeister M, Kuttner A et al. Estimation of radiation exposure in 16-detector row computed tomography of the heart with retrospective ECG-gating. Rofo 2003;175:1051–5.
- Cioppa A, Picano V, Ambrosini G et al. Radiation dose exposure during cardiac catheterization. Eur Heart J 2005;26(suppl 1):Abstract 2925.
- Efstathopoulos EP, Karvouni E, Kottou S et al. Patient dosimetry during coronary interventions: a comprehensive analysis. Am Heart J 2004;147:468–75.
- Hendee WR. Estimation of radiation risks. BEIR V and its significance for medicine. JAMA 1992;268:620–4.
- Vano E, Gonzalez L, Guibelalde E et al. Evaluation of risk of deterministic effects in fluoroscopically guided procedures. Radiat Prot Dosimetry 2006;117:190–4.
- Koenig TR, Mettler FA, Wagner LK. Skin injuries from fluoroscopically guided procedures: part 2, review of 73 cases and recommendations for minimizing dose delivered to patient. AJR Am J Roentgenol 2001;177:13–20.
- Vlietstra RE, Wagner LK, Koenig T, Mettler F. Radiation burns as a severe complication of fluoroscopically guided cardiological interventions. J Interv Cardiol 2004;17:131–42.
