We present a case in which the use of cardiovascular magnetic resonance (CMR) allowed the full pathology underlying syncope to be established.
Case report
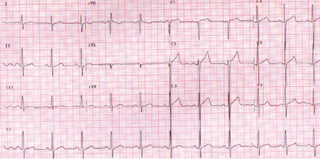
A 67-year-old man was referred to the cardiology clinic with a history of collapse and a family history of hypertrophic cardiomyopathy (HCM). He denied any history of angina or dyspnoea. On physical examination he had a 3/6 grade ejection murmur in the aortic area and a pansystolic murmur at the mitral area accentuated on squatting. There were no signs of volume overload. X-ray angiography demonstrated normal coronaries but a raised end diastolic pressure. His electrocardiogram (ECG) was compatible with left ventricular (LV) hypertrophy (figure 1). A single Holter recording was performed following the index presentation – no ventricular arrhythmia was identified. Echocardiography demonstrated LV concentric hypertrophy with systolic anterior motion of the mitral valve, left ventricular outflow tract (LVOT) obstruction (gradient of 70 mmHg) and mild mitral regurgitation.
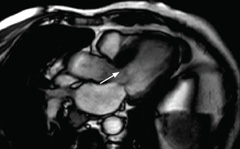
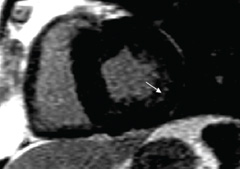
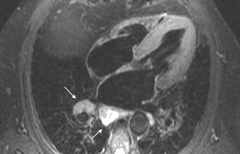
A cardiovascular magnetic resonance (CMR) scan was performed demonstrating asymmetric rather than concentric LV wall thickening with a basal septal wall thickness of 23 mm compared to a lateral wall of 9 mm at the same level. LV cavity dimensions were small. There was hyperdynamic systolic function with near complete cavity obliteration in end systole at the apex. Systolic anterior motion and LVOT obstruction were confirmed (figure 2). On spin echo images, there was no evidence of myocardial active inflammation. Following administration of the contrast agent Gadolinium, on late images there was patchy mid-wall enhancement in the anteroseptal and inferior walls typical of fibrosis (figure 3).
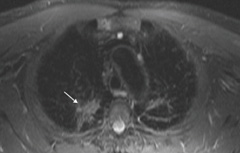
Unexpectedly, there was also extensive mediastinal lymphadenopathy and parenchymal changes in the upper lobes of both lungs (figures 4 and 5). There was evidence of an active inflammatory process in the lymph nodes. Subsequent lymph node biopsy confirmed the presence of sarcoidosis. No evidence for cardiac involvement in this case was identified by CMR or on subsequent follow-up. The ECG findings are uncommon for obstructive HCM. However, the patient had a strong family history of HCM with several affected family members that would support the likelihood of his carrying the genotype. Predominant cardiac pathology is HCM rather than sarcoidosis.
Conclusion
The CMR findings are of HCM in addition to concurrent pulmonary sarcoidosis. This case demonstrates the value of CMR in first identifying potential aetiologies for patients presenting with syncope and second, its role in tissue characterisation, particularly where there may be dual pathology •
Conflict of interest
None declared.
Further reading
- Moon JC, Prasad SK. Cardiovascular magnetic resonance and the evaluation of heart failure. Curr Cardiol Rep 2005;7:39–44.
- Smedema JP, Tadamura E. Previous studies on delayed enhanced MRI for the detection of cardiac sarcoidosis. Am J Roentgenol 2006;186:578.
- Smedema JP, Snoep G, van Kroonenburgh MPG et al. Evaluation of the accuracy of Gadolinium-enhanced cardiovascular magnetic resonance in the diagnosis of cardiac sarcoidosis. J Am Coll Cardiol 2005;45: 1683–90.
